Generation M – by Dr. Jessica Shepherd
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Menopause is something that very few people are adequately prepared for despite its predictability, and also something that very many people then neglect to take seriously enough.
Dr. Shepherd encourages a more proactive approach throughout all stages of menopause and beyond; she discusses “the preseason, the main event, and the after-party” (perimenopause, menopause, and postmenopause), which is important, because typically people take up an interest in perimenopause, are treating it like a marathon by menopause, and when it comes to postmenopause, it’s easy to think “well, that’s behind me now”, and it’s not, because untreated menopause will continue to have (mostly deleterious) cumulative effects until death.
As for HRT, there’s a chapter on that of course, going into quite some detail. There is also plenty of attention given to popular concerns such as managing weight changes and libido changes, as well as oft-neglected topics such as brain changes, as well as things considered more cosmetic but that can have a big impact on mental health, such as skin and hair.
The style throughout is pop-science; friendly without skimping on detail and including plenty of good science.
Bottom line: if you’d like a fairly comprehensive overview of the changes that occur from perimenopause all the way to menopause and well beyond, then this is a great book for that.
Click here to check out Generation M, and live well at every stage of life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Nature Provides Us With A Surprisingly Powerful Painkiller
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s well-known (at least to regular 10almonds-readers) that seeing nature, ideally green leaves and blue sky, improves our mood by stimulating production of serotonin.
See also: Neurotransmitter Cheatsheet
But it does a lot more.
Reducing the actual signals of pain
Researchers at the University of Vienna have discovered that viewing nature scenes (even if just on video) alleviates physical pain—not just in self-reported subjective assessments, but also by a reduction of the neural activity that signals pain:
❝Pain is like a puzzle, made up of different pieces that are processed differently in the brain. Some pieces of the puzzle relate to our emotional response to pain, such as how unpleasant we find it. Other pieces correspond to the physical signals underlying the painful experience, such as its location in the body and its intensity.
Unlike placebos, which usually change our emotional response to pain, viewing nature changed how the brain processed early, raw sensory signals of pain.
Thus, the effect appears to be less influenced by participants’ expectations, and more by changes in the underlying pain signals❞
This was tested against, varyingly, viewing an urban environment or viewing an indoor environment, neither of which gave the same benefits.
The setup of the experiment is relevant, so…
Matching soundscape accompanied each visual stimulus. The three pain runs had a total duration of 9 min each, during which one environment was accompanied by 16 painful and 16 non-painful shocks. Neuroimaging was used for all parts, and participants were exposed to all environments:
- First, a cue indicating the intensity of the next shock (red = painful, yellow = not painful) was presented for 2000 milliseconds (ms).
- Second, a variable interval of 3500 ± 1500 ms was shown.
- Third, a cue indicating the intensity of the shock was presented for 1000 ms, accompanied by an electrical shock with a duration of 500 ms.
- Fourth, a variable interval of 3500 ± 1500 ms followed.
- Fifth, after each third trial, participants rated the shock’s intensity and unpleasantness at 6000 ms each.
- Sixth, each trial ended with an intertrial interval (ITI) presented for 2000 ms.
They found that as well as the self-assessment reports being as expected (nature scenes reduced subjective experience of pain),
❝In summary, the multivoxel and region of interest analyses converged in showing that pain responses when exposed to nature as compared to urban or indoor stimuli were associated with a decrease in neural processes related to lower-level nociception-related features (NPS, thalamus), as well as in regions of descending modulatory circuitry associated with attentional alterations of pain that also encode sensory-discriminative aspects (S2, pINS).❞
In other words—to the extent that pain can be quantified objectively by neural imaging—the pain was also objectively reduced, much like with a chemical painkiller.
You can read the paper in full, here:
Nature exposure induces analgesic effects by acting on nociception-related neural processing
How to benefit from this
Well, first there is the obvious, “view nature“.
However, note the timescales involved in the testing periods: 2000 milliseconds is two seconds, and that was the intertrial interval used—the equivalent of a washout phase in an interventional trial (but a drug/supplement/diet washout is usually a number of weeks).
The fact that the test periods were a matter of seconds, and the intertrial period was also literally two seconds, this means:
It works quickly, and the effect disappears quickly, too.
In other words: if you want pain relief from nature, the good news is you can get it immediately while viewing nature, and the bad news is that you have to keep viewing nature to continue enjoying the painkilling effect.
So that’s a limitation, but it’s still clearly a very worthy option for a little respite from chronic pain now and again, for example.
Want to learn more?
We’ve written quite a bit about pain management, including:
- Before You Reach For That Tylenol…
- How To Stop Pain Spreading
- How To Dial Down Your Pain
- Managing Chronic Pain (Realistically!)
- Get The Right Help For Your Pain
- The 7 Approaches To Pain Management
- Science-Based Alternative Pain Relief (When Painkillers Aren’t Helping, These Things Might)
Take care!
Share This Post
-
Why Everyone You Don’t Like Is A Narcissist
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about how psychiatry tends to name disorders after how they affect other people, rather than how they affect the bearer, and this is most exemplified when it comes to personality disorders. For example:
“You have a deep insecurity about never being good enough, and you constantly mess up in your attempt to overcompensate? You may have Evil Bastard Disorder!”
“You have a crippling fear of abandonment and that you are fundamentally unloveable, so you do all you can to try to keep people close? You must have Manipulative Bitch Disorder!”
See also: Miss Diagnosis: Anxiety, ADHD, & Women
Antisocial DiagnosesThese days, it is easy to find on YouTube countless videos of how to spot a narcissist, with a list of key traits that all mysteriously describe exactly the exes of everyone in the comments.
And these days it is mostly “narcissist”, because “psychopath” and “sociopath” have fallen out of popular favor a bit:
- perhaps for coming across as overly sensationalized, and thus lacking credibility
- perhaps because “Narcissistic Personality Disorder (NPD)” exists in the DSM-5 (the US’s latest “Diagnostic and Statistical Manual of Mental Disorders”), while psychopathy and sociopathy are not mentioned as existing.
You may be wondering: what do “psychopathy” and “sociopathy” mean?
And the answer is: they mean whatever the speaker wants them to mean. Their definitions and differences/similarities have been vigorously debated by clinicians and lay enthusiasts alike for long enough that the scientific world has pretty much given up on them and moved on.
Stigma vs pathology
Because of the popular media (and social media) representation of NPD, it is easy to armchair diagnose one’s relative/ex/neighbor/in-law/boss/etc as being a narcissist, because the focus is on “narcissists do these bad things that are mean to people”.
If the focus were instead on “narcissists have cripplingly low self-esteem, and are desperate to not show weakness in a world they have learned is harsh and predatory”, then there may not be so many armchair diagnoses—or at the very least, the labels may be attached with a little more compassion, the same way we might with other mental health issues such as depression.
Not that those with depression get an easy time of it socially either—society’s response is generally some manner of “aren’t you better yet, stop being lazy”—but at the very least, depressed people are not typically viewed with hatred.
A quick aside: if you or someone you know is struggling with depression, here are some things that actually help:
The Mental Health First-Aid You’ll Hopefully Never Need
The disorder is not the problem
Maybe your relative, ex, neighbor, etc really is clinically diagnosable as a narcissist. There are still two important things to bear in mind:
- After centuries of diagnosing people with mental health maladies that we now know don’t exist per se (madness, hysteria, etc), and in recent decades countless revisions to the DSM and similar tomes, thank goodness we now have the final and perfect set of definitions that surely won’t be re-written in the next few years or so ← this is irony; it will absolutely be re-written numerous times yet because of course it’s still not a magically perfect descriptor of the broad spectrum of human nature
- The disorder is not the problem; the way they treat (or have treated) you is the problem.
For example, let’s take a key thing generally attributed to narcissists: a lack of empathy
Now, empathy can be divided into:
- affective empathy: the ability to feel what other people are feeling
- cognitive empathy: the ability to intellectually understand what other people are feeling (akin to sympathy, which is the same but with the requisite of having experienced the thing in question oneself)
A narcissist (as well as various other people without NPD) will typically have negligible affective empathy, and their cognitive empathy may be a little sluggish too.
Sluggish = it may take them a beat longer than most people, to realize what an external signifier of emotions means, or correctly guess how something will be felt by others. This can result in gravely misspeaking (or inappropriately emoting), after failing to adequately quickly “read the room” in terms of what would be a socially appropriate response. To save face, they may then either deny/minimize the thing they just said/did, or double-down on it and go on [what for them feels like] the counterattack.
As to why this shutting off of empathy happens: they have learned that the world is painful, and that people are sources of pain, and so—to avoid further pain—have closed themselves off to that, often at a very early age. This will also apply to themselves; narcissists typically have negligible self-empathy too, which is why they will commonly make self-destructive decisions, even while trying to put themselves first.
Important note on how this impacts other people: the “Golden Rule” of “treat others as you would wish to be treated” becomes intangible, as they have no more knowledge of their own emotional needs than they do of anyone else’s, so cannot make that comparison.
Consider: if instead of being blind to empathy, they were colorblind… You would probably not berate them for buying green apples when you asked for red. They were simply incapable of seeing that, and consequently made a mistake. So it is when it’s a part of the brain that’s not working normally.
So… Since the behavior does adversely affect other people, what can be done about it? Even if “hate them for it and call for their eradication from the face of the Earth” is not a reasonable (or compassionate) option, what is?
Take the bull by the horns
Above all, and despite all appearances, a narcissist’s deepest desire is simply to be accepted as good enough. If you throw them a life-ring in that regard, they will generally take it.
So, communicate (gently, because a perceived attack will trigger defensiveness instead, and possibly a counterattack, neither of which are useful to anyone) what behavior is causing a problem and why, and ask them to do an alternative thing instead.
And, this is important, the alternative thing has to be something they are capable of doing. Not merely something that you feel they should be capable of doing, but that they are actually capable of doing.
- So not: “be a bit more sensitive!” because that is like asking the colorblind person to “be a bit more observant about colors”; they are simply not capable of it and it is folly to expect it of them, because no matter how hard they try, they can’t.
- But rather: “it upsets me when you joke about xyz; I know that probably doesn’t make sense to you and that’s ok, it doesn’t have to. I am asking, however, if you will please simply refrain from joking about xyz. Would you do that for me?”
Presented with such, it’s much more likely that the narcissist will drop their previous attempt to be good enough (by joking, because everyone loves someone with a sense of humor, right?) for a new, different attempt to be good enough (by showing “behold, look, I am a good person and doing the thing you asked, of which I am capable”).
That’s just one example, but the same methodology can be applied to most things.
For tricks pertaining to how to communicate such things without causing undue resistance, see:
Seriously Useful Communication Skills
Take care!
Share This Post
-
6-Minute Core Strength – by Dr. Jonathan Su
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t normally do author biographies here, but in this case it’s worth noting that Dr. Su is a physiotherapist, military rehab expert, and an IAYT yoga therapist. So, these things together certainly do lend weight to his advice.
About the “6-minute” thing: this is in the style of the famous “7-minute workout” and “5 Minutes’ Physical Fitness” etc, and refers to how long each exercise session should take. The baseline is one such session per day, though of course doing more than one set of 6 minutes each time is a bonus if you wish to do so.
The exercises are focused on core strength, but they also include hip and shoulder exercises, since these are after all attached to the core, and hip and shoulder mobility counts for a lot.
A particular strength of the book is in troubleshooting mistakes of the kind that aren’t necessarily visible from photos; in this case, Dr. Su explains what you need to go for in a certain exercise, and how to know if you are doing it correctly. This alone is worth the cost of the book, in this reviewer’s opinion.
Bottom line: if you want core strength and want it simple yet comprehensive, this book can guide you.
Click here to check out 6-Minute Core Strength, and strengthen yours!
Share This Post
Related Posts
-
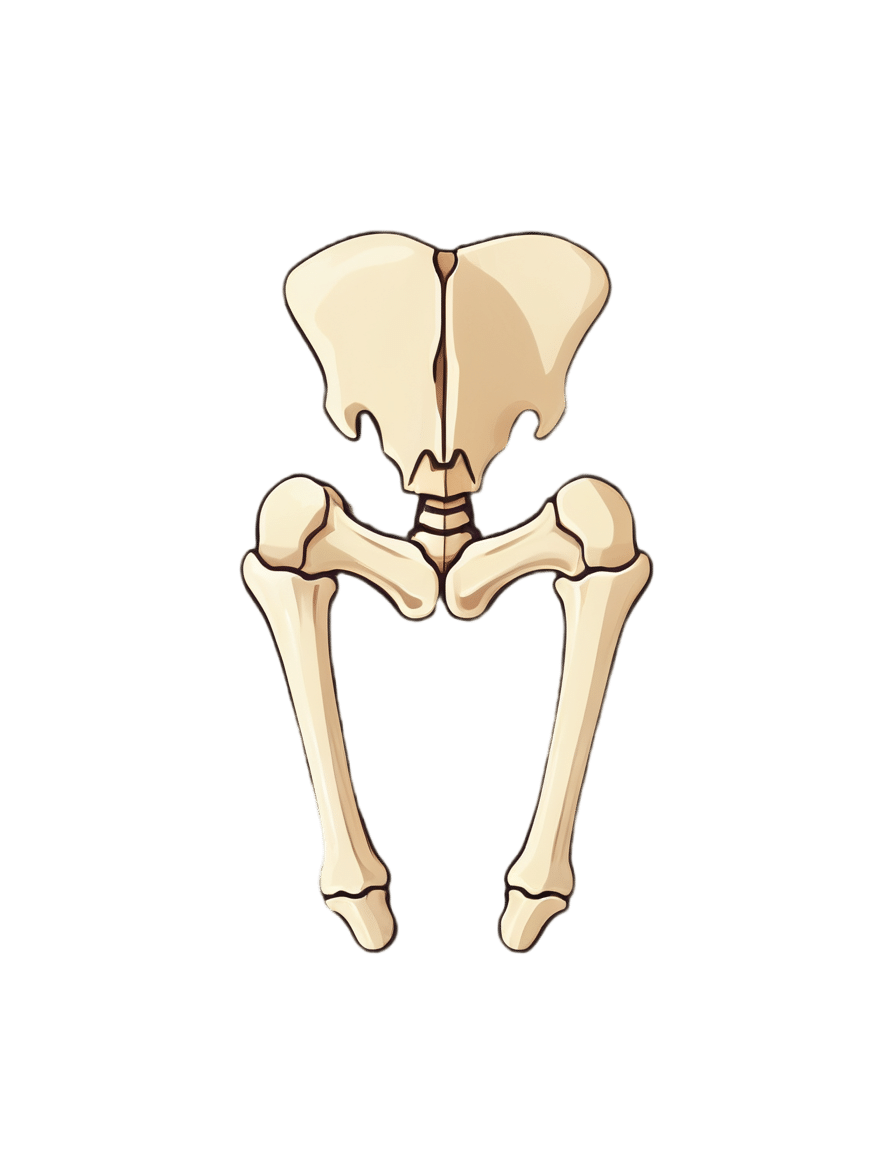
One Cause; Countless Aches
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Is The Cause?
Zac Cupples’ video (below) makes an appealing claim: 90% of movement issues and discomforts we experience daily come from one source: reduced joint space due to increased muscle tension.
For Cupples, this could be causing anything from knee pain to foot pain to ankle pain to hip pain to generalized joint pain to…pretty much any sort of pain.
So, why do we describe this as “appealing”?
Well, if there’s just one cause, that means there is only one thing to fix
Can This Be True?
Whilst we normally stray away from oversimplifications, we found Cupples’ example quite powerful.
Cupples defends his thesis by illustrating it with a simple wrist movement experiment: try moving your wrist in a circle with your palm open, and then do the same with your fist clenched.
Did you notice a difference?
When you clench your fist, movement (normally) becomes restricted and uncomfortable, illustrating how increased tension limits joint space.
It’s a powerful analogy for understanding our body’s mechanics.
So How Do We Fix It?
To combat issues with reduced joint space, Cupples proposes a three-step solution: reducing muscle tension, increasing range of motion in commonly limited areas, and enhancing movement efficiency. He delves into strategies for achieving these, including adopting certain positions and breathing techniques.
There are also some elements of strategic muscle engagement, but we’ll leave that to him to describe:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
90% Of People Skip This Essential Exercise—Are You One Of Them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Single-leg strengthening is essential for joint health at any age (unless you want to bunny-hop up and down the stairs with both feet at once, for example), yet many people overlook it. This neglect often leads to pain, stiffness, and a higher risk of injury.
Dr. Alyssa Kuhn, arthritis specialist, explains how to do it:
On the rise
In this video, different exercise variations—beginner, intermediate, and advanced—are presented to help you build strength at your own pace:
Beginner: start by using a chair, adding a cushion for support if needed. Sit at the edge and position one foot slightly in front of the other in a staggered stance. Stand up and sit down in a controlled manner, allowing the back leg to bear more weight and work harder than the front leg. Do 8–10 repetitions per side and pay attention to whether one side feels weaker. To build strength, incorporate this movement into daily activities, such as standing up from the couch. Master this variation before progressing, to avoid knee injury.
Intermediate: to make the exercise more challenging, you can either use a lower chair, or extend your front foot further out, shifting more weight to your back leg. Only modify one variable at a time to maintain control. Do 8–10 repetitions per side, ensuring proper form. A common mistake is allowing the back knee to move inward, which can cause knee stress. To prevent this, use a mirror to check your form and keep the knee and ankle aligned during movement.
Advanced: when you’re ready, extend your front leg completely with the heel on the ground and toes up, removing its stability and forcing the back leg to work even harder. Maintain controlled movement while keeping your knee and ankle aligned. Repeat the exercise on both sides, focusing extra effort on the weaker leg to build balanced strength.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
The Secret To Better Squats: Foot, Knee, & Ankle Mobility
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can We Side-Step Age-Related Alienation?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When The World Moves Without Us…
We’ve written before about how reduced social engagement can strike people of all ages, and what can be done about it:
How To Beat Loneliness & Isolation
…but today we’re going to talk more about a specific aspect of it, namely, the alienation that can come with old age—and other life transitions too, but getting older is something that (unless accident or incident befall us first) all of us will definitely do.
What’s the difference?
Loneliness is a status, alienation is more of a process. It can be the alienation in the sense of an implicit “you don’t belong here” message from the world that’s geared around the average person and thus alienates those who are not that (a lack of accessibility to people with disabilities can be an important and very active example of this), and it can also be an alienation from what we’ve previously considered our “niche” in the world—the loss of purpose many people feel upon retirement fits this bill. It can even be a more generalized alienation from our younger selves; it’s easy to have a self-image that doesn’t match one’s current reality, for instance.
Read more: Estranged by Time: Alienation in the Aging Process
So, how to “un-alienate”?
To “un-alienate”, that is to say, to integrate/reintegrate, can be hard. Some things may even be outright impossible, but most will not be!
Consider how, for example, former athletes become coaches—or for that matter, how former party-goers might become party-hosts (even if the kind of “party” might change with time, give or take the pace at which we like to live our lives).
What’s important is that we take what matters the most to us, and examine how we can realistically still engage with that thing.
This is different from trying to hold on grimly to something that’s no longer our speed.
Letting go of the only thing we’ve known will always be scary; sometimes it’s for the best, and sometimes what we really need is just more of a pivot, like the examples above. The crux lies in knowing which:
- Is our relationship with the thing (whatever it may be) still working for us, or is it just bringing strife now?
- If it’s not working for us, is it because of a specific aspect that could be side-stepped while keeping the rest?
- If we’re going to drop that thing entirely (or be dropped by it, which, while cruel, also happens in life), then where are we going to land?
This latter is one where foresight is a gift, because if we bury our heads in the sand we’re going to land wherever we’re dropped, whereas if we acknowledge the process, we can make a strategic move and land on our feet.
Here’s a good pop-science article about this—it’s aimed at people around retirement age, but honestly the advice is relevant for people of all ages, and facing all manner of life transitions, e.g. career transitions (of which retirement is of course the career transition to end all career transitions), relationship transitions (including B/B/B/B: births, betrothals/break-ups, and bereavements) health transitions (usually: life-changing illnesses and/or disabilities—which again, happens to most of us if something doesn’t get us first), etc. So with all that in mind, this becomes more of a “how to reassess your life at those times when it needs reassessing”:
How to Reassess Your Life in Retirement
But that doesn’t mean that letting go is always necessary
Sometimes, the opposite! Sometimes, the age-old advice to “lean in” really is all the situation calls for, which means:
- Be ready to say “yes” to things, and if nobody’s asking, be ready to “hey, do you wanna…?” and take a “build it and they will come” approach. This includes with people of different ages, too! Intergenerational friendships can be very rewarding for all concerned, if done right. Communities that span age-ranges can be great for this—they might be about special interests (this writer has friends ranging through four generations from playing chess, for instance), they could be religious communities if we be religious, LGBT groups if that fits for us, even mutual support groups such as for specific disabilities or chronic illness if we have such—notice how the very things that might isolate us can also bring us together!
- Be open-minded to new experiences; it’s easy to get stuck in a rut of “I’ve never done that” and mistake that self-assessment for an uncritical assumption of “I’m not the kind of person who does that”. Sometimes, you really won’t be! But at least think about it and entertain the possibility, before dismissing it out of hand. And, here’s a life tip: it can be really good to (within the realms of safety, and one’s personal moral principles, of course) take an approach of “try anything once”. Even if we’re almost certain we won’t like it, and even if we then turn out to indeed not like it, it can be a refreshing experience—and now we can say “Yep, tried that, not doing that again” from a position of informed knowledge. That’s the only way we get to look back on a richly lived life of broad experiences, after all, and it is never too late for such.
- Be comfortable prioritizing quality over quantity. This goes for friends, it goes for activities, it goes for experiences. The topic of “what’s the best number of friends to have?” has been a matter of discussion since at least ancient Greek times (Plato and Aristotle examined this extensively), but whatever number we might arrive at, it’s clear that quality is the critical factor, and quantity after that is just a matter of optimizing.
In short: make sure you’re investing—in your relationships, in your areas of interest, in your community (whatever that may mean for you personally), and most of all, and never forget this: in yourself.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: