Functional Exercise For Seniors – by James Atkinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of exercises books are tailored to 20-year-old athletes training for their first Tough Mudder. Others, that the only thing standing between us and a perfect Retroflex Countersupine Divine Pretzel position is a professionally-lit Instagrammable photo.
This one’s not like that.
But! Nor does it think being over a certain age is a reason to not have genuinely robust health, of the kind that may make some younger people envious. So, it lays out, in progressive format, guidelines for exercises targeted at everything we need to build and maintain as we get older.
The writing style is clear, and the illustrations too (the cover art is the same style as the illustrations inside).
Bottom line: if you’re looking for a workout guide that understands you are nearer 80 than 18, and/but also doesn’t assume your age limits your exercise potential to “wrist exercises in chair”, then this book is a fine pick.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
This Is Your Brain on Food – by Dr. Uma Naidoo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Diet will fix your brain” is a bold claim that often comes from wishful thinking and an optimistic place where anecdote is louder than evidence. But, diet does incontrovertibly also affect brain health. So, what does Dr. Naidoo bring to the table?
The author is a Harvard-trained psychiatrist, a professional chef who graduated with her culinary school’s most coveted award, and a trained-and-certified nutritionist. Between those three qualifications, it’s safe to she knows her stuff when it comes to the niche that is nutritional psychiatry. And it shows.
She takes us through the neurochemistry involved, what chemicals are consumed, made, affected, inhibited, upregulated, etc, what passes through the blood-brain barrier and what doesn’t, what part the gut really plays in its “second brain” role, and how we can leverage that—as well as mythbusting a lot of popular misconceptions about certain foods and moods.
There’s hard science in here, but presented in quite a pop-science way, making for a very light yet informative read.
Bottom line: if you’d like to better understand what your food is doing to your brain (and what it could be doing instead), then this is a top-tier book for you!
Click here to check out This Is Your Brain On Food, and get to know yours!
Share This Post
-
Ultra-Processed People – by Dr. Chris van Tulleken
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It probably won’t come as a great surprise to any of our readers that ultra-processed food is—to make a sweeping generalization—not fabulous for the health. So, what does this book offer beyond that?
Perhaps this book’s greatest strength is in showing not just what ultra-processed foods are, but why they are. In principle, food being highly processed should be neither good nor bad by default. Much like GMOs, if a food is modified to be more nutritious, that should be good, right?
Only, that’s mostly not what happens. What happens instead is that food is modified (be it genetically or by ultra-processing) to be cheaper to produce, and thus maximise the profit margin.
The addition of a compound that increases shelf-life but harms the health, increases sales and is a net positive for the manufacturer, for instance. Dr. van Tulleken offers us many, many, examples and explanations of such cost-cutting strategies at our expense.
In terms of qualifications, the author has an MD from Oxford, and also a PhD, but the latter is in molecular virology; not so relevant here. Yet, we are not expected to take an “argument from authority”, and instead, Dr. van Tulleken takes great pains to go through a lot of studies with us—the good, the bad, and the misleading.
If the book has a downside, then this reviewer would say it’s in the format; it’s less a reference book, and more a 384-page polemic. But, that’s a subjective criticism, and for those who like that sort of thing, that is the sort of thing that they like.
Share This Post
-
What are ‘collarium’ sunbeds? Here’s why you should stay away
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reports have recently emerged that solariums, or sunbeds – largely banned in Australia because they increase the risk of skin cancer – are being rebranded as “collarium” sunbeds (“coll” being short for collagen).
Commercial tanning and beauty salons in Queensland, New South Wales and Victoria are marketing collariums, with manufacturers and operators claiming they provide a longer lasting tan and stimulate collagen production, among other purported benefits.
A collarium sunbed emits both UV radiation and a mix of visible wavelength colours to produce a pink or red light. Like an old-school sunbed, the user lies in it for ten to 20 minute sessions to quickly develop a tan.
But as several experts have argued, the providers’ claims about safety and effectiveness don’t stack up.
Why were sunbeds banned?
Commercial sunbeds have been illegal across Australia since 2016 (except for in the Northern Territory) under state-based radiation safety laws. It’s still legal to sell and own a sunbed for private use.
Their dangers were highlighted by young Australians including Clare Oliver who developed melanoma after using sunbeds. Oliver featured in the No Tan Is Worth Dying For campaign and died from her melanoma at age 26 in 2007.
Sunbeds lead to tanning by emitting UV radiation – as much as six times the amount of UV we’re exposed to from the summer sun. When the skin detects enough DNA damage, it boosts the production of melanin, the brown pigment that gives you the tanned look, to try to filter some UV out before it hits the DNA. This is only partially successful, providing the equivalent of two to four SPF.
Essentially, if your body is producing a tan, it has detected a significant amount of DNA damage in your skin.
Research shows people who have used sunbeds at least once have a 41% increased risk of developing melanoma, while ten or more sunbed sessions led to a 100% increased risk.
In 2008, Australian researchers estimated that each year, sunbeds caused 281 cases of melanoma, 2,572 cases of squamous cell carcinoma (another common type of skin cancer), and $3 million in heath-care costs, mostly to Medicare.
How are collarium sunbeds supposed to be different?
Australian sellers of collarium sunbeds imply they are safe, but their machine descriptions note the use of UV radiation, particularly UVA.
UVA is one part of the spectrum of UV radiation. It penetrates deeper into the skin than UVB. While UVB promotes cancer-causing mutations by discharging energy straight into the DNA strand, UVA sets off damage by creating reactive oxygen species, which are unstable compounds that react easily with many types of cell structures and molecules. These damage cell membranes, protein structures and DNA.
Evidence shows all types of sunbeds increase the risk of melanoma, including those that use only UVA.
Some manufacturers and clinics suggest the machine’s light spectrum increases UV compatibility, but it’s not clear what this means. Adding red or pink light to the mix won’t negate the harm from the UV. If you’re getting a tan, you have a significant amount of DNA damage.
Collagen claims
One particularly odd claim about collarium sunbeds is that they stimulate collagen.
Collagen is the main supportive tissue in our skin. It provides elasticity and strength, and a youthful appearance. Collagen is constantly synthesised and broken down, and when the balance between production and recycling is lost, the skin loses strength and develops wrinkles. The collagen bundles become thin and fragmented. This is a natural part of ageing, but is accelerated by UV exposure.
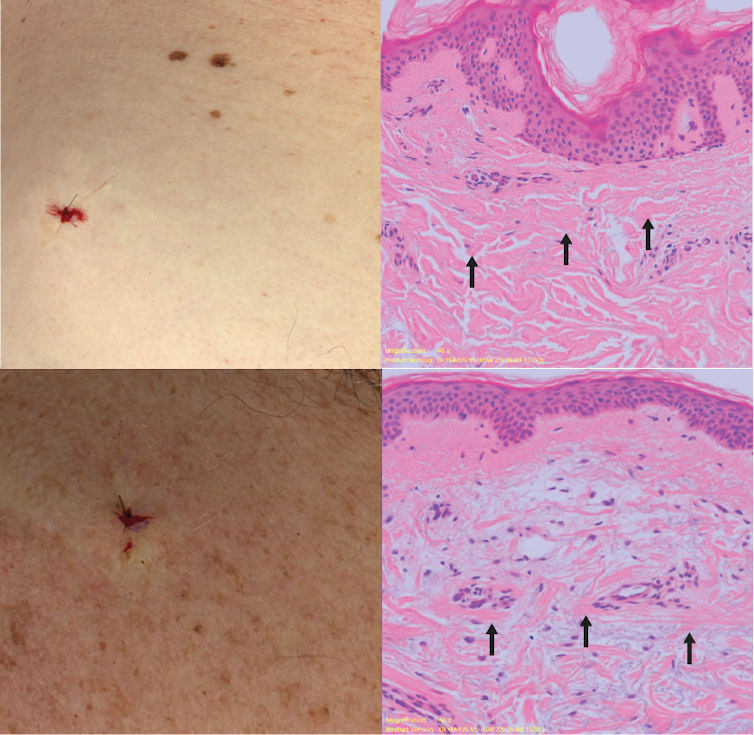
Sun-protected skin (top) has thick bands of pink collagen (arrows) in the dermis, as seen on microscopic examination. Chronically sun-damaged skin (bottom) has much thinner collagen bands.
Katie Lee/UQThe reactive oxygen species generated by UVA light damage existing collagen structures and kick off a molecular chain of events that downgrades collagen-producing enzymes and increases collagen-destroying enzymes. Over time, a build-up of degraded collagen fragments in the skin promotes even more destruction.
While there is growing evidence red light therapy alone could be useful in wound healing and skin rejuvenation, the UV radiation in collarium sunbeds is likely to undo any benefit from the red light.
What about phototherapy?
There are medical treatments that use controlled UV radiation doses to treat chronic inflammatory skin diseases like psoriasis.
The anti-collagen effects of UVA can also be used to treat thickened scars and keloids. Side-effects of UV phototherapy include tanning, itchiness, dryness, cold sore virus reactivation and, notably, premature skin ageing.
These treatments use the minimum exposure necessary to treat the condition, and are usually restricted to the affected body part to minimise risks of future cancer. They are administered under medical supervision and are not recommended for people already at high risk of skin cancer, such as people with atypical moles.
So what happens now?
It looks like many collariums are just sunbeds rebranded with red light. Queensland Health is currently investigating whether these salons are breaching the state’s Radiation Safety Act, and operators could face large fines.
As the 2024 Australians of the Year – melanoma treatment pioneers Georgina Long and Richard Scolyer – highlighted in their acceptance speech, “there is nothing healthy about a tan”, and we need to stop glamorising tanning.
However, if you’re desperate for the tanned look, there is a safer and easy way to get one – out of a bottle or by visiting a salon for a spray tan.
Katie Lee, PhD Candidate, Dermatology Research Centre, The University of Queensland and Anne Cust, Professor of Cancer Epidemiology, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
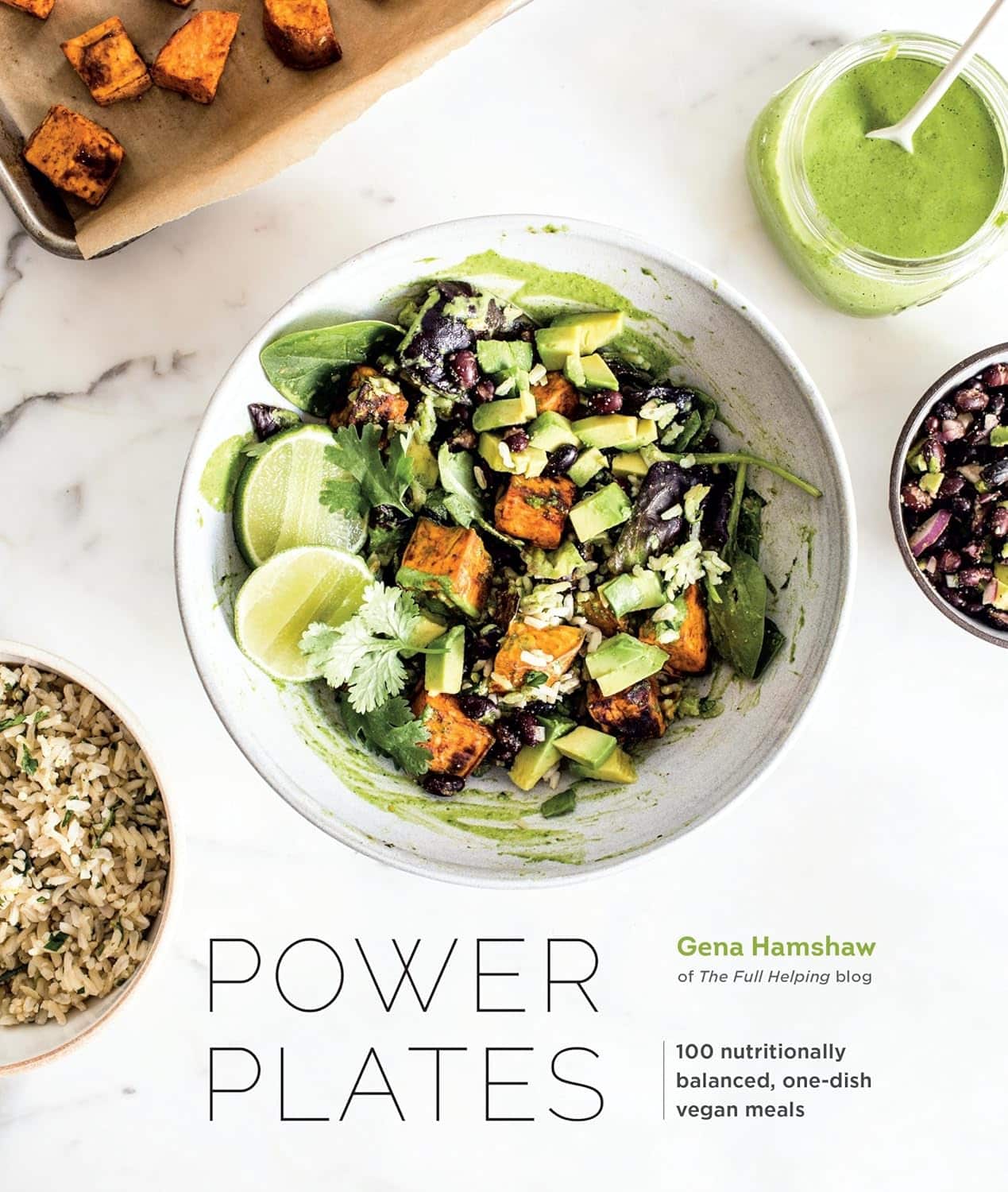
Power Plates – by Gena Hamshaw
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superfoods are all well and good, but there are only so many ways one can reasonably include watercress before it starts becoming a chore.
Happily, Gena Hamshaw is here with a hundred single-dish vegan meals, that are not only nutritionally balanced as the subtitle promises, but also, as the title suggests, are nutritional powerhouses too.
In the category of criticism, some ingredients are not so universally available as others. For example, depending on where you live, your local supermarket might not have freekeh, gochujang, or pomegranate molasses.
However, most of the recipes have ingredients that are easy enough to source in any medium-sized supermarket, and for the ones that aren’t, we do recommend ordering the ingredient online and trying something you might not otherwise have experienced—that’s an important thing in life, after all!
Bottom line: if you’d like plant-based meals that are packed full of nutrients and are delicious too, this is a top-tier recipe book.
Click here to check out Power Plates, and enjoy a wide variety of plant-based cuisine!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
For many who are suffering with prolonged grief, the holidays can be a time to reflect and find meaning in loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The holiday season is meant to be filled with joy, connection and celebration of rituals. Many people, however, are starkly reminded of their grief this time of year and of whom – or what – they have lost.
The added stress of the holiday season doesn’t help. Studies show that the holidays negatively affect many people’s mental health.
While COVID-19-related stressors may have lessened, the grief from change and loss that so many endured during the pandemic persists. This can cause difficult emotions to resurface when they are least expected.
I am a licensed therapist and trauma-sensitive yoga instructor. For the last 12 years, I’ve helped clients and families manage grief, depression, anxiety and complex trauma. This includes many health care workers and first responders who have recounted endless stories to me about how the pandemic increased burnout and affected their mental health and quality of life.
I developed an online program that research shows has improved their well-being. And I’ve observed firsthand how much grief and sadness can intensify during the holidays.
Post-pandemic holidays and prolonged grief
During the pandemic, family dynamics, close relationships and social connections were strained, mental health problems increased or worsened, and most people’s holiday traditions and routines were upended.
Those who lost a loved one during the pandemic may not have been able to practice rituals such as holding a memorial service, further delaying the grieving process. As a result, holiday traditions may feel more painful now for some. Time off from school or work can also trigger more intense feelings of grief and contribute to feelings of loneliness, isolation or depression.
Sometimes feelings of grief are so persistent and severe that they interfere with daily life. For the past several decades, researchers and clinicians have been grappling with how to clearly define and treat complicated grief that does not abate over time.
In March 2022, a new entry to describe complicated grief was added to the Diagnostic and Statistical Manual of Mental Disorders, or DSM, which classifies a spectrum of mental health disorders and problems to better understand people’s symptoms and experiences in order to treat them.
This newly defined condition is called prolonged grief disorder. About 10% of bereaved adults are at risk, and those rates appear to have increased in the aftermath of the pandemic.
People with prolonged grief disorder experience intense emotions, longing for the deceased, or troublesome preoccupation with memories of their loved one. Some also find it difficult to reengage socially and may feel emotionally numb. They commonly avoid reminders of their loved one and may experience a loss of identity and feel bleak about their future. These symptoms persist nearly every day for at least a month. Prolonged grief disorder can be diagnosed at least one year after a significant loss for adults and at least six months after a loss for children.
I am no stranger to complicated grief: A close friend of mine died by suicide when I was in college, and I was one of the last people he spoke to before he ended his life. This upended my sense of predictability and control in my life and left me untangling the many existential themes that suicide loss survivors often face.
How grieving alters brain chemistry
Research suggests that grief not only has negative consequences for a person’s physical health, but for brain chemistry too.
The feeling of grief and intense yearning may disrupt the neural reward systems in the brain. When bereaved individuals seek connection to their lost loved one, they are craving the chemical reward they felt before their loss when they connected with that person. These reward-seeking behaviors tend to operate on a feedback loop, functioning similar to substance addiction, and could be why some people get stuck in the despair of their grief.
One study showed an increased activation of the amygdala when showing death-related images to people who are dealing with complicated grief, compared to adults who are not grieving a loss. The amygdala, which initiates our fight or flight response for survival, is also associated with managing distress when separated from a loved one. These changes in the brain might explain the great impact prolonged grief has on someone’s life and their ability to function.
Recognizing prolonged grief disorder
Experts have developed scales to help measure symptoms of prolonged grief disorder. If you identify with some of these signs for at least one year, it may be time to reach out to a mental health professional.
Grief is not linear and doesn’t follow a timeline. It is a dynamic, evolving process that is different for everyone. There is no wrong way to grieve, so be compassionate to yourself and don’t make judgments on what you should or shouldn’t be doing.
Increasing your social supports and engaging in meaningful activities are important first steps. It is critical to address any preexisting or co-occurring mental health concerns such as anxiety, depression or post-traumatic stress.
It can be easy to confuse grief with depression, as some symptoms do overlap, but there are critical differences.
If you are experiencing symptoms of depression for longer than a few weeks and it is affecting your everyday life, work and relationships, it may be time to talk with your primary care doctor or therapist.
A sixth stage of grief
I have found that naming the stage of grief that someone is experiencing helps diminish the power it might have over them, allowing them to mourn their loss.
For decades, most clinicians and researchers have recognized five stages of grief: denial/shock, anger, depression, bargaining and acceptance.
But “accepting” your grief doesn’t sit well for many. That is why a sixth stage of grief, called “finding meaning,” adds another perspective. Honoring a loss by reflecting on its meaning and the weight of its impact can help people discover ways to move forward. Recognizing how one’s life and identity are different while making space for your grief during the holidays might be one way to soften the despair.
When my friend died by suicide, I found a deeper appreciation for what he brought into my life, soaking up the moments he would have enjoyed, in honor of him. After many years, I was able to find meaning by spreading mental health awareness. I spoke as an expert presenter for suicide prevention organizations, wrote about suicide loss and became certified to teach my local community how to respond to someone experiencing signs of mental health distress or crisis through Mental Health First Aid courses. Finding meaning is different for everyone, though.
Sometimes, adding a routine or holiday tradition can ease the pain and allow a new version of life, while still remembering your loved one. Take out that old recipe or visit your favorite restaurant you enjoyed together. You can choose to stay open to what life has to offer, while grieving and honoring your loss. This may offer new meaning to what – and who – is around you.
If you need emotional support or are in a mental health crisis, dial 988 or chat online with a crisis counselor.
Mandy Doria, Assistant Professor of Psychiatry, University of Colorado Anschutz Medical Campus
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
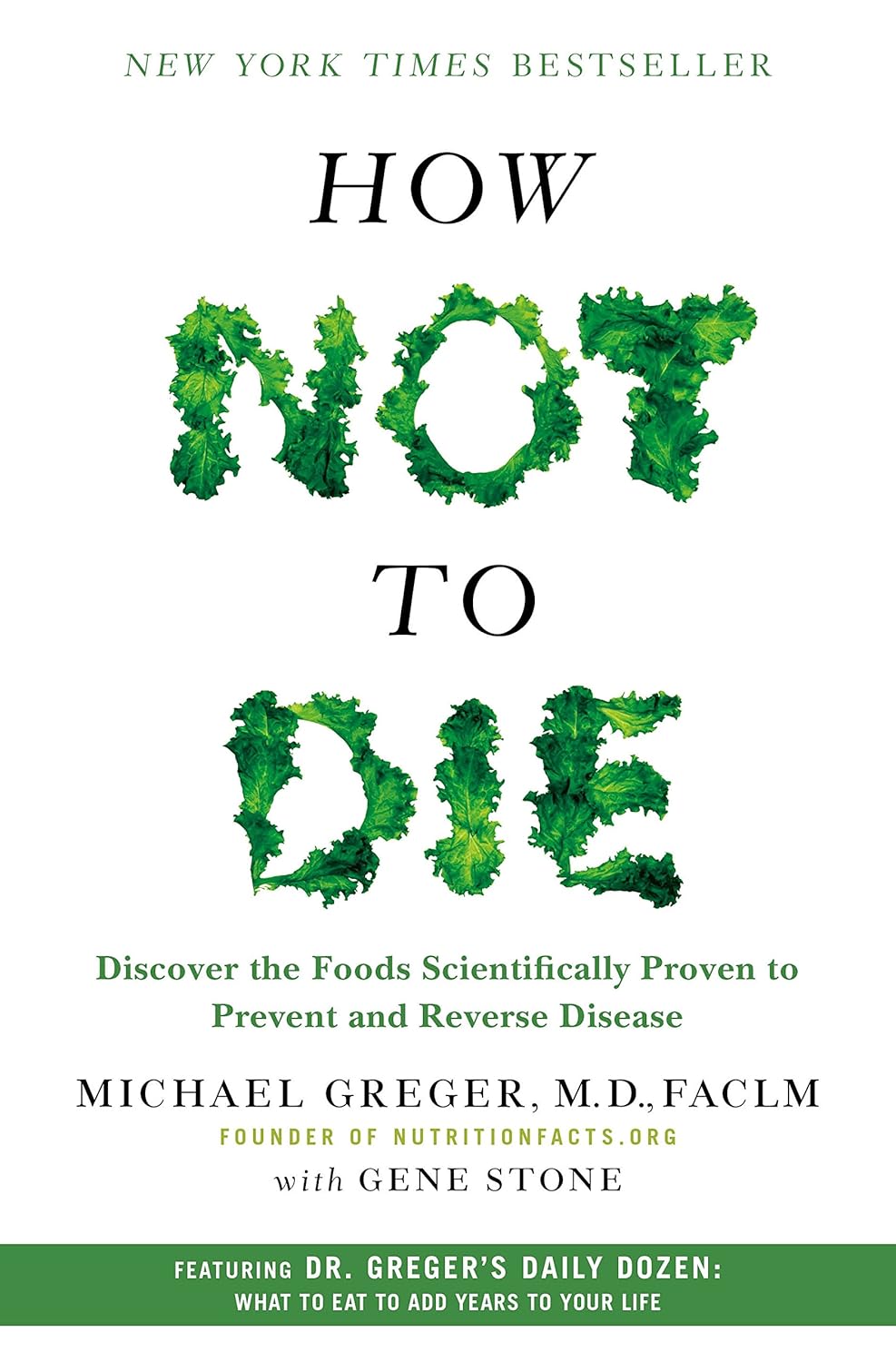
How Not To Die – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed this book some years ago, but we’re revisiting it now because:
- It really is a book that should be in every healthspan-enjoyer’s collection
- Our book reviews back then were not as comprehensive as now (though we still generally try to fit into the “it takes about one minute to read this review” idea, sometimes we’ll spend a little extra time).
Dr. Greger (of “Dr. Greger’s Daily Dozen” fame) outlines for us in cold hard facts and stats what’s most likely to be our cause of death. While this is not a cheery premise for a book, he then sets out to work back from there—what could have prevented those specific things?
Thus, while the book doesn’t confer immortality (the title is not “how to not die”, after all), it does teach us how not to die—i.e, from heart disease, lung diseases, brain diseases, digestive cancers, infections, diabetes, high blood pressure, liver disease, blood cancers, kidney disease, breast cancer, suicidal depression, prostate cancer, Parkinson’s disease, and even iatrogenic causes.
This it does with a lot of solid science, explained for the layperson, and/but without holding back when it comes to big words, and a lot of them, at that. If you want to add in daily exercises, just lifting the book could be a start; weighing in at 678 pages, it’s an information-dense tome that’s more likely to be sifted through than read cover-to-cover.
The style is thus dense science somewhat editorialized for lay readability, and well-evidenced with around 3,000 citations. That’s not a typo; there are 178 pages of bibliography at the back with about 15–20 scientific references per page.
In terms of practical use, he does also devote chapters to that, it’s not just all textbook. Indeed, he discusses the reasonings behind the items, portion sizes, and quantities of his “daily dozen” foods, so that the reader will understand how much bang-for-buck they deliver, and then it’ll seem a lot less like an arbitrary list, and more likely to be adopted and maintained.
Bottom line: if you care about not getting life-threatening illnesses (which at the end of the day, come to most people at some point), then this book is a must-read.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: