Fast. Feast. Repeat – by Dr. Gin Stephens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed intermittent fasting books before, so what makes this one different?
The title “Fast. Feast. Repeat.” doesn’t give much away; after all, we already know that that’s what intermittent fasting is.
After taking the reader though the basics of how intermittent fasting works and what it does for the body, much of the rest of the book is given over to improvements.
That’s what the real strength of this book is: ways to make intermittent fasting more efficient, including how to avoid plateaus. After all, sometimes it can seem like the only way to push further with intermittent fasting is to restrict the eating window further. Not so!
Instead, Dr. Stephens gives us ways to keep confusing our metabolism (in a good way) if, for example, we had a weight loss goal we haven’t met yet.
Best of all, this comes without actually having to eat less.
Bottom line: if you want to be in good physical health, and/but also believe that life is for living and you enjoy eating food, then this book can resolve that age-old dilemma!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Silent Struggle – by L. William Ross-Child, MLC
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The vast majority of literature out there about ADHD is about children. And fair enough, there are enough popular misunderstandings of ADHD in children so it’s good those works exist… but what about adults?
Adults face different challenges than children, and have different responsibilities. People have different expectations. And even if you say you have ADHD… If you’re not behaving like a squirrel, they will often not accept this, much less understand it, because half the actual symptoms are not what most people think they are.
Ross-Child first lays out the neurobiological underpinnings of ADHD. This is a good place to start, because the physiology of it explains a lot of the other parts of it that can otherwise seem quite mystifying.
Thereafter, he looks one-by-one at the various cognitive and behavioral aspects of ADHD in adults, which will surely help the reader to better understand themself (or perhaps a loved one).
The next part of the book is given over to an exploration of ADHD and the differences it can make in the workplace, relationships (incl. ADHD and sex), as well as parenting, and how these things can all be navigated better by all concerned.
The style throughout is light and very readable, peppered with science made comprehensible. If there’s any flaw, it’s that there are only two pages of references in the bibliography—we’d have liked to have seen more.
All in all though, a really useful guide if you or a loved one has ADHD and you’d like strategies for working with (or around) this condition in a world not made to be kind to such.
Order your copy of “The Silent Struggle: Taking Charge of ADHD in Adults” from Amazon today!
Share This Post
-
Can You Step Backwards Without Your Foot Or Torso Turning Out?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Walking backwards is often overlooked, but research shows it can enhance forward walking, especially in stroke patients; it has other benefits for everyone else, too. The physiotherapists at Fitness4Life Physical Therapy explain:
…and one step back
How it works: walking backwards heightens proprioception and stimulates muscles, improving balance and posture. Additionally, our daily lives tend to involve forward-leaning postures, causing upper back bending, and walking backwards helps counterbalance this.
Extra benefits: training to walk backwards can reduce the risk of falls, as stepping back is a common movement that is often untrained.
Exercise: try doing backwards lunges, to assess your skill and balance while moving backward. If foot rotation or torso rotation occurs during the exercise, then there’s room for improvement. Correcting these movements is then simply a matter of practicing backward lunges without turning.
10almonds tip: any exercise is only as good as your will to actually do it. For this reason, dancing is a great exercise in this case, as almost all forms of dance involve stepping backwards (in order to have steps without travelling somewhere, forwards steps are usually balanced with backwards ones)
For more on all this, plus a visual demonstration of the exercise, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Fall Special ← About how to avoid falling, and how to avoid (and failing that, at least minimize) injury if you do fall. If you think this only happens to other/older people, remember, there’s a first time for everything, so it is better to be prepared in advance!
Take care!
Share This Post
-
Never Too Late To Start Over: Finding Purpose At Any Age
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dana Findwell’s late 50s were not an easy time, but upon now hitting 60 (this week, at time of writing), she’s enthusiastically throwing herself into the things that bring her purpose, and so can you.
Start where you are
Findwell was already no stranger to starting again, having been married and divorced twice, and having moved frequently, requiring constant “life resets”.
Nevertheless, she always had her work to fall back on; she was a graphic designer and art director for 30 years… Until burnout struck.
And when burnout struck, so did COVID, resulting in the loss of her job. Her job wasn’t the only thing she lost though, as her mother died around the same time. All in all, it was a lot, and not the fun kind of “a lot”.
Struggling to find a new career direction, she ended up starting a small business for herself, so that she could direct the pace; pressing forwards as and when she had the energy. This became her new “ikigai“, the main thing that brings a sense of purpose to her life, but getting one part of her life back into order brought her attention to the rest; she realized she’d neglected her health, so she joined a gym. And a weightlifting class. And a hip-hop class. And she took up the practice of Japanese drumming (for the unfamiliar, this can be a rather athletic ability; it’s not a matter of sitting at a drum kit).
And now? Her future is still not clear, but that’s ok, because she’s making it as she goes, and she’s doing it her way, trusting in her ability to handle what may come up, and doing the things now that future-her will be glad of having done (e.g. laying the groundwork of both financial security and good health).
Change can sometimes be triggered by adverse circumstances, but there’s always the opportunity to find something better. For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
Related Posts
-
Stop The World…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some news highlights from this week:
“US vs Them”?
With the US now set to lose its WHO membership, what does that mean for Americans? For most, the consequences will be indirect:
- the nation’s scientists and institutions will be somewhat “left out in the cold” when it comes to international scientific collaboration in the field of health
- the US will no longer enjoy a position of influence and power within the WHO, which organization’s reports and position statements have a lot of sway over the world’s health practices
Are there any benefits (of leaving the WHO) for Americans? Yes, there is one: the US will no longer be paying into the WHO’s budget, which means:
- the US will save the 0.006% of the Federal budget that it was paying into the WHO annually
- for the average American’s monthly budget, that means (if the saving is passed on) you’ll have an extra dime
However, since US scientific institutions will still need access to international data, likely that access will need to be paid separately, at a higher rate than US membership in WHO cost.
In short: it seems likely to go the way that Brexit did: “saving” on membership fees and then paying more for access to less.
Why is the US leaving again? The stated reasons were mainly twofold:
- the cost of US membership (the US’s contribution constituted 15% of the the overall WHO budget)
- holding the US’s disproportionately high COVID death rate (especially compared to countries such as China) to be a case of WHO mismanagement
Read in full: What losing WHO membership means for the U.S.
Related: What Would a Second Trump Presidency Look Like for Health Care? ← this was a speculative post by KFF Health News, last year
Halt, You’re Under A Breast
More seriously, this is about halting the metastasis of cancerous tumors in the breast. It is reasonable to expect the same principle and thus treatment may apply to other cancers too, but this is where the research is at for now (breast cancer research gets a lot of funding).
And, what principle and treatment is this, you ask? It’s about the foxglove-derived drug digoxin, and how it stops cancerous cells from forming clusters, and even actively dissolves clusters that have already formed. No clusters means no new tumors, which means no metastasis. No metastasis, in turn, means the cancer becomes much more treatable because it’s no longer a game of whack-a-mole; instead of spreading to other places, it’s a much more manageable case of “here’s the tumor, now let’s kill it with something”.
Note: yes, that does mean the tumor still needs killing by some other means—digoxin won’t do that, it “just” stops it from spreading while treatment is undertaken.
Read in full: Proof-of-concept study dissolves clusters of breast cancer cells to prevent metastases
Related: The Hormone Therapy That Reduces Breast Cancer Risk & More
Force Of Habit
“It takes 21 days to make a habit”, says popular lore. Popular is not, however, evidence-based:
❝This systematic review of 20 studies involving 2601 participants challenges the prevailing notion of rapid habit formation, revealing that health-related habits typically require 2–5 months to develop, with substantial individual variability ranging from 4 to 335 days. The meta-analysis demonstrated significant improvements in habit scores across various health behaviours, with key determinants including morning practices, personal choice, and behavioural characteristics❞
So, this is not a lottery, “maybe it will take until Tuesday, maybe it will take nearly a year”, so much as “there are important factors that seriously change how long a habit takes to become engrained, and here is what those factors are”.
Read in full: Study reveals healthy habits take longer than 21 days to set in
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
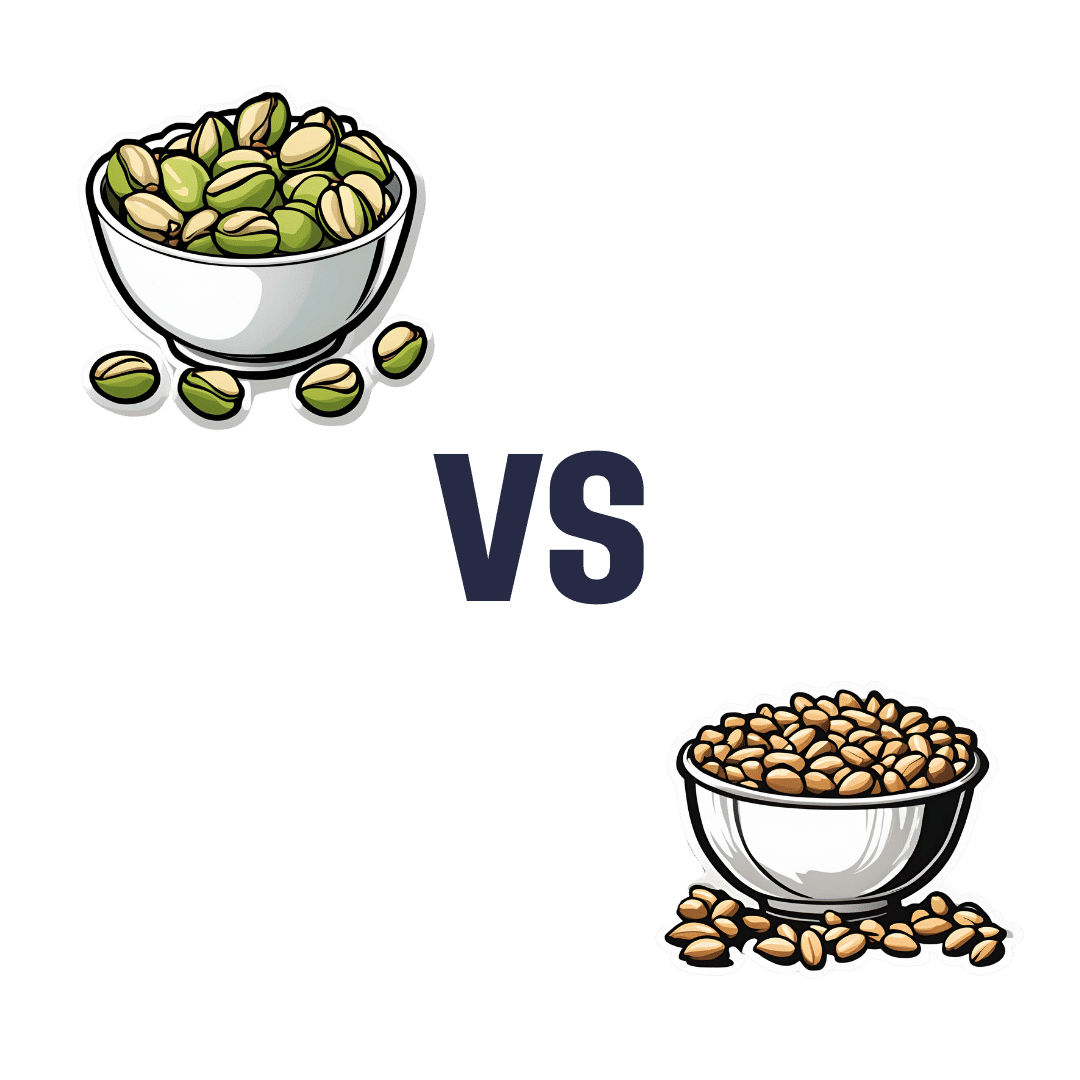
Pistachios vs Pine Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pistachios to pine nuts, we picked the pistachios.
Why?
First looking at the macros, pistachios have nearly 2x the protein while pine nuts have nearly 2x the fat. The fats are healthy in moderation (mostly polyunsaturated, a fair portion of monounsaturated, and a little saturated), but we’re going to value the protein content higher. Also, pistachios have approximately 2x the carbs, and/but nearly 3x the fiber. All in all, we’ll call this section a moderate win for pistachios.
When it comes to vitamins, pistachios have more of vitamins A, B1, B5, B6, B9, and C, while pine nuts have more of vitamins B2, B3, E, K, and choline. All in all, pistachios are scraping a 6:5 win here, or we could call it a tie if we want to value pine nuts’ vitamins more (due to the difference in how many foods each vitamin is found in, and thus the likelihood of having a deficiency or not).
In the category of minerals, pistachios have more calcium, copper, potassium, and selenium, while pine nuts have more iron, magnesium, manganese, and zinc. This would be a tie if we just call it 4:4, but what’s worth noting is that while both of these nuts are a good source of most of the minerals mentioned, pine nuts aren’t a very good source of calcium or selenium, so we’re going to declare this section a very marginal win for pistachios.
Adding up the moderate win, the scraped win, and the barely scraped win, all adds up to a win for pistachios. However, as you might have noticed, both are great so do enjoy both if you can!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Radical Longevity – by Dr. Ann Gittleman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Gittleman takes a comprehensive approach, advising us about avoiding AGEs, freeing up fascia, stimulating cellular rejuvenation, the mind-gut connection, keeping the immune system healthy, and more.
The “plan” promised by the subtitle involves identifying the key factors of nutrition and lifestyle most impactful to you, and adjusting them accordingly, in a multistep, author-walks-the-reader-by-the-hand process.
There’s also, for those who prefer it, a large section (seven chapters) on a body part/system by body part/system approach, e.g. brain health, heart health, revitalizing skin, reversing hair loss, repairing bones, muscles, joints, etc.
The writing style is quite casual,butalso with a mind to education, with its call-out boxes, bullet-point summaries, and so forth. There is a “select references” section, but if one wants to find studies, it’s often necessary to go looking, as there aren’t inline citations.
Bottom line: we’d love to see better referencing, but otherwise this is a top-tier anti-aging book, and a lot more accessible than most, without skimping on depth and breadth.
Click here to check out Radical Longevity, and get rejuvenating radically!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: