End the Insomnia Struggle – by Dr. Colleen Ehrnstrom and Dr. Alisha Brosse
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed sleep books before, and we always try to recommend books that have something a little different than the rest, so what makes this one stand out?
While there is the usual quick overview of the basics that we’re sure you already know (sleep hygiene etc), most of the attention here is given to cold, hard clinical psychology… in a highly personalized way.
How, you may ask, can they personalize a book, that is the same for everyone?
The answer is, by guiding the reader through examining our own situation. With template logbooks, worksheets, and the like—for this reason we recommend getting a paper copy of the book, rather than the Kindle version, in case you’d like to use/photocopy those.
Essentially, reading this book is much like having your own psychologist (or two) to guide you through finding a path to better sleep.
The therapeutic approach, by the way, is a combination of Cognitive Behavioral Therapy (CBT) and Acceptance-Commitment Therapy (ACT), which work very well together here.
Bottom line: if you’ve changed your bedsheets and turned off your electronic devices and need something a little more, this book is the psychological “big guns” for removing the barriers between you and good sleep.
Click here to check out End the Insomnia Struggle, and end yours once and for all!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
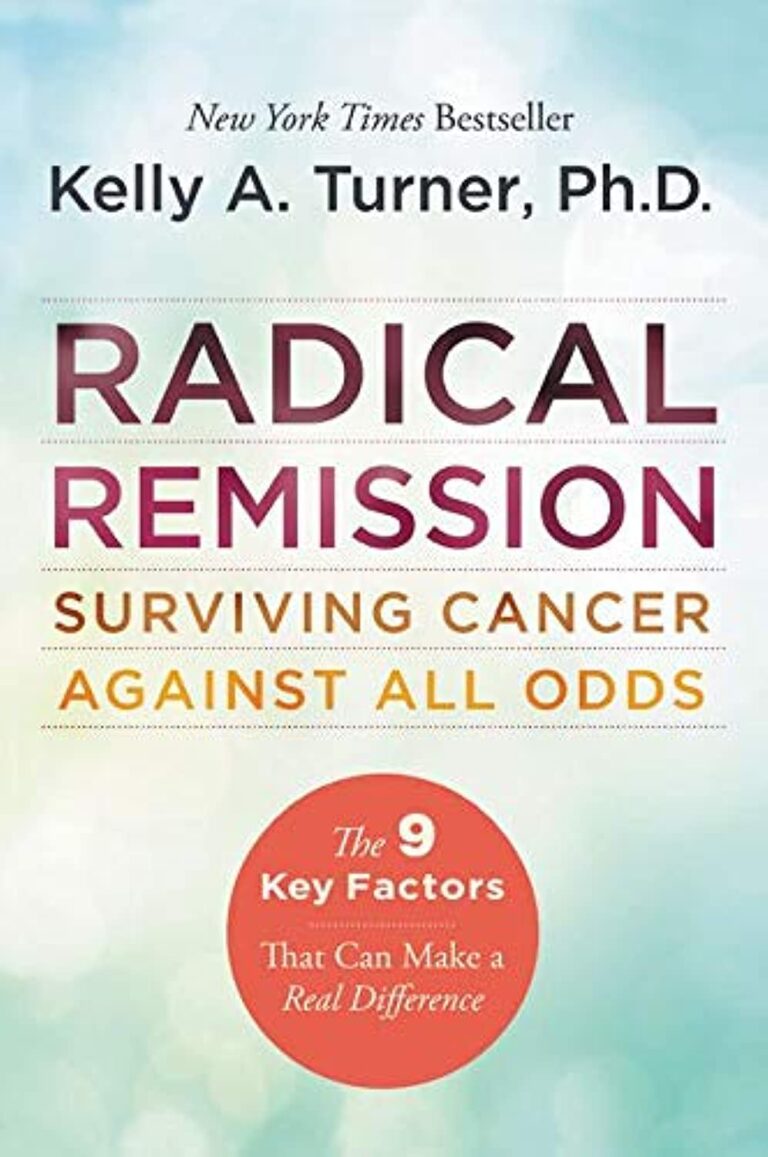
Learning to Love Midlife – by Chip Conley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While the book is titled about midlife, it could have said: midlife and beyond.
Some of the benefits discussed in this book really only kick in during one’s 50s, 60s, or 70s, usually. Which, for all but the most optimistic, is generally considered to be stretching beyond what is usually called “midlife”.
However! Chip Conley makes the argument for midlife being anywhere from one’s early 30s to mid-70s, depending on what (and how) we’re doing in life.
He talks about (as the subtitle promises) 12 reasons life gets better with age, and those reasons are grouped into 5 categories, thus:
- Physical life
- Emotional life
- Mental life
- Vocational life
- Spiritual life
It may surprise some readers that there are physical benefits that come with aging, but we do get two chapters in that category.
The writing style is very casual, yet with references to science throughout, and a bibliography for such.
Bottom line: if you’d like to make sure you’re making the most of your midlife and beyond, this a book that offers a lot of guidance on doing so!
Click here to check out Learning to Love Midlife, and age in style!
Share This Post
-
Peas vs Green Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peas to green beans, we picked the peas.
Why?
Looking at macros first, peas have nearly 6x the protein, nearly 2x the fiber, and nearly 2x the carbs, making them the “more food per food” choice.
In terms of vitamins, peas have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, and choline, while green beans have more of vitamins E and K. An easy win for peas.
In the category of minerals, peas have more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while green beans have more calcium. Another overwhelming win for peas.
In short, enjoy both (diversity is good), but there’s a clear winner here and it’s peas.
Want to learn more?
You might like to read:
Peas vs Broad Beans – Which is Healthier?
Take care!
Share This Post
-
How a Friend’s Death Turned Colorado Teens Into Anti-Overdose Activists
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Gavinn McKinney loved Nike shoes, fireworks, and sushi. He was studying Potawatomi, one of the languages of his Native American heritage. He loved holding his niece and smelling her baby smell. On his 15th birthday, the Durango, Colorado, teen spent a cold December afternoon chopping wood to help neighbors who couldn’t afford to heat their homes.
McKinney almost made it to his 16th birthday. He died of fentanyl poisoning at a friend’s house in December 2021. His friends say it was the first time he tried hard drugs. The memorial service was so packed people had to stand outside the funeral home.
Now, his peers are trying to cement their friend’s legacy in state law. They recently testified to state lawmakers in support of a bill they helped write to ensure students can carry naloxone with them at all times without fear of discipline or confiscation. School districts tend to have strict medication policies. Without special permission, Colorado students can’t even carry their own emergency medications, such as an inhaler, and they are not allowed to share them with others.
“We realized we could actually make a change if we put our hearts to it,” said Niko Peterson, a senior at Animas High School in Durango and one of McKinney’s friends who helped write the bill. “Being proactive versus being reactive is going to be the best possible solution.”
Individual school districts or counties in California, Maryland, and elsewhere have rules expressly allowing high school students to carry naloxone. But Jon Woodruff, managing attorney at the Legislative Analysis and Public Policy Association, said he wasn’t aware of any statewide law such as the one Colorado is considering. Woodruff’s Washington, D.C.-based organization researches and drafts legislation on substance use.
Naloxone is an opioid antagonist that can halt an overdose. Available over the counter as a nasal spray, it is considered the fire extinguisher of the opioid epidemic, for use in an emergency, but just one tool in a prevention strategy. (People often refer to it as “Narcan,” one of the more recognizable brand names, similar to how tissues, regardless of brand, are often called “Kleenex.”)
The Biden administration last year backed an ad campaign encouraging young people to carry the emergency medication.
Most states’ naloxone access laws protect do-gooders, including youth, from liability if they accidentally harm someone while administering naloxone. But without school policies explicitly allowing it, the students’ ability to bring naloxone to class falls into a gray area.
Ryan Christoff said that in September 2022 fellow staff at Centaurus High School in Lafayette, Colorado, where he worked and which one of his daughters attended at the time, confiscated naloxone from one of her classmates.
“She didn’t have anything on her other than the Narcan, and they took it away from her,” said Christoff, who had provided the confiscated Narcan to that student and many others after his daughter nearly died from fentanyl poisoning. “We should want every student to carry it.”
Boulder Valley School District spokesperson Randy Barber said the incident “was a one-off and we’ve done some work since to make sure nurses are aware.” The district now encourages everyone to consider carrying naloxone, he said.
Community’s Devastation Turns to Action
In Durango, McKinney’s death hit the community hard. McKinney’s friends and family said he didn’t do hard drugs. The substance he was hooked on was Tapatío hot sauce — he even brought some in his pocket to a Rockies game.
After McKinney died, people started getting tattoos of the phrase he was known for, which was emblazoned on his favorite sweatshirt: “Love is the cure.” Even a few of his teachers got them. But it was classmates, along with their friends at another high school in town, who turned his loss into a political movement.
“We’re making things happen on behalf of him,” Peterson said.
The mortality rate has spiked in recent years, with more than 1,500 other children and teens in the U.S. dying of fentanyl poisoning the same year as McKinney. Most youth who die of overdoses have no known history of taking opioids, and many of them likely thought they were taking prescription opioids like OxyContin or Percocet — not the fake prescription pills that increasingly carry a lethal dose of fentanyl.
“Most likely the largest group of teens that are dying are really teens that are experimenting, as opposed to teens that have a long-standing opioid use disorder,” said Joseph Friedman, a substance use researcher at UCLA who would like to see schools provide accurate drug education about counterfeit pills, such as with Stanford’s Safety First curriculum.
Allowing students to carry a low-risk, lifesaving drug with them is in many ways the minimum schools can do, he said.
“I would argue that what the schools should be doing is identifying high-risk teens and giving them the Narcan to take home with them and teaching them why it matters,” Friedman said.
Writing in The New England Journal of Medicine, Friedman identified Colorado as a hot spot for high school-aged adolescent overdose deaths, with a mortality rate more than double that of the nation from 2020 to 2022.
“Increasingly, fentanyl is being sold in pill form, and it’s happening to the largest degree in the West,” said Friedman. “I think that the teen overdose crisis is a direct result of that.”
If Colorado lawmakers approve the bill, “I think that’s a really important step,” said Ju Nyeong Park, an assistant professor of medicine at Brown University, who leads a research group focused on how to prevent overdoses. “I hope that the Colorado Legislature does and that other states follow as well.”
Park said comprehensive programs to test drugs for dangerous contaminants, better access to evidence-based treatment for adolescents who develop a substance use disorder, and promotion of harm reduction tools are also important. “For example, there is a national hotline called Never Use Alone that anyone can call anonymously to be supervised remotely in case of an emergency,” she said.
Taking Matters Into Their Own Hands
Many Colorado school districts are training staff how to administer naloxone and are stocking it on school grounds through a program that allows them to acquire it from the state at little to no cost. But it was clear to Peterson and other area high schoolers that having naloxone at school isn’t enough, especially in rural places.
“The teachers who are trained to use Narcan will not be at the parties where the students will be using the drugs,” he said.
And it isn’t enough to expect teens to keep it at home.
“It’s not going to be helpful if it’s in somebody’s house 20 minutes outside of town. It’s going to be helpful if it’s in their backpack always,” said Zoe Ramsey, another of McKinney’s friends and a senior at Animas High School.
“We were informed it was against the rules to carry naloxone, and especially to distribute it,” said Ilias “Leo” Stritikus, who graduated from Durango High School last year.
But students in the area, and their school administrators, were uncertain: Could students get in trouble for carrying the opioid antagonist in their backpacks, or if they distributed it to friends? And could a school or district be held liable if something went wrong?
He, along with Ramsey and Peterson, helped form the group Students Against Overdose. Together, they convinced Animas, which is a charter school, and the surrounding school district, to change policies. Now, with parental permission, and after going through training on how to administer it, students may carry naloxone on school grounds.
Durango School District 9-R spokesperson Karla Sluis said at least 45 students have completed the training.
School districts in other parts of the nation have also determined it’s important to clarify students’ ability to carry naloxone.
“We want to be a part of saving lives,” said Smita Malhotra, chief medical director for Los Angeles Unified School District in California.
Los Angeles County had one of the nation’s highest adolescent overdose death tallies of any U.S. county: From 2020 to 2022, 111 teens ages 14 to 18 died. One of them was a 15-year-old who died in a school bathroom of fentanyl poisoning. Malhotra’s district has since updated its policy on naloxone to permit students to carry and administer it.
“All students can carry naloxone in our school campuses without facing any discipline,” Malhotra said. She said the district is also doubling down on peer support and hosting educational sessions for families and students.
Montgomery County Public Schools in Maryland took a similar approach. School staff had to administer naloxone 18 times over the course of a school year, and five students died over the course of about one semester.
When the district held community forums on the issue, Patricia Kapunan, the district’s medical officer, said, “Students were very vocal about wanting access to naloxone. A student is very unlikely to carry something in their backpack which they think they might get in trouble for.”
So it, too, clarified its policy. While that was underway, local news reported that high school students found a teen passed out, with purple lips, in the bathroom of a McDonald’s down the street from their school, and used Narcan to revive them. It was during lunch on a school day.
“We can’t Narcan our way out of the opioid use crisis,” said Kapunan. “But it was critical to do it first. Just like knowing 911.”
Now, with the support of the district and county health department, students are training other students how to administer naloxone. Jackson Taylor, one of the student trainers, estimated they trained about 200 students over the course of three hours on a recent Saturday.
“It felt amazing, this footstep toward fixing the issue,” Taylor said.
Each trainee left with two doses of naloxone.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
I’ve been diagnosed with cancer. How do I tell my children?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With around one in 50 adults diagnosed with cancer each year, many people are faced with the difficult task of sharing the news of their diagnosis with their loved ones. Parents with cancer may be most worried about telling their children.
It’s best to give children factual and age-appropriate information, so children don’t create their own explanations or blame themselves. Over time, supportive family relationships and open communication help children adjust to their parent’s diagnosis and treatment.
It’s natural to feel you don’t have the skills or knowledge to talk with your children about cancer. But preparing for the conversation can improve your confidence.
Benjamin Manley/Unsplash Preparing for the conversation
Choose a suitable time and location in a place where your children feel comfortable. Turn off distractions such as screens and phones.
For teenagers, who can find face-to-face conversations confronting, think about talking while you are going for a walk.
Consider if you will tell all children at once or separately. Will you be the only adult present, or will having another adult close to your child be helpful? Another adult might give your children a person they can talk to later, especially to answer questions they might be worried about asking you.
Choose the time and location when your children feel comfortable. Craig Adderley/Pexels Finally, plan what to do after the conversation, like doing an activity with them that they enjoy. Older children and teenagers might want some time alone to digest the news, but you can suggest things you know they like to do to relax.
Also consider what you might need to support yourself.
Preparing the words
Parents might be worried about the best words or language to use to make sure the explanations are at a level their child understands. Make a plan for what you will say and take notes to stay on track.
The toughest part is likely to be saying to your children that you have cancer. It can help to practise saying those words out aloud.
Ask family and friends for their feedback on what you want to say. Make use of guides by the Cancer Council, which provide age-appropriate wording for explaining medical terms like “cancer”, “chemotherapy” and “tumour”.
Having the conversation
Being open, honest and factual is important. Consider the balance between being too vague, and providing too much information. The amount and type of information you give will be based on their age and previous experiences with illness.
Remember, if things don’t go as planned, you can always try again later.
Start by telling your children the news in a few short sentences, describing what you know about the diagnosis in language suitable for their age. Generally, this information will include the name of the cancer, the area of the body affected and what will be involved in treatment.
Let them know what to expect in the coming weeks and months. Balance hope with reality. For example:
The doctors will do everything they can to help me get well. But, it is going to be a long road and the treatments will make me quite sick.
Check what your child knows about cancer. Young children may not know much about cancer, while primary school-aged children are starting to understand that it is a serious illness. Young children may worry about becoming unwell themselves, or other loved ones becoming sick.
Young children might worry about other loved ones becoming sick. Pixabay/Pexels Older children and teenagers may have experiences with cancer through other family members, friends at school or social media.
This process allows you to correct any misconceptions and provides opportunities for them to ask questions. Regardless of their level of knowledge, it is important to reassure them that the cancer is not their fault.
Ask them if there is anything they want to know or say. Talk to them about what will stay the same as well as what may change. For example:
You can still do gymnastics, but sometimes Kate’s mum will have to pick you up if I am having treatment.
If you can’t answer their questions, be OK with saying “I’m not sure”, or “I will try to find out”.
Finally, tell children you love them and offer them comfort.
How might they respond?
Be prepared for a range of different responses. Some might be distressed and cry, others might be angry, and some might not seem upset at all. This might be due to shock, or a sign they need time to process the news. It also might mean they are trying to be brave because they don’t want to upset you.
Children’s reactions will change over time as they come to terms with the news and process the information. They might seem like they are happy and coping well, then be teary and clingy, or angry and irritable.
Older children and teenagers may ask if they can tell their friends and family about what is happening. It may be useful to come together as a family to discuss how to inform friends and family.
What’s next?
Consider the conversation the first of many ongoing discussions. Let children know they can talk to you and ask questions.
Resources might also help; for example, The Cancer Council’s app for children and teenagers and Redkite’s library of free books for families affected by cancer.
If you or other adults involved in the children’s lives are concerned about how they are coping, speak to your GP or treating specialist about options for psychological support.
Cassy Dittman, Senior Lecturer/Head of Course (Undergraduate Psychology), Research Fellow, Manna Institute, CQUniversity Australia; Govind Krishnamoorthy, Senior Lecturer, School of Psychology and Wellbeing, Post Doctoral Fellow, Manna Institute, University of Southern Queensland, and Marg Rogers, Senior Lecturer, Early Childhood Education; Post Doctoral Fellow, Manna Institute, University of New England
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fermenting Everything – by Andy Hamilton
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is not justanother pickling book! This is, instead, what it says on the front cover, “fermenting everything”.
Ok, maybe not literally everything, but every kind of thing that can reasonably be fermented, and it’s probably a lot more things than you might think.
From habanero chutney to lacto-lemonade, aioli to kombucha, Ukrainian fermented tomatoes to kvass. We could go on, but we’d soon run out of space. You get the idea. If it’s a fermented product (food, drink, condiment) and you’ve heard of it, there’s probably a recipe in here.
All in all, this is a great way to get in your gut-healthy daily dose of fermented products!
He does also talk safety, and troubleshooting too. And so long as you have a collection of big jars and a fairly normally-furnished kitchen, you shouldn’t need any more special equipment than that, unless you decide to you your fermentation skills for making beer (which does need some extra equipment, and he offers advice on that—our advice as a health science publication is “don’t drink beer”, though).
Bottom line: with this in hand, you can create a lot of amazing foods/drinks/condiments that are not only delicious, but also great for gut health.
Click here to check out Fermenting Everything, and widen your culinary horizons!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Celery vs Rhubarb – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to rhubarb, we picked the rhubarb.
Why?
In terms of macros, rhubarb has more carbs and fiber, the ratio of which give it the lower glycemic index, though both are low glycemic index foods. This means this category is a very marginal win for rhubarb.
When it comes to vitamins, rhubarb has more vitamin C, while celery has more of vitamins A, B5, B6, and B9. A win for celery, this time.
In the category of minerals, rhubarb has more calcium, iron, magnesium, manganese, potassium, and selenium, while celery has more copper and phosphorus. This one’s a win for rhubarb.
Let’s give a quick nod also to polyphenols; rhubarb has more by overall quantity, and more in terms of “more useful to humans” too, being rich in an assortment of flavanols while celery must make do with some furanocoumarins.
In short, enjoy either or both, but nutritional density is a great reason to get some rhubarb in!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: