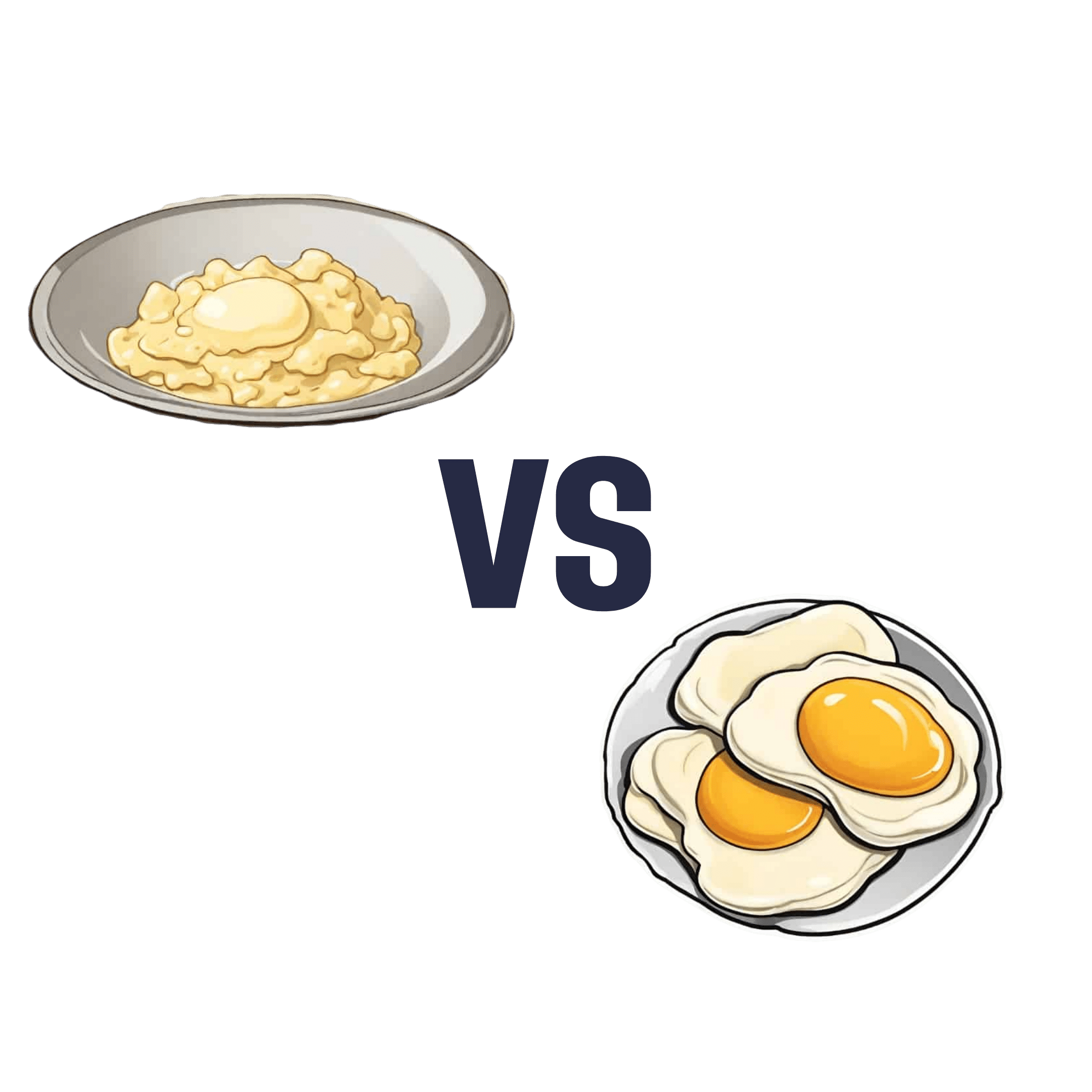
Egg Whites vs Whole Eggs – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing egg whites to whole eggs, we picked the whole eggs.
Why?
Egg whites are mostly protein. Egg yolks are mostly fat, with some protein.
However, fat ≠ bad, and the yolk is also where the choline is stored, which itself (as well as its benefits for your brain) will tend to reduce fat storage in the body.
Furthermore, the yolk contains an assortment of vitamins, minerals, and essential amino acids. After all, the yolk is there specifically to contain everything needed to turn a cluster of cells into a small bird.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The End of Old Age – by Dr. Marc Agronin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is not: a book about ending aging. For that, you would want to check out “Ending Aging”, by Dr. Aubrey de Grey.
What this book actually is: a book about the purpose of aging. As in: “aging: to what end?”, and then the book answers that question.
Rather than viewing aging as solely a source of decline, this book (while not shying away from that) resolutely examines the benefits of old age—from clinically defining wisdom, to exploring the many neurological trade-offs (e.g., “we lose this thing but we get this other thing in the process”), and the assorted ways in which changes in our brain change our role in society, without relegating us to uselessness—far from it!
The style of the book is deep and meaningful prose throughout. Notwithstanding the author’s academic credentials and professional background in geriatric psychiatry, there’s no hard science here, just comprehensible explanations of psychiatry built into discussions that are often quite philosophical in nature (indeed, the author additionally has a degree in psychology and philosophy, and it shows).
Bottom line: if you’d like your own aging to be something you understand better and can actively work with rather than just having it happen to you, then this is an excellent book for you.
Share This Post
-
How to Prevent Dementia – by Dr. Richard Restak
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written about this topic here, we know. But there’s a lot more we can do to be on guard against, and pre-emptively strengthen ourselves against, dementia.
The author, a neurologist, takes us on a detailed exploration of dementia in general, with a strong focus on Alzheimer’s in particular, as that accounts for more than half of all dementia cases.
But what if you can’t avoid it? It could be that with the wrong genes and some other factor(s) outside of your control, it will get you if something else doesn’t get you first.
Rather than scaremongering, Dr. Restak tackles this head-on too, and discusses how symptoms can be managed, to make the illness less anxiety-inducing, and look to maintain quality of life as much as possible.
The style of the book is… it reads a lot like an essay compilation. Good essays, then organized and arranged in a sensible order for reading, but distinct self-contained pieces. There are ten or eleven chapters (depending on how we count them), each divided into few or many sections. All this makes for:
- A very “read a bit now and a bit later and a bit the next day” book, if you like
- A feeling of a very quick pace, if you prefer to sit down and read it in one go
Either way, it’s a very informative read.
Bottom line: if you’d like to better understand the many-headed beast that is dementia, this book gives a far more comprehensive overview than we could here, and also explains the prophylactic interventions available.
Share This Post
-
Mineral-Rich Mung Bean Pancakes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mung beans are rich in an assortment of minerals, especially iron, copper, phosphorus, and magnesium. They’re also full of protein and fiber! What better way to make pancakes healthy?
You will need
- ½ cup dried green mung beans
- ½ cup chopped fresh parsley
- ½ cup chopped fresh dill
- ¼ cup uncooked wholegrain rice
- ¼ cup nutritional yeast
- 1 tsp MSG, or 2 tsp low-sodium salt
- 2 green onions, finely sliced
- 1 tbsp extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Soak the mung beans and rice together overnight.
2) Drain and rinse, and blend them in a blender with ¼ cup of water, to the consistency of regular pancake batter, adding more water (sparingly) if necessary.
3) Transfer to a bowl and add the rest of the ingredients except for the olive oil, which latter you can now heat in a skillet over a medium-high heat.
4) Add a few spoonfuls of batter to the pan, depending on how big you want the pancakes to be. Cook on both sides until you get a golden-brown crust, and repeat for the rest of the pancakes.
5) Serve! As these are savory pancakes, you might consider serving them with a little salad—tomatoes, olives, and cucumbers go especially well.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- What’s The Deal With MSG?
- All About Olive Oils: Is “Extra Virgin” Worth It?
Take care!
Share This Post
Related Posts
-
Gut Feelings – by Dr Will Cole
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More and more, science is uncovering links between our gut health and the rest of our health—including our mental health! We all know “get some fiber and consider probiotics”, but what else is there that we can do?
Quite a lot, actually. And part of it, which Dr. Cole also explores, is the fact that the gut-brain highway is a two-way street!
The book looks a lot especially at the particular relationship between shame and eating. The shame need not initially be about eating, though it can certainly end up that way too. But any kind of shame—be it relating to one’s body, work, relationship, or anything else, can not only have a direct effect on the gut, but indirect too:
Once our “eating our feelings” instinct kicks in, things can spiral from there, after all.
So, Dr. Cole walks us through tackling this from both sides—nutrition and psychology. With chapters full of tips and tricks, plus a 21-day plan (not a diet plan, a habit integration plan), this book hits shame (and inflammation, incidentally) hard and leads us into much healthier habits and cycles.
In short: if you’d like to have a better relationship with your food, improve your gut health, and/or reduce inflammation, this is definitely a book for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why You Probably Need More Sleep
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sleep: yes, you really do still need it!
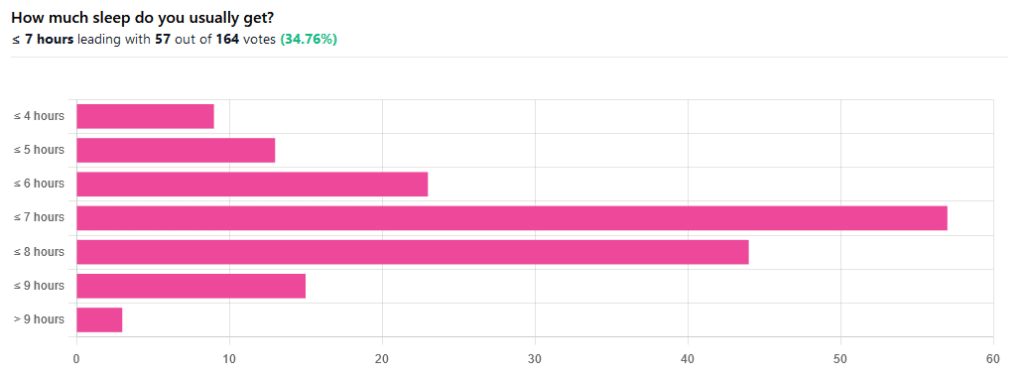
We asked you how much sleep you usually get, and got the above-pictured, below-described set of responses:
- A little of a third of all respondents selected the option “< 7 hours”
- However, because respondents also selected options such as < 6 hours, < 5 hours, and < 4 hours, so if we include those in the tally, the actual total percentage of respondents who reported getting under 7 hours, is actually more like 62%, or just under two thirds of all respondents.
- Nine respondents, which was about 5% of the total, reported usually getting under 4 hours sleep
- A little over quarter of respondents reported usually getting between 7 and 8 hours sleep
- Fifteen respondents, which was a little under 10% of the total, reported usually getting between 8 and 9 hours of sleep
- Three respondents, which was a little under 2% of the total, reported getting over 9 hours of sleep
- In terms of the classic “you should get 7–9 hours sleep”, approximately a third of respondents reported getting this amount.
You need to get 7–9 hours sleep: True or False?
True! Unless you have a (rare!) mutated ADRB1 gene, which reduces that.
The way to know whether you have this, without genomic testing to know for sure, is: do you regularly get under 6.5 hours sleep, and yet continue to go through life bright-eyed and bushy-tailed? If so, you probably have that gene. If you experience daytime fatigue, brain fog, and restlessness, you probably don’t.
About that mutated ADRB1 gene:
NIH | Gene identified in people who need little sleep
Quality of sleep matters as much as duration, and a lot of studies use the “RU-Sated” framework, which assesses six key dimensions of sleep that have been consistently associated with better health outcomes. These are:
- regularity / usual hours
- satisfaction with sleep
- alertness during waking hours
- timing of sleep
- efficiency of sleep
- duration of sleep
But, that doesn’t mean that you can skimp on the last one if the others are in order. In fact, getting a good 7 hours sleep can reduce your risk of getting a cold by three or four times (compared with six or fewer hours):
Behaviorally Assessed Sleep and Susceptibility to the Common Cold
^This study was about the common cold, but you may be aware there are more serious respiratory viruses freely available, and you don’t want those, either.
Napping is good for the health: True or False?
True or False, depending on how you’re doing it!
If you’re trying to do it to sleep less in total (per polyphasic sleep scheduling), then no, this will not work in any sustainable fashion and will be ruinous to the health. We did a Mythbusting Friday special on specifically this, a while back:
Could Just Two Hours Sleep Per Day Be Enough?
PS: you might remember Betteridge’s Law of Headlines
If you’re doing it as a energy-boosting supplement to a reasonable night’s sleep, napping can indeed be beneficial to the health, and can give benefits such as:
- Increased alertness
- Helps with learning
- Improved memory
- Boost to immunity
- Enhance athletic performance
However! There is still a right and a wrong way to go about it, and we wrote about this previously, for a Saturday Life Hacks edition of 10almonds:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
As we get older, we need less sleep: True or False
False, with one small caveat.
The small caveat: children and adolescents need 9–12 hours sleep because, uncredited as it goes, they are doing some seriously impressive bodybuilding, and that is exhausting to the body. So, an adult (with a normal lifestyle, who is not a bodybuilder) will tend to need less sleep than a child/adolescent.
But, the statement “As we get older, we need less sleep” is generally taken to mean “People in the 65+ age bracket need less sleep than younger adults”, and this popular myth is based on anecdotal observational evidence: older people tend to sleep less (as our survey above shows! For any who aren’t aware, our readership is heavily weighted towards the 60+ demographic), and still continue functioning, after all.
Just because we survive something with a degree of resilience doesn’t mean it’s good for us.
In fact, there can be serious health risks from not getting enough sleep in later years, for example:
Sleep deficiency promotes Alzheimer’s disease development and progression
Want to get better sleep?
What gets measured, gets done. Sleep tracking apps can be a really good tool for getting one’s sleep on a healthier track. We compared and contrasted some popular ones:
The Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
Take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Curing Hiccups And Headaches At Home With Actual Science
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Quick fixes for bodily annoyances
Do you ever find yourself desperately trying to cure hiccups, and advice on the Internet is like “breathe in through your ears while drinking vinegar upside-down through your nose”?
If so, you’re not alone. So, today we’re going to look at some science-based approaches to dealing with common bodily annoyances.
Hiccups
Unfortunately, most popular advices simply don’t work, and the only near-guaranteed way to cure these is with anti-convulsive medications whose side-effects may be worse than the hiccups.
However, before you head to the pharmacy, there is one breathing exercise that has a very simple scientific underpinning: 4:4 breathing. If you’re unfamiliar, it’s just:
- Breathe slowly in through your nose to a count of four
- Hold your breath for a count of four
- Breathe slowly out through your nose to a count of four
- Hold your breath for a count of four
…and repeat. The slower the better. At first, your hiccups will interrupt this, but just “keep calm and carry on”.
The reason this can work is that breathing is an autonomic function (e.g., it happens without us thinking about it) that, unlike most other autonomic functions, we can all control directly. By taking control of one, others will tend to fall into line with it.
For example, it is normal that your heart rate will tend to slow or quicken as your breathing slows or quickens, respectively.
Your hiccups? Autonomic function. Actually a very, very old evolutionary left-over trait, that’s only useful for protecting lungs while breathing underwater. In other words, it’s the bodily function thinks you’re a fish (or a tadpole-like amphibious creature) in the process of developing lungs. Unfortunately, because hiccuping doesn’t harm our chances of passing on our genes, it never got naturally de-selected so we still have it.
Anyway, the bottom line is: take control of your breathing in the aspects you can directly control, and the aspects you can’t directly control will fall into line. You may need to give it some minutes, don’t give up too quickly.
Headaches
If you ever get a headache and you don’t have painkillers or perhaps they’re not helping or you have another reason for not wanting to take them, there’s “one quick trick” that can cure most headaches in seconds.
First, the limitation: this will only cure headaches that have been caused by increased localized blood pressure in the forehead. However, that’s more than half of most common headaches.
Next, how it works…
We’re mentioning this first, because understanding how it works will give you more confidence in using it.
Your body has a wonderful homeostatic system, which is the system by which your body maintains its “Goldilocks zones” of not too hot or cold, not to acidine or alkaline, not too hydrated or dehydrated, blood pressure not too high or too low, etc. Sometimes, however, it can get confused, and needs a nudge back to where it should be.
One of the ways it maintains blood pressure is biofeedback from receptors in blood vessel walls, called baroreceptors. They are what it sounds like; they measure blood pressure internally.
In certain places, there are clusters of baroreceptors in one place. And if we press on that one place, the body will think “Oh no! Super high blood pressure in this bit!” and reduce the blood pressure immediately.
This is called the baroreflex, and that’s what you need to cure a hypertensive headache.
So, what to do:
With your thumb, carefully feel the upper inside corner of your eye socket. So, at the top, and about ¼ of the way out from the bridge of your nose. You should feel a groove. No, not like the Emperor’s New, but, an actual groove in your eye socket. That’s the supraorbital notch (or foramen), and it allows the supraorbital artery, veins, and nerve to run through.
Press it firmly (you can do both sides at once, assuming you have two thumbs) for about three seconds, and then massage it gently. Repeat as necessary, but it shouldn’t take more than about three goes to have cured the headache.
As a bonus, this is a great party trick for curing other people’s headaches, when the need arises!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: