Dodging Dengue In The US
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dengue On The Rise
We wrote recently about dengue outbreaks in the Americas, with Puerto Rico declaring an epidemic. Cases are now being reported in Florida too, and are likely to spread, so it’s good to be prepared, if your climate is of the “warm and humid” kind.
If you want to catch up on the news first, here you go:
- UN health agency cites tenfold increase in reported cases of dengue over the last generation
- Puerto Rico has declared an epidemic following a spike in dengue cases
- Dengue fever confirmed in Florida Keys as US on watch for rise in mosquito illness
Note: dengue is far from unheard of in Florida, but the rising average temperatures in each year mean that each year stands a good chance of seeing more cases than the previous. It’s been climbing since at least 2017, took a dip during the time of COVID restrictions keeping people at home more, and then for the more recent years has been climbing again since.
What actually is it?
Dengue is a viral, mosquito-borne disease, characterized by fever, vomiting, muscle pain, and a rash, in about 1 in 4 cases.
Which can sound like “you’ll know if you have it”, but in fact it’s usually asymptomatic for a week or more after infection, so, watch out!
What next, if those symptoms appear?
The good news is: the fever will usually last less than a week
The bad news is: a day or so after that the fever subsided, the more serious symptoms are likely to start—if they’re going to.
If you’re unlucky enough to be one of the 1 in 20 who get the serious symptoms, then you can expect abdominal cramps, repeat vomiting, bleeding from various orifices (you may not get them all, but all are possible), and (hardly surprising, given the previous items) “extreme fatigue and restlessness”.
If you get those symptoms, then definitely get to an ER as soon as possible, as dengue can become life-threatening within hours of such.
Read more: CDC | Symptoms of Dengue and Testing
While there is not a treatment for dengue per se, the Emergency Room will be better able to manage your symptoms and thus keep you alive long enough for them to pass.
If you’d like much more detail (on symptoms, seriousness, at-risk demographics, and prognosis) than what the CDC offers, then…
Read more: BMJ | Dengue Fever
Ok, so how do we dodge the dengue?
It sounds flippant to say “don’t get bitten”, but that’s it. However, there are tips are not getting bitten:
- Use mosquito-repellent, but it has to contain >20% DEET, so check labels
- Use mosquito nets where possible (doors, windows, etc, and the classic bed-tent net is not a bad idea either)
- Wear clothing that covers your skin, especially during the day—it can be light clothing; it doesn’t need to be a HazMat suit! But it does need to reduce the area of attack to reduce the risk of bites.
- Limit standing water around your home—anything that can hold even a small amount of standing water is a potential mosquito-breeding ground. Yes, even if it’s a crack in your driveway or a potted bromeliad.
Further reading
You might also like to check out:
Stickers and wristbands aren’t a reliable way to prevent mosquito bites. Here’s why
…and in case dengue wasn’t bad enough:
Mosquitoes can spread the flesh-eating Buruli ulcer. Here’s how you can protect yourself
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Meningitis Outbreak
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Don’t Let Your Guard Down
In the US, meningitis is currently enjoying a 10-year high, with its highest levels of infection since 2014.
This is a big deal, given the 10–15% fatality rate of meningitis, even with appropriate medical treatment.
But of course, not everyone gets appropriate medical treatment, especially because symptoms can become life-threatening in a matter of hours.
Most recent stats gave an 18% fatality rate for the cases with known outcomes in the last year:
CDC Emergency | Increase in Invasive Serogroup Y Meningococcal Disease in the United States
The quick facts:
❝Meningococcal disease most often presents as meningitis, with symptoms that may include fever, headache, stiff neck, nausea, vomiting, photophobia, or altered mental status.
[It can also present] as meningococcal bloodstream infection, with symptoms that may include fever and chills, fatigue, vomiting, cold hands and feet, severe aches and pains, rapid breathing, diarrhea, or, in later stages, a dark purple rash.
While initial symptoms of meningococcal disease can at first be non-specific, they worsen rapidly, and the disease can become life-threatening within hours. Immediate antibiotic treatment for meningococcal disease is critical.
Survivors may experience long-term effects such as deafness or amputations of the extremities.❞
~ Ibid.
The good news (but still don’t let your guard down)
Meningococcal bacteria are, happily, not spread as easily as cold and flu viruses.
The greatest risks come from:
- Close and enduring proximity (e.g. living together)
- Oral, or close-to-oral, contact (e.g. kissing, or coughing nearby)
Read more:
CDC | Meningococcal Disease: Causes & How It Spreads
Is there a vaccine?
There is, but it’s usually only offered to those most at risk, which is usually:
- Children
- Immunocompromised people, especially if HIV+
- People taking certain medications (e.g. Solaris or Ultomiris)
Read more:
CDC | Meningococcal Vaccine Recommendations
Will taking immune-boosting supplements help?
Honestly, probably not, but they won’t harm either. The most important thing is: don’t rely on them—too many people pop a vitamin C supplement and then assume they are immune to everything, and it doesn’t work like that.
On a tangential note, for more general immune health, you might also want to check out:
Beyond Supplements: The Real Immune-Boosters!
The short version:
If you or someone you know experiences the above-mentioned symptoms, even if it does not seem too bad, get thee/them to a doctor, and quickly, because the (very short) clock may be ticking already.
Better safe than sorry.
Share This Post
-
Food Expiration Dates Don’t Mean What Most People Think They Mean
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever wondered why rock salt that formed during the Precambrian era has a label on it saying that it expires next month? To take something more delicate, how about eggs that expire next Thursday; isn’t that oddly specific for something that is surely affected by many variables? What matters, and what doesn’t?
Covering their assets
The US in particular wastes huge amounts of food, with 37% of food waste coming from households. Confusion over date labels is a major contributor, accounting for 20% of household food waste. Many people misinterpret these labels, often discarding food that is still safe to eat—which is good for the companies selling the food, because then they get to sell you more.
Date labels were introduced in the 70s with the “open dating” system to indicate optimal freshness, not safety. These dates are often conservative, set by manufacturers to ensure food is consumed at its best quality and encourage repeat purchases. However, many foods remain safe well past their labeled dates, including shelf-stable items like pasta, rice, and canned goods, as well as frozen foods stored properly.
Some foods do pose safety risks, especially meat and dairy products, as well as many grain-based foods, all of which which can harbor harmful bacteria. Infant formula labels are strictly regulated for safety. However, most date labels are not linked to health risks, leading to unnecessary waste.
When it comes down to it, our senses of sight, smell, and taste are more reliable than dates on packaging. Some quick pointers and caveats:
- If it has changed color in some way that’s not associated with a healthily ripening fruit or vegetable, that’s probably bad
- If it is moldy, that’s probably bad (but the degree of badness varies from food to food; see the link beneath today’s video for more on that)
- If a container has developed droplets of water on the inside when it didn’t have those before, that’s probably bad (it means something is respiring, and is thus alive, that probably shouldn’t be)
- If it smells bad, that’s probably bad—however this is not a good safety test, because a bad smell may often mean you are inhaling mold spores, which are not good for your lungs.
- If it tastes different than that food usually does, that’s probably bad (especially if it became bitter, pungent, tangy, sour, or cheesy, and does nor normally taste that way).
Some places have trialled clearer labelling, for example a distinction between “expires” and merely “best before”, but public awareness about the distinction is low. Some places have trialled removing dates entirely, to oblige the consumer to use their own senses instead. This is good for the seller in a different way than household food waste is, because it means the seller will have less in-store waste (because they can still sell something that might previously have been labelled as expired).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
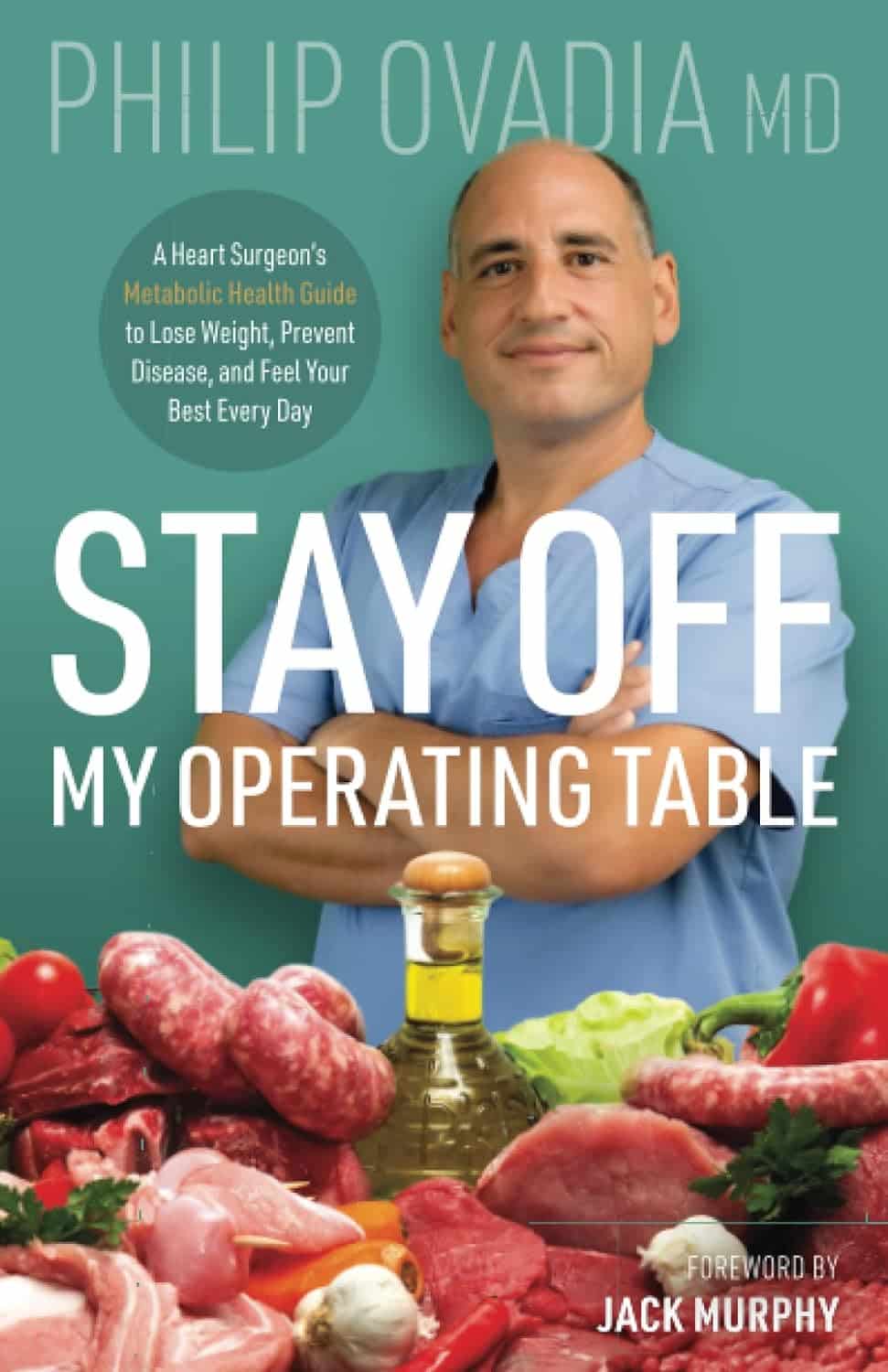
Stay off My Operating Table – by Dr. Philip Ovadia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With heart disease as the #1 killer worldwide, and 88% of adults being metabolically unhealthy (leading cause of heart disease), this is serious!
Rather than taking a “quick fix” advise-and-go approach, Dr. Ovadia puts the knowledge and tools in our hands to do better in the long term.
As a heart surgeon himself, his motto here is:
❝What foods to put on your table so you don’t end up on mine❞
There’s a lot more to this book than the simple “eat the Mediterranean diet”:
- While the Mediterranean diet is generally considered the top choice for heart health, he also advises on how to eat healthily on all manner of diets… Carnivore, Keto, Paleo, Atkins, Gluten-Free, Vegan, you-name-it.
- A lot of the book is given to clearing up common misconceptions, things that sounded plausible but are just plain dangerous. This information alone is worth the price of the book, we think.
- There’s also a section given over to explaining the markers of metabolic health, so you can monitor yourself effectively
- Rather than one-size-fits-all, he also talks about common health conditions and medications that may change what you need to be doing
- He also offers advice about navigating the health system to get what you need—including dealing with unhelpful doctors!
Bottom line: A very comprehensive (yet readable!) manual of heart health.
Get your copy of Stay Off My Operating Table from Amazon today!
Share This Post
Related Posts
-
It’s On Me – by Dr. Sara Kuburic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This isn’t about bootstrapping and nor is it a motivational pep talk. What it is, however, is a wake-up call for the wayward, and that doesn’t mean “disaffected youth” or such. Rather, therapist Dr. Sara Kuburic tackles the problem of self-loss.
It’s about when we get so caught up in what we need to do, should do, are expected to do, are in a rut of doing… That we forget to also live. After all, we only get one shot at life so far as we know, so we might as well live it in whatever way is right for us.
That probably doesn’t mean a life of going through the motions.
The writing style here is personal and direct, and it makes for quite compelling reading from start to finish.
Bottom line: if ever you find yourself errantly sleepwalking through life and would like to change that, this is a book for you.
Click here to check out It’s On Me, and take control of what’s yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Becoming a Supple Leopard – by Dr. Kelly Starrett and Glen Cordoza
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Starrett’s other book, “Built To Move“, and now today we’ll review his more famous book!
Why is this one so famous? It’s popularly considered “the Bible of Cross-Fit”, even though it’s not at all marketed as such, and nor does it talk about Cross Fit directly. But: people who are interested in being fit, fast, strong, mobile, stable, and so forth, tend to invest in this book at some point if they are serious.
The book is big, heavy, and textbook-like. This isn’t a quick light read. This is a “study over the course of a year or more while doing your physiotherapy degree” book. And yet, it’s written for the widest audience, and as such, everything is explained from the ground up, so no prior knowledge is expected.
It does have pictures, which are clear and helpful, though the print version is better for this than the Kindle edition.
The subtitle of the book is no lie; it does indeed cover all those things, deeply and at length, for everything musculoskeletal.
Bottom line: this book will seriously improve your knowledge and understanding of all things body mechanics and related body maintenance. If you care to get/remain fit/strong/mobile/etc, this book is a fine cornerstone for such endeavors.
Click here to check out Becoming A Supple Leopard, and become a supple leopard!*
*Metaphorically. Furry metamorphosis is not a side-effect. Suppleness, however, is on offer. Yes, even for you, dear reader!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s So Special About Alpha-Lipoic Acid?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Access-All-Areas Antioxidant
Alpha-Lipoic Acid (ALA) is one of the most bioavailable antioxidants in existence. A bold claim, but most antioxidants are only water-soluble or fat-soluble, whereas ALA is both. This has far-reaching implications—and we mean that literally, because its “go everywhere” status means that it can access (and operate in) all living cells of the human body.
We make it inside our body, and we can also get it in our diet, or take it as a supplement.
What foods contain it?
The richest food sources are:
- For the meat-eaters: organ meats
- For everyone: broccoli, tomatoes, & spinach
However, supplements are more efficient at delivering it, by several orders of magnitude:
Read more: Lipoic acid – biological activity and therapeutic potential
What are its benefits?
Most of its benefits are the usual benefits you would expect from any antioxidant, just, more of it. In particular, reduced inflammation and slowed skin aging are common reasons that people take ALA as a supplement.
Does it really reduce inflammation?
Yes, it does. This one’s not at all controversial, as this systematic review of studies shows:
(C-reactive protein is a marker of inflammation)
Does it really reduce skin aging?
Again yes—which again is not surprising for such a potent antioxidant; remember that oxidative stress is one of the main agonists of cellular aging:
As a special feature, ALA shows particular strength against sun-related skin aging, because of how it protects against UV radiation and increases levels of gluthianone, which also helps:
- Photochemical stability of lipoic acid and its impact on skin ageing
- Modern approach to topical treatment of aging skin
Where can I get some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: