Severe Complications for Pregnant Veterans Nearly Doubled in the Last Decade, a GAO Report Finds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: Post-Roe America:Abortion Access Divides the Nation
After the Supreme Court overturned Roe v. Wade, ending nearly 50 years of federal protection for abortion, some states began enforcing strict abortion bans while others became new havens for the procedure. ProPublica is investigating how sweeping changes to reproductive health care access in America are affecting people, institutions and governments.
Over the past decade, the rate of veterans suffering severe pregnancy complications has risen dramatically, a new federal report found.
Veterans have raced to the hospital with dangerous infections, kidney failure, aneurysms or blood loss. They’ve required hysterectomies, breathing machines and blood transfusions to save their lives. Between 2011 and 2020, 13 veterans died after such complications.
The report found that among people getting health care benefits through the Department of Veterans Affairs, the rate of severe complications nearly doubled during that time, from about 93 per 10,000 hospitalizations in 2011 to just over 184 per 10,000 hospitalizations in 2020. Black veterans had the highest rates.
The report, which was put together by the Government Accountability Office, also made recommendations for reducing the problem, which focus on conducting more routine screenings throughout pregnancy and in the postpartum period.
“It is imperative that the VA help ensure veterans have the healthiest pregnancy outcomes possible,” the report said, highlighting the increasing number of veterans using the agency’s maternity benefits as well as the troublesome complication rates faced by Black women.
The report’s findings are an unfortunate trend, said Alyssa Hundrup, director of health care at the GAO. The office analyzed data on 40,000 hospitalizations related to deliveries paid for by the VA. It captures a time period before 21 states banned or greatly restricted abortion and the military was thrust into a political battle over whether it would pay for active service members to travel for abortion care if a pregnancy was a risk to their health.
Hundrup, who led the review, said the analysis included hospital records from days after delivery to a year postpartum. The report was mandated after Congress passed a law in 2021 that aimed to address the maternal health crisis among veterans. The law led to a $15 million investment in maternity care coordination programs for veterans.
The report recommended that the VA analyze and collect more data on severe complications as well as data on the mental health, race and ethnicity of veterans who experience complications to understand the causes behind the increase and the reasons for the disparity. The report also states that oversight is needed to ensure screenings are being completed.
Studies show there’s a connection between mental health conditions and pregnancy-related complications, VA officials said.
The report recommended expanding the screening questions that providers ask patients at appointments to glean more information about their mental health, including anxiety and PTSD symptoms. It urged the VA to review the data more regularly.
“You don’t know what you don’t measure,” Hundrup said in an interview with ProPublica.
The VA health system, which historically served a male population, does not provide maternity care at its facilities. Instead, the agency has outsourced maternity care. But when patients were treated by those providers, the VA failed to track whether they were getting screened for other health issues and mental health problems.
Officials hope the improved data collection will help the VA study underlying issues that may lead to complications. For example, do higher rates of anxiety have a connection to rates of high blood pressure in pregnant people?
VA officials are working with a maternal health review committee to monitor the data as it is gathered. The agency recently conducted its first review of data going back five years about pregnancy-related complications, said Dr. Amanda Johnson, acting head of the VA’s Office of Women’s Health, who is overseeing the implementation of the report’s recommendations.
The VA has created a dashboard to monitor pregnant veterans’ health outcomes. The VA’s data analysis team will also examine the impact of veterans’ ages on complications and whether they differ for people who live in urban and rural areas.
VA officials will begin to review mental health screenings conducted by maternal care coordinators in March. The coordinators advocate for veterans, helping them between health care visits, whether their providers are inside or outside the VA.
Johnson said that reducing racial and ethnic disparities is a priority for the agency. In 2018, ProPublica published “Lost Mothers,” a series that shed light on the country’s maternal health crisis. Studies have shown that in the general population, Black women are three times more likely than white women to die from pregnancy-related complications. While deaths made up only a small portion of the bad outcomes for Black veterans cited in the report, VA care could not spare them from elevated rates of severe complications. Johnson said the maternal health crisis also persists within the VA.
“There is a disparity,” Johnson said. “We are not immune to that.”
Research shows pregnant people who have used the VA’s coverage have higher rates of trauma and mental conditions that can increase their risks of complications and bad outcomes.
This may be because many people who join the military enter it having already faced trauma, said Dr. Laura Miller, a psychiatrist and the medical director of reproductive mental health at the VA.
She said veterans with PTSD have higher rates of complications such as preeclampsia, a potentially fatal condition related to high blood pressure, gestational diabetes and postpartum depression. If untreated during pregnancy, depression also increases the likelihood of preterm birth and lingering problems for babies.
Hundrup said she hopes this proactive work will improve maternal health.
“We want these numbers trending in the other direction,” Hundrup said.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mythbusting Cookware Materials
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
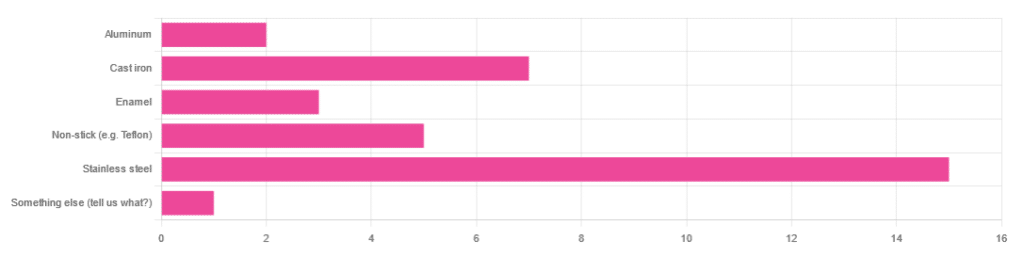
In Wednesday’s newsletter, we asked you what kind of cookware you mostly use, and got the above-depicted, below-described, set of responses:
- About 45% said stainless steel
- About 21% said cast iron
- About 15% said non-stick (e.g. Teflon)
- About 9% said enamel
- About 6% said aluminum
- And 1 person selected “something else”, but then commented to the contrary, writing “I use all of the above”
So, what does the science say about these options?
Stainless steel cookware is safe: True or False?
True! Assuming good quality and normal use, anyway. There really isn’t a lot to say about this, because it’s very unexciting. So long as it is what it is labelled as: there’s nothing coating it, nothing comes out of it unless you go to extremes*, and it’s easy to clean.
*If you cook for long durations at very high temperatures, it can leach nickel and chromium into food. What this means in practical terms: if you are using stainless steel to do deep-frying, then maybe stop that, and also consider going easy on deep-frying in general anyway, because obviously deep-frying is unhealthy for other reasons.
Per normal use, however: pretty much the only way (good quality) stainless steel cookware will harm you is if you touch it while it’s hot, or if it falls off a shelf onto your head.
That said, do watch out for cheap stainless steel cookware that can contain a lot of impurities, including heavy metals. Since you probably don’t have a mass spectrometer and/or chemistry lab at home to check for those impurities, your best guard here is simply to buy from a reputable brand with credible certifications.
Ceramic cookware is safe: True or False?
True… Most of the time! Ceramic pans usually have metal parts and a ceramic cooking surface coated with a very thin layer of silicon. Those metal parts will be as safe as the metals used, so if that’s stainless steel, you’re just as safe as the above. As for the silicon, it is famously inert and body-safe (which is why it’s used in body implants).
However: ceramic cookware that doesn’t have an obvious metal part and is marketed as being pure ceramic, will generally be sealed with some kind of glaze that can leach heavy metals contaminants into the food; here’s an example:
Lead toxicity from glazed ceramic cookware
Copper cookware is safe: True or False?
False! This is one we forgot to mention in the poll, as one doesn’t see a lot of it nowadays. The copper from copper pans can leach into food. Now, of course copper is an important mineral that we must get from our diet, but the amount of copper that that can leach into food from copper pans is far too much, and can induce copper toxicity.
In addition, copper cookware has been found to be, on average, highly contaminated with lead:
Non-stick cookware contaminates the food with microplastics: True or False?
True! If we were to discuss all the common non-stick contaminants here, this email would no longer fit (there’s a size limit before it gets clipped by most email services).
Suffice it to say: the non-stick coating, polytetrafluoroethylene, is itself a PFAS, that is to say, part of the category of chemicals considered environmental pollutants, and associated with a long list of health issues in humans (wherein the level of PFAS in our bloodstream is associated with higher incidence of many illnesses):
You may have noticed, of course, that the “non-stick” coating doesn’t stick very well to the pan, either, and will tend to come off over time, even if used carefully.
Also, any kind of wet cooking (e.g. saucepans, skillets, rice cooker inserts) will leach PFAS into the food. In contrast, a non-stick baking tray lined with baking paper (thus: a barrier between the tray and your food) is really not such an issue.
We wrote about PFAS before, so if you’d like a more readable pop-science article than the scientific paper above, then check out:
PFAS Exposure & Cancer: The Numbers Are High
Aluminum cookware contaminates the food with aluminum: True or False?
True! But not usually in sufficient quantities to induce aluminum toxicity, unless you are aluminum pans Georg who eats half a gram of aluminum per day, who is a statistical outlier and should not be counted.
That’s a silly example, but an actual number; the dose required for aluminum toxicity in blood is 100mg/L, and you have about 5 liters of blood.
Unless you are on kidney dialysis (because 95% of aluminum is excreted by the kidneys, and kidney dialysis solution can itself contain aluminum), you will excrete aluminum a lot faster than you can possibly absorb it from cookware. On the other hand, you can get too much of it from it being a permitted additive in foods and medications, for example if you are taking antacids they often have a lot of aluminum oxide in them—but that is outside the scope of today’s article.
However, aluminum may not be the real problem in aluminum pans:
❝In addition, aluminum (3.2 ± 0.25 to 4.64 ± 0.20 g/kg) and copper cookware (2.90 ± 0.12 g/kg) were highly contaminated with lead.
The time and pH-dependent study revealed that leaching of metals (Al, Pb, Ni, Cr, Cd, Cu, and Fe, etc.) into food was predominantly from anodized and non-anodized aluminum cookware.
More metal leaching was observed from new aluminum cookware compared to old. Acidic food was found to cause more metals to leach during cooking.❞
~ the same paper we cited when talking about copper
Cast iron cookware contaminates the food with iron: True or False?
True, but unlike with the other metals discussed, this is purely a positive, and indeed, it’s even recommended as a good way to fortify one’s diet with iron:
The only notable counterpoint we could find for this is if you have hemochromatosis, a disorder in which the body is too good at absorbing iron and holding onto it.
Thinking of getting some new cookware?
Here are some example products of high-quality safe materials on Amazon, but of course feel free to shop around:
Stainless Steel | Ceramic* | Cast Iron
*it says “non-stick” in the description, but don’t worry, it’s ceramic, not Teflon etc, and is safe
Bonus: rice cooker with stainless steel inner pot
Take care!
Share This Post
-
Stand Up For Your Health (Or Don’t)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may have heard the phrase “sitting is the new smoking”, and while the jury’s out on whether that’s accurate or not in terms of exactly how damaging it is, one thing that is universally agreed-upon is that sitting is indeed very bad.
It’s especially bad for your spine (because of being folded in ways it shouldn’t be), your muscles and associated nerves of the lower back and hip area, your abdominal organs (because of being compressed in ways they shouldn’t be), and your heart (because of arteries and veins being squashed up in ways they shouldn’t be), and if you remember how “what’s good for your heart is good for your brain”, the inverse is true, and what’s bad for your heart is also bad for your brain, which won’t get nourished with oxygen and nutrients and which won’t have its detritus removed as efficiently as it should; that’ll be left to build up in the brain instead.
First, elephant in the room: not everybody can stand, and of those who can, not everybody can stand for long. So obviously, work within what’s attainable for you.
Also note that while sitting is the disease-bringer/worsener, standing isn’t the only solution, for example:
- Walking is better than standing. You may be wondering: “who can’t stand but can walk?” and the answer is, a lot of people with certain kinds of chronic pain, for whom walking is less chronic-pain-exacerbating than standing, because the human body is built for movement and inactivity can worsen things even more than movement.
- See also: Managing Chronic Pain (Realistically)
- Lying down is better than sitting. One of the major problems with sitting is that your organs are all bunched up in ways they shouldn’t be. Lying down is, in this regard, closer to standing than sitting, because your body has a nice straight line to it.
- Sitting can be made less bad! For example:
- Sitting in a recliner chair in the reclined position is… Not great, if you’re then tilting your skull forwards to compensate, but if you’re just sitting back and relaxing, this is a lot better than sitting in the usual seated position, because again, it’s closer to lying down, which is closer to standing.
- Sitting in seiza (the traditional Japanese kneeling position) is, provided you do it correctly and with good posture, better than sitting in the traditional Western manner. The reason for this is simple: instead of having your torso and legs at 90°, they are at 120°ish, give or take the size of your thighs and butt (bigger being better in this regard), and even that angle can be made even better if you use a meditation bench like this one ← we’re eyeballing it and didn’t get out a protractor, but if you look at the model’s torso and thighs, that’s about 135° difference, which is huge improvement over the 90° you get while sitting Western-style.
For most of us a lot of the time though, we can stand to sit less. Think about the places you most often sit, and what can be done to reasonably minimize those, for example:
- Car: minimize driving (or being a passenger in a car); walk where reasonably possible. Public transport, if available, may have standing options.
- Office: a standing desk is, of course, the way to go. You can even use a standing desk converter, like this one. Just make sure to set it at the correct height, both in terms of where the keyboard and mouse go (the same height as your elbows are when your arms are dropped to your sides), and where the monitor goes (center of the monitor should be at eye-level).
- Note: laptops will never be right for this, unless the natural resting distance between your elbows and your eyes is about 4½ inches, which will only be the case if your total height is approximately 1 foot and 2 inches. For anyone taller than that, laptops are still great to have when on the move and as a backup, but not great for ergonomics.
- Workaround: if for some reason you must use a laptop for your day-to-day work, consider using a bluetooth keyboard so that you can still set them the appropriate height-distance apart and thus not have to hunch over them.
- Dining room: sitting to eat a main meal is reasonable, but consider standing options for lighter bites; a standing-height “brunch bar” is great if you can arrange one.
- Lounge: let it live up to its name, and actually lounge: if you’re not going to stand, then horizontal lounging is an improvement over sitting—as is sitting on the floor, and changing your position frequently. Who knew, kids had it right in that regard!
- Note: if, like this writer, you do a lot of reading, the same applies regardless of which room you’re doing it in.
- Bedroom: a culprit for many will be sitting while doing a beauty routine and/or possibly make-up. Easily avoided if you set a well-lit mirror at the correct height to use while standing.
- Note: at the correct height though! While hunching up over a wall-mounted mirror is an improvement over hunching up at a seated vanity, it’s not a great improvement. You want to be able to stand with good posture and do it comfortably.
- Bathroom: leave your phone outside—which is also a good approach for avoiding hemorrhoids! See also: Half Of Americans Over 50 Have Hemorrhoids, But They Can Be Prevented!
Want to know more?
We reviewed this book recently, which goes into all of the above in much more detail than we have room for here, plus also discusses a lot of social reframes that can be used (since a lot of sitting is a matter of social expectations, not actual need). It’s a very useful read:
Take care!
Share This Post
- Walking is better than standing. You may be wondering: “who can’t stand but can walk?” and the answer is, a lot of people with certain kinds of chronic pain, for whom walking is less chronic-pain-exacerbating than standing, because the human body is built for movement and inactivity can worsen things even more than movement.
-
Sweet Dreams Are Made Of Cheese (Or Are They?)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝In order to lose a little weight I have cut out cheese from my diet – and am finding that I am sleeping better. Would be interested in your views on cheese and sleep, and whether some types of cheese are worse for sleep than others. I don’t want to give up cheese entirely!❞
In principle, there’s nothing in cheese that, biochemically, should impair sleep. If anything, its tryptophan content could aid good sleep.
Tryptophan is found in many foods, including cheese, which (of common foods, anyway), for example cheddar cheese ranks second only to pumpkin seeds in tryptophan content.
Tryptophan can be converted by the body into 5-HTP, which you’ve maybe seen sold as a supplement. Its full name is 5-hydroxytryptophan.
5-HTP can, in turn, be used to make melatonin and/or serotonin. Which of those you will get more of, depends on what your body is being cued to do by ambient light/darkness, and other environmental cues.
If you are having cheese and then checking your phone, for instance, or otherwise hanging out where there are white/blue lights, then your body may dutifully convert the tryptophan into serotonin (calm wakefulness) instead of melatonin (drowsiness and sleep).
In short: the cheese will (in terms of this biochemical pathway, anyway) augment some sleep-inducing or wakefulness-inducing cues, depending on which are available.
You may be wondering: what about casein?
Casein is oft-touted as producing deep sleep, or disturbed sleep, or vivid dreams, or bad dreams. There’s no science to back any of this up, though the following research review is fascinating:
Dreams of the Rarebit Fiend: food and diet as instigators of bizarre and disturbing dreams
(it largely supports the null hypothesis of “not a causal factor” but does look at the many more likely alternative explanations, ranging from associated actually casual factors (such as alcohol and caffeine) and placebo/nocebo effect)
Finally, simple digestive issues may be the real thing at hand:
Worth noting that around two thirds of all people, including those who regularly enjoy dairy products, have some degree of lactose intolerance:
Lactose Intolerance in Adults: Biological Mechanism and Dietary Management
So, in terms of what cheese may be better/worse for you in this context, you might try experimenting with lactose-free cheese, which will help you identify whether that was the issue!
Share This Post
Related Posts
-
We analysed almost 1,000 social media posts about 5 popular medical tests. Most were utterly misleading
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Kim Kardashian posted on Instagram about having had a full-body MRI, she enthused that the test can be “life saving”, detecting diseases in the earliest stages before symptoms arise.
What Kardashian neglected to say was there’s no evidence this expensive scan can bring benefits for healthy people. She also didn’t mention it can carry harms including unnecessary diagnoses and inappropriate treatments.
With this post in mind, we wanted to explore what influencers are telling us about medical tests.
In a new study published today in JAMA Network Open, we analysed nearly 1,000 Instagram and TikTok posts about five popular medical tests which can all do more harm than good to healthy people, including the full-body MRI scan.
We found the overwhelming majority of these posts were utterly misleading.
C-R-V/Shutterstock 5 controversial tests
Before we get into the details of what we found, a bit about the five tests included in our study.
While these tests can be valuable to some, all five carry the risk of overdiagnosis for generally healthy people. Overdiagnosis is the diagnosis of a condition which would have never caused symptoms or problems. Overdiagnosis leads to overtreatment, which can cause unnecessary side effects and stress for the person, and wasted resources for the health system.
As an example, estimates suggest 29,000 cancers a year are overdiagnosed in Australia alone.
Overdiagnosis is a global problem, and it’s driven in part by healthy people having tests like these. Often, they’re promoted under the guise of early screening, as a way to “take control” of your health. But most healthy people simply don’t need them.
These are the five tests we looked at:
The full-body MRI scan claims to test for up to 500 conditions, including cancer. Yet there is no proven benefit of the scan for healthy people, and a real risk of unnecessary treatment from “false alarm” diagnoses.
The “egg timer” test (technically known as the AMH, or anti-mullarian hormone test) is often falsely promoted as a fertility test for healthy women. While it may be beneficial for women within a fertility clinic setting, it cannot reliably predict the chance of a woman conceiving, or menopause starting. However, low results can increase fear and anxiety, and lead to unnecessary and expensive fertility treatments.
Multi-cancer early detection blood tests are being heavily marketed as the “holy grail of cancer detection”, with claims they can screen for more than 50 cancers. In reality, clinical trials are still a long way from finished. There’s no good evidence yet that the benefits will outweigh the harms of unnecessary cancer diagnoses.
The gut microbiome test of your stool promises “wellness” via early detection of many conditions, from flatulence to depression, again without good evidence of benefit. There’s also concern that test results can lead to wasted resources.
Testosterone testing in healthy men is not supported by any high-quality evidence, with concerns direct-to-consumer advertising leads men to get tested and take testosterone replacement therapy unnecessarily. Use of testosterone replacement therapy carries its own risk of potential harms with the long-term safety in relation to heart disease and mortality still largely unknown.
Multi-cancer early detection blood tests are heavily marketed. Yuri A/Shutterstock What we found
Together with an international group of health researchers, we analysed 982 posts pertaining to the above tests from across Instagram and TikTok. The posts we looked at came from influencers and account holders with at least 1,000 followers, some with a few million followers. In total, the creators of the posts we included had close to 200 million followers.
Even discounting the bots, that’s a massive amount of influence (and likely doesn’t reflect their actual reach to non-followers too).
The vast majority of posts were misleading, failing to even mention the possibility of harm arising from taking one of these tests. We found:
- 87% of posts mentioned test benefits, while only 15% mentioned potential harms
- only 6% of posts mentioned the risk of overdiagnosis
- only 6% of posts discussed any scientific evidence, while 34% of posts used personal stories to promote the test
- 68% of influencers and account holders had financial interests in promoting the test (for example, a partnership, collaboration, sponsorship or selling for their own profit in some way).
Further analysis revealed medical doctors were slightly more balanced in their posts. They were more likely to mention the harms of the test, and less likely to have a strongly promotional tone.
The vast majority of posts we looked at were misleading. DimaBerlin/Shutterstock As all studies do, ours had some limitations. For example, we didn’t analyse comments connected to posts. These may give further insights into the information being provided about these tests, and how social media users perceive them.
Nonetheless, our findings add to the growing body of evidence showing misleading medical information is widespread on social media.
What can we do about it?
Experts have proposed a range of solutions including pre-bunking strategies, which means proactively educating the public about common misinformation techniques.
However, solutions like these often place responsibility on the individual. And with all the information on social media to navigate, that’s a big ask, even for people with adequate health literacy.
What’s urgently needed is stronger regulation to prevent misleading information being created and shared in the first place. This is especially important given social media platforms including Instagram are moving away from fact-checking.
In the meantime, remember that if information about medical tests promoted by influencers sounds too good to be true, it probably is.
Brooke Nickel, NHMRC Emerging Leader Research Fellow, University of Sydney; Joshua Zadro, NHMRC Emerging Leader Research Fellow, Sydney Musculoskeletal Health, University of Sydney, and Ray Moynihan, Assistant Professor, Faculty of Health Sciences & Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Celery vs Radish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to radish, we picked the celery.
Why?
It was very close! And yes, surprising, we know. Generally speaking, the more colorful/pigmented an edible plant is, the healthier it is. Celery is just one of those weird exceptions (as is cauliflower, by the way).
Macros-wise, these two are pretty much the same—95% water, with just enough other stuff to hold them together. The proportions of “other stuff” are also pretty much equal.
In the category of vitamins, celery has more vitamin K while radish has more vitamin C; the other vitamins are pretty close to equal. We’ll call this one a minor win for celery, as vitamin K is found in fewer foods than vitamin C.
When it comes to minerals, celery has more calcium, manganese, phosphorus, and potassium, while radish has more copper, iron, selenium, and zinc. We’ll call this a minor win for radish, as the margins are a little wider for its minerals.
So, that makes the score 1–1 so far.
Both plants have an assortment of polyphenols, of which, when we add up the averages, celery comes out on top by some way. Celery also comes out on top when we do a head-to-head of the top flavonoid of each; celery has 5.15mg/100g of apigenin to radish’s 0.63mg/100g kaempferol.
Which means, both are great healthy foods, but celery wins the day.
Want to learn more?
You might like to read:
Celery vs Cucumber – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
He Thinks His Wife Died in an Understaffed Hospital. Now He’s Trying to Change the Industry.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For the past year, police Detective Tim Lillard has spent most of his waking hours unofficially investigating his wife’s death.
The question has never been exactly how Ann Picha-Lillard died on Nov. 19, 2022: She succumbed to respiratory failure after an infection put too much strain on her weakened lungs. She was 65.
For Tim Lillard, the question has been why.
Lillard had been in the hospital with his wife every day for a month. Nurses in the intensive care unit had told him they were short-staffed, and were constantly rushing from one patient to the next.
Lillard tried to pitch in where he could: brushing Ann’s shoulder-length blonde hair or flagging down help when her tracheostomy tube gurgled — a sign of possible respiratory distress.
So the day he walked into the ICU and saw staff members huddled in Ann’s room, he knew it was serious. He called the couple’s adult children: “It’s Mom,” he told them. “Come now.”
All he could do then was sit on Ann’s bed and hold her hand, watching as staff members performed chest compressions, desperately trying to save her life.
A minute ticked by. Then another. Lillard’s not sure how long the CPR continued — long enough for the couple’s son to arrive and take a seat on the other side of Ann’s bed, holding her other hand.
Finally, the intensive care doctor called it and the team stopped CPR. Time of death: 12:37 p.m.
Lillard didn’t know what to do in a world without Ann. They had been married almost 25 years. “We were best friends,” he said.
Just days before her death, nurses had told Lillard that Ann could be discharged to a rehabilitation center as soon as the end of the week. Then, suddenly, she was gone. Lillard didn’t understand what had happened.
Lillard said he now believes that overwhelmed, understaffed nurses hadn’t been able to respond in time as Ann’s condition deteriorated. And he has made it his mission to fight for change, joining some nursing unions in a push for mandatory ratios that would limit the number of patients in a nurse’s care. “I without a doubt believe 100% Ann would still be here today if they had staffing levels, mandatory staffing levels, especially in ICU,” Lillard said.
Last year, Oregon became the second state after California to pass hospital-wide nurse ratios that limit the number of patients in a nurse’s care. Michigan, Maine, and Pennsylvania are now weighing similar legislation.
But supporters of mandatory ratios are going up against a powerful hospital industry spending millions of dollars to kill those efforts. And hospitals and health systems say any staffing ratio regulations, however well-intentioned, would only put patients in greater danger.
Putting Patients at Risk
By next year, the United States could have as many as 450,000 fewer nurses than it needs, according to one estimate. The hospital industry blames covid-19 burnout, an aging workforce, a large patient population, and an insufficient pipeline of new nurses entering the field.
But nursing unions say that’s not the full story. There are now 4.7 million registered nurses in the country, more than ever before.
The problem, the unions say, is a hospital industry that’s been intentionally understaffing their units for years in order to cut costs and bolster profits. The unions say there isn’t a shortage of nurses but a shortage of nurses willing to work in those conditions.
The nurse staffing crisis is now affecting patient care. The number of Michigan nurses who say they know of a patient who has died because of understaffing has nearly doubled in recent years, according to a Michigan Nurses Association survey last year.
Just months before Ann Picha-Lillard’s death, nurses and doctors at the health system where she died had asked the Michigan attorney general to investigate staffing cuts they believed were leading to dangerous conditions, including patient deaths, according to The Detroit News.
But Lillard didn’t know any of that when he drove his wife to the hospital in October 2022. She had been feeling short of breath for a few weeks after she and Lillard had mild covid infections. They were both vaccinated, but Ann was immunocompromised. She suffered from rheumatoid arthritis, a condition that had also caused scarring in her lungs.
To be safe, doctors at DMC Huron Valley-Sinai Hospital wanted to keep Ann for observation. After a few days in the facility, she developed pneumonia. Doctors told the couple that Ann needed to be intubated. Ann was terrified but Lillard begged her to listen to the doctors. Tearfully, she agreed.
With Ann on a ventilator in the ICU, it seemed clear to Lillard that nurses were understaffed and overwhelmed. One nurse told him they had been especially short-staffed lately, Lillard said.
“The alarms would go off for the medications, they’d come into the room, shut off the alarm when they get low, run to the medication room, come back, set them down, go to the next room, shut off alarms,” Lillard recalled. “And that was going on all the time.”
Lillard felt bad for the nurses, he said. “But obviously, also for my wife. That’s why I tried doing as much as I could when I was there. I would comb her hair, clean her, just keep an eye on things. But I had no idea what was really going on.”
Finally, Ann’s health seemed to be stabilizing. A nurse told Lillard they’d be able to discharge Ann, possibly by the end of that week.
By Nov. 17, Ann was no longer sedated and she cried when she saw Lillard and her daughter. Still unable to speak, she tried to mouth words to her husband “but we couldn’t understand what she was saying,” Lillard said.
The next day, Lillard went home feeling hopeful, counting down the days until Ann could leave the hospital.
Less than 24 hours later, Ann died.
Lillard couldn’t wrap his head around how things went downhill so fast. Ann’s underlying lung condition, the infection, and her weakened state could have proved fatal in the best of circumstances. But Lillard wanted to understand how Ann had gone from nearly discharged to dying, seemingly overnight.
He turned his dining room table into a makeshift office and started with what he knew. The day Ann died, he remembered her medical team telling him that her heart rate had spiked and she had developed another infection the night before. Lillard said he interviewed two DMC Huron Valley-Sinai nurse administrators, and had his own doctor look through Ann’s charts and test results from the hospital. “Everybody kept telling me: sepsis, sepsis, sepsis,” he said.
Sepsis is when an infection triggers an extreme reaction in the body that can cause rapid organ failure. It’s one of the leading causes of death in U.S. hospitals. Some experts say up to 80% of sepsis deaths are preventable, while others say the percentage is far lower.
Lives can be saved when sepsis is caught and treated fast, which requires careful attention to small changes in vital signs. One study found that for every additional patient a nurse had to care for, the mortality rate from sepsis increased by 12%.
Lillard became convinced that had there been more nurses working in the ICU, someone could have caught what was happening to Ann.
“They just didn’t have the time,” he said.
DMC Huron Valley-Sinai’s director of communications and media relations, Brian Taylor, declined a request for comment about the 2022 staffing complaint to the Michigan attorney general.
Following the Money
When Lillard asked the hospital for copies of Ann’s medical records, DMC Huron Valley-Sinai told him he’d have to request them from its parent company in Texas.
Like so many hospitals in recent years, the Lillards’ local health system had been absorbed by a series of other corporations. In 2011, the Detroit Medical Center health system was bought for $1.5 billion by Vanguard Health Systems, which was backed by the private equity company Blackstone Group.
Two years after that, in 2013, Vanguard itself was acquired by Tenet Healthcare, a for-profit company based in Dallas that, according to its website, operates 480 ambulatory surgery centers and surgical hospitals, 52 hospitals, and approximately 160 additional outpatient centers.
As health care executives face increasing pressure from investors, nursing unions say hospitals have been intentionally understaffing nurses to reduce labor costs and increase revenue. Also, insurance reimbursements incentivize keeping nurse staffing levels low. “Hospitals are not directly reimbursed for nursing services in the same way that a physician bills for their services,” said Karen Lasater, an associate professor of nursing in the Center for Health Outcomes and Policy Research at the University of Pennsylvania. “And because hospitals don’t perceive nursing as a service line, but rather a cost center, they think about nursing as: How can we reduce this to the lowest denominator possible?” she said.
Lasater is a proponent of mandatory nurse ratios. “The nursing shortage is not a pipeline problem, but a leaky bucket problem,” she said. “And the solutions to this crisis need to address the root cause of the issue, which is why nurses are saying they’re leaving employment. And it’s rooted in unsafe staffing. It’s not safe for the patients, but it’s also not safe for nurses.”
A Battle Between Hospitals and Unions
In November, almost one year after Ann’s death, Lillard told a room of lawmakers at the Michigan State Capitol that he believes the Safe Patient Care Act could save lives. The health policy committee in the Michigan House was holding a hearing on the proposed act, which would limit the amount of mandatory overtime a nurse can be forced to work, and require hospitals to make their staffing levels available to the public.
Most significantly, the bills would require hospitals to have mandatory, minimum nurse-to-patient ratios. For example: one nurse for every patient in the ICU; one for every three patients in the emergency room; a nurse for triage; and one nurse for every four postpartum birthing patients and well-baby care.
Efforts to pass mandatory ratio laws failed in Washington and Minnesota last year after facing opposition from the hospital industry. In Minnesota, the Minnesota Nurses Association accused the Mayo Clinic of using “blackmail tactics”: Mayo had told lawmakers it would pull billions of dollars in investment from the state if mandatory ratio legislation passed. Soon afterward, lawmakers removed nurse ratios from the legislation.
While Lillard waited for his turn to speak to Michigan lawmakers about the Safe Patient Care Act in November, members of the Michigan Nurses Association, which says it represents some 13,000 nurses, told lawmakers that its units were dangerously understaffed. They said critical care nurses were sometimes caring for up to 11 patients at a time.
“Last year I coded someone in an ICU for 10 minutes, all alone, because there was no one to help me,” said the nurses association president and registered nurse Jamie Brown, reading from another nurse’s letter.
“I have been left as the only specially trained nurse to take care of eight babies on the unit: eight fragile newborns,” said Carolyn Clemens, a registered nurse from the Grand Blanc area of Michigan.
Nikia Parker said she has left full-time emergency room nursing, a job she believes is her calling. After her friend died in the hospital where she worked, she was left wondering whether understaffing may have contributed to his death.
“If the Safe Patient Care Act passed, and we have ratios, I’m one of those nurses who would return to the bedside full time,” Parker told lawmakers. “And so many of my co-workers who have left would join me.”
But not all nurses agree that mandatory ratios are a good idea.
While the American Nurses Association supports enforceable ratios as an “essential approach,” that organization’s Michigan chapter does not, saying there may not be enough nurses in the state to satisfy the requirements of the Safe Patient Care Act.
For some lawmakers, the risk of collateral damage seems too high. State Rep. Graham Filler said he worries that mandating ratios could backfire.
“We’re going to severely hamper health care in the state of Michigan. I’m talking closed wards because you can’t meet the ratio in a bill. The inability for a hospital to treat an emergent patient. So it feels kind of to me like a gamble we’re taking,” said Filler, a Republican.
Michigan hospitals are already struggling to fill some 8,400 open positions, according to the Michigan Health & Hospital Association. That association says that complying with the Safe Patient Care Act would require hiring 13,000 nurses.
Every major health system in the state signed a letter opposing mandatory ratios, saying it would force them to close as many as 5,100 beds.
Lillard watched the debate play out in the hearing. “That’s a scare tactic, in my opinion, where the hospitals say we’re going to have to start closing stuff down,” he said.
He doesn’t think legislation on mandatory ratios — which are still awaiting a vote in the Michigan House’s health policy committee — are a “magic bullet” for such a complex, national problem. But he believes they could help.
“The only way these hospitals and the administrations are gonna make any changes, and even start moving towards making it better, is if they’re forced to,” Lillard said.
Seated in the center of the hearing room in Lansing, next to a framed photo of Ann, Lillard’s hands shook as he recounted those final minutes in the ICU.
“Please take action so that no other person or other family endures this loss,” he said. “You can make a difference in saving lives.”
Grief is one thing, Lillard said, but it’s another thing to be haunted by doubts, to worry that your loved one’s care was compromised before they ever walked through the hospital doors. What he wants most, he said, is to prevent any other family from having to wonder, “What if?”
This article is from a partnership that includes Michigan Public, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: