Cold Medicines & Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold Medicines & Heart Health
In the wake of many decongestants disappearing from a lot of shelves after a common active ingredient being declared useless*, you may find yourself considering alternative decongestants at this time of year.
*In case you missed it:
It doesn’t seem to be dangerous, by the way, just also not effective:
FDA Panel Says Common OTC Decongestant, Phenylephrine, Is Useless
Good for your nose, bad for your heart?
With products based on phenylephrine out of the running, products based on pseudoephedrine, a competing drug, are enjoying a surge in popularity.
Good news: pseudoephedrine works!
Bad news: pseudoephedrine works because it is a vasoconstrictor, and that vasoconstriction reduces nasal swelling. That same vasoconstriction also raises overall blood pressure, potentially dangerously, depending on an assortment of other conditions you might have.
Further reading: Can decongestants spike your blood pressure? What to know about hypertension and cold medicine
Who’s at risk?
The warning label, unread by many, reads:
❝Do not use this product if you have heart disease, high blood pressure, thyroid disease, diabetes, or difficulty in urination due to enlargement of the prostate gland, unless directed by a doctor❞
Source: Harvard Health | Don’t let decongestants squeeze your heart
What are the other options?
The same source as above recommends antihistamines as an option to be considered, citing:
❝Antihistamines such as […] cetirizine (Zyrtec) and loratadine (Claritin) can help with a stuffy nose and are safe for the heart.❞
But we’d be remiss not to mention drug-free options too, for example:
- Saline rinse with a neti pot or similar
- Use of a humidifier in your house/room
- Steam inhalation, with or without eucalyptus etc
See also: Inhaled Eucalyptus’s Immunomodulatory and Antimicrobial Effects
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chair Stretch Workout Guide
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝The 3 most important exercises don’t work if you can’t get on the floor. I’m 78, and have knee replacements. What about 3 best chair yoga stretches? Love your articles!❞
Here are six!
Share This Post
-
Dietary Changes for Artery Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝How does your diet change clean out your arteries of the bad cholesterol?❞
There’s good news and bad news here, and they can both be delivered with a one-word reply:
Slowly.
Or rather: what’s being cleaned out is mostly not the LDL (bad) cholesterol, but rather, the result of that.
When our diet is bad for cardiovascular health, our arteries get fatty deposits on their walls. Cholesterol gets stuck here too, but that’s not the main physical problem.
Our body’s natural defenses come into action and try to clean it up, but they (for example macrophages, a kind of white blood cell that consumes invaders and then dies, before being recycled by the next part of the system) often get stuck and become part of the buildup (called atheroma), which can lead to atherosclerosis and (if calcium levels are high) hardening of the arteries, which is the worst end of this.
This can then require medical attention, precisely because the body can’t remove it very well—especially if you are still maintaining a heart-unhealthy diet, thus continuing to add to the mess.
However, if it is not too bad yet, yes, a dietary change alone will reverse this process. Without new material being added to the arterial walls, the body’s continual process of rejuvenation will eventually fix it, given time (free from things making it worse) and resources.
In fact, your arteries can be one of the quickest places for your body to make something better or worse, because the blood is the means by which the body moves most things (good or bad) around the body.
All the more reason to take extra care of it, since everything else depends on it!
You might also like our previous main feature:
Share This Post
-
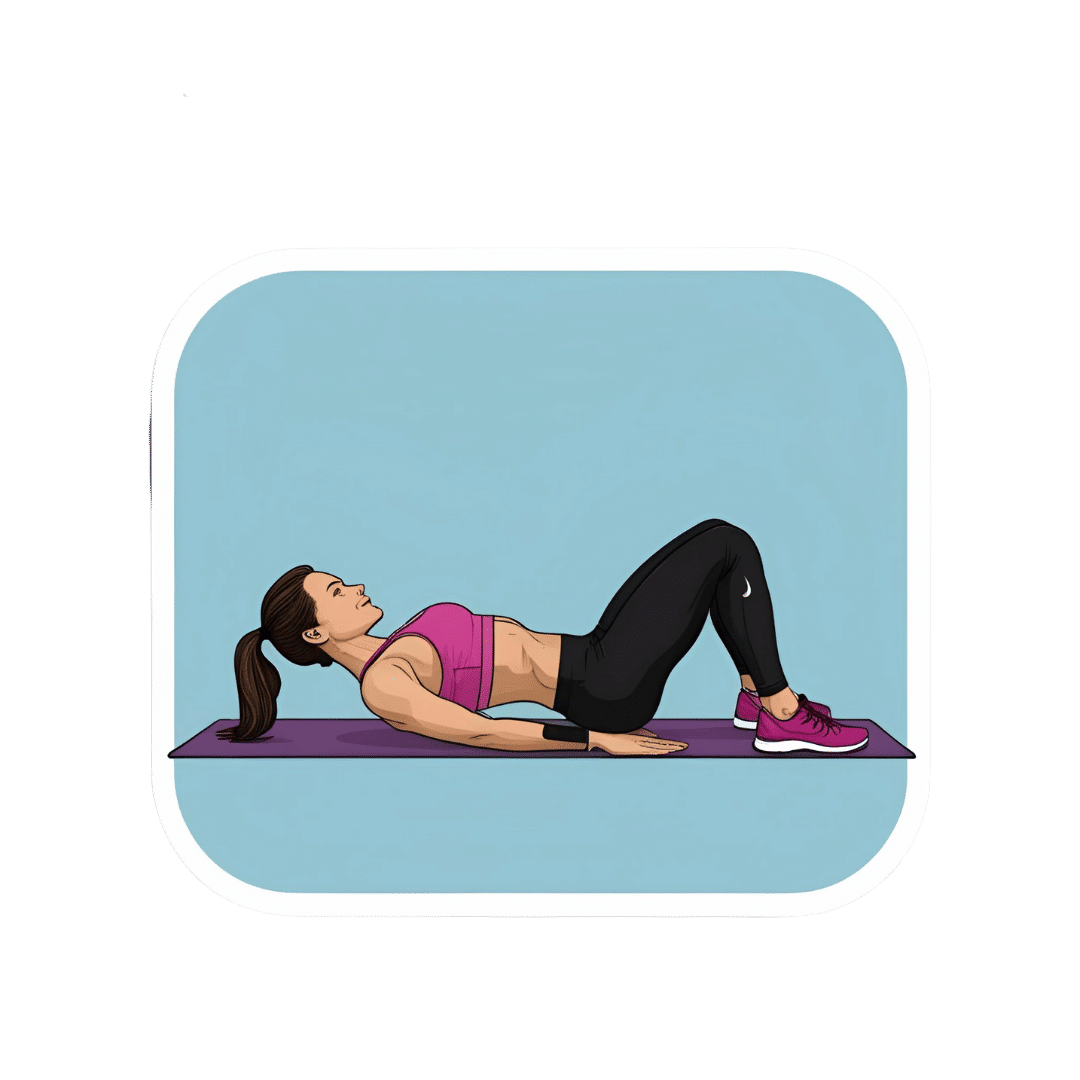
What Happens To Your Body When You Do 100 Glute Bridges Every Day
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not just for a sculpted butt:
Benefits
With consistent daily glute bridge practice, you may expect:
- Rounder, toned butt: targets the gluteus maximus, toning and lifting the butt for a rounder appearance.
- Improved posture: strengthens glutes to support the spine and pelvis, alleviating lower back and hip pain. Stretches tight hip flexors from prolonged sitting.
- Stronger lower back: glutes support the lower back and spine, reducing pain and making it easier to lift heavy objects. Activating the glutes transfers force from legs to core, preventing injuries.
- Stronger knees: stabilizes the knee joint and promotes alignment by engaging glutes, hamstrings, and quadriceps, reducing knee pain.
- Sculpted hamstrings: contracts hamstrings during lifts for strength, while stretching them on the way down increases flexibility.
- Increased hip flexibility: strengthens muscles around the hip joint, improving mobility and counteracting tight hips from sedentary habits.
- Reduced back pain: strengthens glutes to correct pelvic tilt and reduce strain on the lower back.
- Faster running speed: improves hip extension, strengthens hamstrings, and activates the gluteus medius for better running power and balance.
- Enhanced strength training performance: strengthens glutes, back, and knees, improving performance in exercises like squats and deadlifts.
As for how to get going, the video offers the following very sound advice: begin with 25–30 reps per session and gradually increase to sets of 100 daily. It should take about 5 minutes (that’s 3 seconds per repetition). Results can be seen in as little as 2 weeks, with significant changes after a month of consistent practice.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Strong Curves: A Woman’s Guide to Building a Better Butt and Body – by Bret Contreras & Kellie Davis
Take care!
Share This Post
Related Posts
-
28-Day FAST Start Day-by-Day – by Gin Stephens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have previously reviewed Gin Stephens’ other book, “Fast. Feast. Repeat.”, so what’s so special about this one that it deserves reviewing too?
This one is all about troubleshooting the pitfalls that many people find when taking up intermittent fasting.
To be clear: the goal here is not a “28 days and yay you did it, put that behind you now”, but rather “28 days and you are now intermittently fasting easily each day and can keep it up without difficulty”. As for the difficulties that may arise early in the 28 days…
Not just issues of willpower, but also the accidental breaks. For example, some artificial sweeteners, while zero-calorie, trigger an insulin response, which breaks the fast on the metabolic level (avoiding that is the whole point of IF). Lots of little tips like that peppered through the book help the reader to stop accidentally self-sabotaging their progress.
The author does talk about psychological issues too, and also how it will feel different at first while the liver is adapting, than later when it has already depleted its glycogen reserves and the body must burn body fat instead. Information like that makes it easier to understand that some initial problems (hunger, getting “hangry”, feeling twitchy, or feeling light-headed) will last only a few weeks and then disappear.
So, understanding things like that makes a big difference too.
The style of the book is simple and clear pop-science, with lots of charts and bullet points and callout-boxes and the like; it makes for very easy reading, and very quick learning of all the salient points, of which there are many.
Bottom line: if you’ve tried intermittent fasting but struggled to make it stick, this book can help you get to where you want to be.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
3 Things Everyone Over 50 Must Do Daily for Healthy Feet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Will Harlow, the over-50s specialist physio, wants you to be on a good footing:
Daily steps in the right direction
The three daily exercises recommended in the video are:
Exercise 1: Towel Scrunch
The towel scrunch exercise strengthens the flexor muscles in the feet, improving balance and improving contact with the ground. To do this exercise, sit on a chair with a towel placed on the floor beneath your toes while keeping your heels on the ground. Use only your toes to pull the towel toward your heel, scrunching it up as much as possible. This movement strengthens the arch of the foot and can help alleviate symptoms of flat feet. For best results, practice this exercise for 2–3 minutes once or twice daily. Once you’ve got the hand of doing it sitting, do it while standing.
Exercise 2: Big Toe Extension
Big toe extension is an essential exercise for maintaining foot mobility and improving walking kinesthetics by preventing stiffness in the big toe. To do this exercise, keep your foot flat on the floor and try to lift only your big toe while keeping the four other toes firmly pressed down. To be clear, we mean under its own power; not using your hands to help. Many people find this difficult initially, but it’s due to a loss of neural connection rather than muscle strength, so with practice, the ability to isolate the movement improves quite quickly. Perform 10 repetitions in a row, three times per day, for optimal benefits. Once you’ve got the hand of doing it sitting, do it while standing.
Exercise 3: Calf Stretch
The calf stretch is an important exercise for maintaining foot health by preventing tight calves, which can contribute to issues like plantar fasciitis and Morton’s neuroma. To do this stretch, place your hands against a wall for support and extend one leg straight behind you while keeping your other heel firmly on the floor. The front knee should be bent while the back leg remains straight, creating a stretch in the calf. Hold this position for 30 seconds (building up to that, if necessary). Since the effectiveness of stretching comes from frequency rather than duration, this stretch should be performed three to four times per day for the best results.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Steps For Keeping Your Feet A Healthy Foundation ← this one’s about general habits, not exercises
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Signs Of Low Estrogen In Women: What Your Skin, Hair, & Nails Are Trying To Tell You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Skin, hair, and nails are often thought of purely as a beauty thing, but in fact they can be indicative of a lot of other aspects of health. Dr. Andrea Suarez takes us through some of them in this video about the systemic (i.e., whole-body, not just related to sex things) effects of estrogen, and/or a deficiency thereof.
Beyond the cosmetic
Low estrogen levels are usual in women during and after untreated menopause, resulting in various changes in the skin, hair, and nails, that reflect deeper issues, down to bone health, heart health, brain health, and more. Since we can’t see our bones or hearts or brains without scans (or a serious accident/incident), we’re going to focus on the outward signs of estrogen deficiency.
Estrogen helps maintain healthy collagen production, skin elasticity, wound healing, and moisture retention, making it essential for youthful and resilient skin. Declining estrogen levels with menopause lead to a thinner epidermis, decreased collagen production, and more pronounced wrinkles. Skin elasticity also diminishes, which slows the skin’s ability to recover from stretching or deformation. Wound healing also becomes slower, increasing the risk of infections and extended recovery periods after injuries or surgeries—bearing in mind that collagen is needed in everything from our skin to our internal connective tissue (fascia) and joints and bones. So all those things are going to struggle to recover from injury (and surgery is also an injury) without it.
Other visible changes associated with declining estrogen include significant dryness as a result of reduced hyaluronic acid and glycosaminoglycan production, which are essential for moisture retention. The skin becomes more prone to irritation and increased water loss. Additionally, estrogen deficiency results in less resistance to oxidative stress, making the skin more susceptible to damage from environmental factors such as UV radiation and pollution, as well as any from-the-inside pollution that some may have depending on diet and lifestyle.
Acne and enlarged pores are associated with increased testosterone, but testosterone and estrogen are antagonistic in most ways, and in this case a decrease in estrogen will do the same, due increased unopposed androgen signaling affecting the oil glands. The loss of supportive collagen also causes the skin around pores to lose structure, making them appear larger. The reduction in skin hydration further exacerbates the visibility of pores and can contribute to the development of blackheads due to abnormal cell turnover.
Blood vessel issues tend to arise as estrogen levels drop, leading to a reduction in angiogenesis, i.e. the formation and integrity of blood vessels. This results in more fragile and leaky blood vessels, making the skin more prone to bruising, especially on areas frequently exposed to the sun, such as the backs of the hands. This weakened vasculature also further contributes to the slower wound healing that we talked about, due to less efficient delivery of growth factors.
Hair and nail changes often accompany estrogen deficiency. Women may notice hair thinning, increased breakage, and a greater likelihood of androgenic alopecia. The texture of the hair can change, becoming more brittle. Similarly, nails can develop ridges, split more easily, and become more fragile due to reduced collagen and keratin production, which also affects the skin around the nails.
As for what to do about it? Management options for estrogen-deficient skin include:
- Bioidentical hormone replacement therapy (HRT), which can improve skin elasticity, boost collagen production, and reduce dryness and fragility, as well as addressing the many more serious internal things that are caused by the same deficiency as these outward signs.
- Low-dose topical estrogen cream, which can help alleviate skin dryness and increase skin strength, won’t give the systemic benefits (incl. to bones, heart, brain, etc) that only systemic HRT can yield.
- Plant-based phytoestrogens, which are not well-evidenced, but may be better than nothing if nothing is your only other option. However, if you are taking anything other form of estrogen, don’t use phytoestrogens as well, or they will compete for estrogen receptors, and do the job not nearly so well while impeding the bioidentical estrogen from doing its much better job.
And for all at any age, sunscreen continues to be one of the best things to put on one’s skin for general skin health, and this is even more true if running low on estrogen.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
These Signs Often Mean These Nutrient Deficiencies (Do You Have Any?)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: