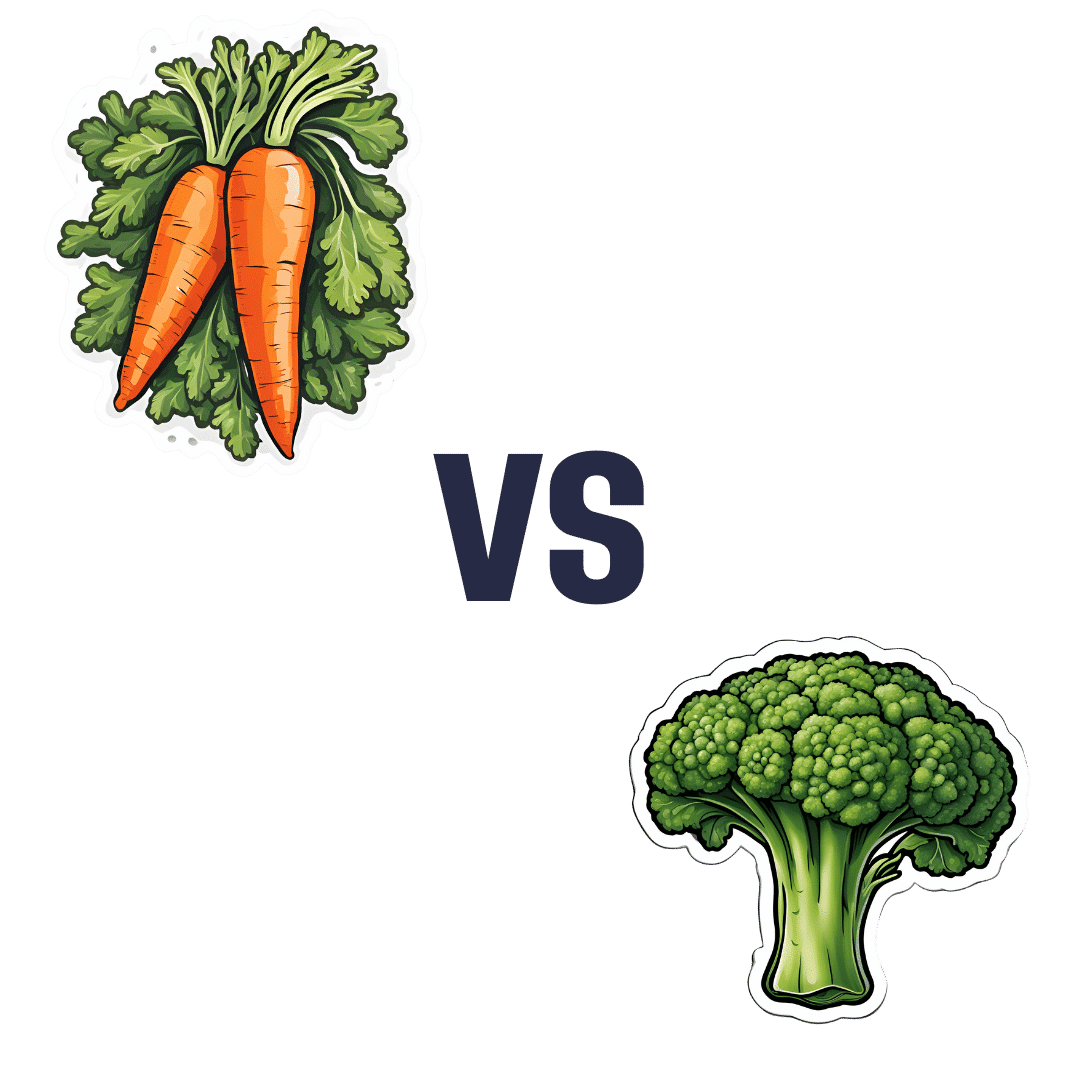
Carrots vs Broccoli – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing carrots to broccoli, we picked the broccoli.
Why?
These are both excellent candidates that should be in everyone’s diet, but there’s a clear winner:
In terms of macros, carrots have 50% more carbs for the same fiber (giving carrots the relatively higher glycemic index, though really, nobody is getting metabolic disease from eating carrots, which are a low-GI food already), while broccoli has more protein. By the numbers, it’s a nominal win for broccoli here, but really, both are great.
In the category of vitamins, carrots have more of vitamins A and B3, while broccoli has more of vitamins B1, B2, B5, B6, B7, B9, C, E, K, and choline. An easy win for broccoli. We’d like to emphasize, though, that this doesn’t mean carrots don’t have lots of vitamins—they do—it’s just that broccoli has even more!
When it comes to minerals, carrots are genuinely great, and/but not higher in any minerals than broccoli, while broccoli has more calcium, copper, iron, magnesium, manganese, phosphorus, selenium, and zinc. So again, a clear win for broccoli, despite carrots’ fortitude.
All in all, an overwhelming win for broccoli, though once again, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Nori vs Wakame – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing nori to wakame, we picked the nori.
Why?
It was close, and both of these seaweed options are great!
In terms of macros, nori has more protein while wakame has more carbs; they’re about equal on fiber. While the difference in protein and carbs isn’t big, out of the two we’ll prioritize protein, and thus say nori gets a notional win here—but as it’s so close, one could just as easily call it a tie.
In the category of vitamins both are very rich in many minerals, but nori has more of vitamins A, B1, B2, B6, B12*, and C, while wakame has more of vitamins B5, B9, K, and choline. Thus, a 6:4 victory for nori.
*Yes, nori is one of those rare vegan foods that naturally contain vitamin B12; it’s because of the composition of the algae that this seaweed is made of, which includes some beneficial B12-making bacteria. Meanwhile, wakame is “just” a kelp, so it doesn’t have B12.
When it comes to minerals, nori has more potassium and zinc, while wakame has more calcium and magnesium. They’re equal on other minerals, except: it’s worth noting that wakame is moderately high in sodium, while nori has very little sodium. So, either a tie-breaking win for nori, or just a tie.
Adding up the sections gives nori the overall win; it’s only the margin of the win that’s reasonably debatable. Still, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
- A Deeper Dive Into Seaweed
- Spirulina vs Nori – Which is Healthier? ← guess which won!
- 21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!) ← nori and wakame both feature (very favorably) in this case study
Enjoy!
Share This Post
-
Astrology, Mental health and the Economics of Well Being
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ultimately can the mental health system single-handedly address the concerns of inequality and economic access in society?
Around 75 per cent of the Indian population lives in rural areas, but their access to quality mental health care is limited and traditional approaches continue to be in use. The shortage is to such a large extent that there are only 0.7 physicians per 1000 population and only one psychiatrist for every 343,000 Indians. While over the years the mental health sector has seen major developments, like the 2017 mental health care act. This act establishes equal access for all citizens, to avail government-run or funded mental health services in the country. However, it does not bridge the gap in society as the majority of the population remains deeply unaware or unable to access these services.
While the uncertainties of the pandemic brought mental wellbeing to the forefront, the national budget for the sector dropped, making this an issue of human rights. This accessibility to services is further corroborated by the recurring financial expenses of medications and frequent visits to government clinics. The cost of sessions is steep and a single session is not ideal. Spending exorbitant amounts on healthcare is a burden most families can’t afford leading to debt. In the absence of insurance and healthcare schemes and provisions, therapy remains a luxury to many Indians.
Economic struggles are only one of the causes of this discerning gap in the mental health sector. Barriers caused by sexuality, gender, caste and religion also play a major role in mediating people’s perception and access to therapeutic services. The persistent stigma surrounding mental health, especially in India continues to be a hindrance to seeking help. The supernatural inhibitions and disparity in knowledge across communities only create more confusion. The notion that mental well being is an optional expense is popular, even though the country’s population is in a dire state. Data collected in a WHO report found that nearly 15 per cent of Indian adults need active intervention for one or more mental health issues.
The population disregards the very prevalence of such mental disorders and more than often finds it fruitless to receive treatment. Some who are open-minded fail to afford the hiked fees that therapists in urban settings charge, leaving them with no option. While for years Indians attributed the systemic weakness of the mental health system to the people’s attitudes, a 2016 survey showed more than 42% of people have positive attitudes toward mental wellbeing and treatment. While the skeptics remain, these underprivileged sections of society too struggle to gain the accessibility they deserve.
This is where astrology, tarot card reading and other spiritual practices, have created a market for themselves in the well-being industry. The sceptics, and those from poor socio-economic backgrounds resort to these local and easily accessible ways of coping, to instil the faith they so desperately need. Astrology is a layman’s substitute for therapy, or for some even a supplement when they cannot afford extended periods of treatment. Visiting a local astrologer in many ways breeds the self-awareness one would expect from a session in therapy. These practices even hold certain similarities to actual psychotherapy settings, in the way they define, and alleviate aspects of one’s personality and behaviour.
Very often one simply needs an explanation, or an answer to the ‘why’ no matter how scientifically rooted that response truly is. Astrologers impart a level of faith, that things will get better. For those in rural areas, struggling to provide the bare necessities to their family affording therapy is impossible, so their local psychic, astrologer or pandit becomes their anchor during emotional duress. Tarot cards and other practices primarily focus on the future and act as a guide point for how to deal with the things ahead. For a farmer coping with anxiety, access to anti-anxiety medication is strained, and so is therapy. His best bet remains to consult his next-door jyotish about his burdens.
A famous clinician Caroline Hexdall in an interview said that “ Part of the popularity of astrology and tarot today has to do with their universal nature”. With growing technology and the pervasiveness of social media, people can gain easy access to self-care and astrology resources. Apps and web pages provide daily tarot cards, zodiac signs readings and astrological predictions for people, and almost serve the purpose of a therapist. Is reading the lines on our palm, and checking the alignment of the stars enough to cure the mental illness they undergo? Is it a solution or a quick fix as a consequence of an ignorant healthcare system?
Several studies have also shown the deteriorating effects of depending on astrology. Cases of worsening and onset of depression, anxiety and personality disorders are common for those who use astrology as more than just a temporary coping mechanism. It also becomes a source of losing control, as every feeling is attributed to fate and destiny, instilling a sense of helplessness. Ultimately can the mental health system single-handedly address the concerns of inequality and economic access in society?
Maahira Jain is a third-year student at Ashoka University studying Psychology and Media studies. She is a movie buff and is extremely passionate about writing and traveling.
This article is republished from OpenAxis under a Creative Commons license. Read the original article.
Share This Post
-
The Brain-Skin Doctor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Of Brains And Breakouts
Today’s spotlight is on Dr. Claudia Aguirre. She’s a molecular neuroscientist, and today she’s going to be educating us about skin.
What? Why?
When we say “neuroscience”, we generally think of the brain. And indeed, that’s a very important part of it.
We might think about eyes, which are basically an extension of the brain.
We don’t usually think about skin, which (just like our eyes) is constantly feeding us a lot of information about our surroundings, via a little under three million nerve endings. Guess where the other ends of those nerves lead!
There’s a constant two-way communication going on between our brain and our skin.
What does she want us to know?
Psychodermatology
The brain and the skin talk to each other, and maladies of one can impact the other:
- Directly, e.g. stress prompting skin breakouts (actually this is a several-step process physiologically, but for the sake of brevity we’ll call this direct)
- Indirectly, e.g. nervous disorders that result in people scratching or picking at their skin, which prompts a whole vicious cycle of one thing making the other worse
Read more: Psychodermatology: The Brain-Skin Connection
To address both kinds of problems, clearly something beyond moisturizer is needed!
Mindfulness (meditation and beyond)
Mindfulness is a well-evidenced healthful practice for many reasons, and Dr. Aguirra argues the case for it being good for our skin too.
As she points out,
❝Cultural stress and anxiety can trigger or aggravate many skin conditions—from acne to eczema to herpes, psoriasis, and rosacea.
Conversely, a disfiguring skin condition can trigger stress, anxiety, depression, and even suicide.
Chronic, generalized anxiety can create chronic inflammation and exacerbate inflammatory skin conditions, such as those I mentioned previously.
Chronic stress can result in chronic anxiety, hypervigilance, poor sleep, and a whole cascade of effects resulting in a constant breakdown of tissues and organs, including the skin.❞
So, she recommends mindfulness-based stress reduction (MBSR), for the above reasons, along with others!
Read more: Mind Matters
How to do it: No-Frills, Evidence-Based Mindfulness
And as for “and beyond?”
Do you remember in the beginning of the pandemic, when people were briefly much more consciously trying to avoid touching their faces so much? That, too, is mindfulness. It may have been a stressed and anxious mindfulness for many*, but mindfulness nonetheless.
*which is why “mindfulness-based stress reduction” is not a redundant tautology repeated more than once unnecessarily, one time after another 😉
So: do try to keep aware of what you are doing to your skin, and so far as is reasonably practicable, only do the things that are good for it!
The skin as an endocrine organ
Nerves are not the only messengers in the body; hormones do a lot of our body’s internal communication too. And not just the ones everyone remembers are hormones (e.g. estrogen, testosterone, although yes, they do both have a big impact on skin too), but also many more, including some made in the skin itself!
Dr. Aguirra gives us a rundown of common conditions, the hormones behind them, and what we can do if we don’t want them:
Read more: Rethinking The Skin As An Endocrine Organ
Take-away advice:
For healthy skin, we need to do more than just hydrate, get good sleep, have good nutrition, and get a little sun (but not too much).
- We should also practice mindfulness-based stress reduction, and seek help for more serious mental health issues.
- We should also remember the part our hormones play in our skin, and not just the obvious ones.
Did you know that vitamin D is also a hormone, by the way? It’s not the only hormone at play in your skin by a long way, but it is an important one:
Society for Endocrinology | Vitamin D
Want to know more?
You might like this interview with Dr. Aguirre:
The Brain in Our Skin: An Interview with Dr. Claudia Aguirre
Take care!
Share This Post
Related Posts
-
Hope: A research-based explainer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This year, more than 60 countries, representing more than 4 billion people, will hold major elections. News headlines already are reporting that voters are hanging on to hope. When things get tough or don’t go our way, we’re told to hang on to hope. HOPE was the only word printed on President Barack Obama’s iconic campaign poster in 2008.
Research on hope has flourished only in recent decades. There’s now a growing recognition that hope has a role in physical, social, and mental health outcomes, including promoting resilience. As we embark on a challenging year of news, it’s important for journalists to learn about hope.
So what is hope? And what does the research say about it?
Merriam-Webster defines hope as a “desire accompanied by expectation of or belief in fulfillment.” This definition highlights the two basic dimensions of hope: a desire and a belief in the possibility of attaining that desire.
Hope is not Pollyannaish optimism, writes psychologist Everett Worthington in a 2020 article for The Conversation. “Instead, hope is a motivation to persevere toward a goal or end state, even if we’re skeptical that a positive outcome is likely.”
There are several scientific theories about hope.
One of the first, and most well-known, theories on hope was introduced in 1991 by American psychologist Charles R. Snyder.
In a paper published in the Journal of Personality and Social Psychology, Snyder defined hope as a cognitive trait centered on the pursuit of goals and built on two components: a sense of agency in achieving a goal, and a perceived ability to create pathways to achieve that goal. He defined hope as something individualistic.
Snyder also introduced the Hope Scale, which continues to be used today, as a way to measure hope. He suggested that some people have higher levels of hope than others and there seem to be benefits to being more hopeful.
“For example, we would expect that higher as compared with lower hope people are more likely to have a healthy lifestyle, to avoid life crises, and to cope better with stressors when they are encountered,” they write.
Others have suggested broader definitions.
In 1992, Kaye Herth, a professor of nursing and a scholar on hope, defined hope as “a multidimensional dynamic life force characterized by a confident yet uncertain expectation of achieving good, which to the hoping person, is realistically possible and personally significant.” Herth also developed the Herth Hope Index, which is used in various settings, including clinical practice and research.
More recently, others have offered an even broader definition of hope.
Anthony Scioli, a clinical psychologist and author of several books on hope, defines hope “as an emotion with spiritual dimensions,” in a 2023 review published in Current Opinion in Psychology. “Hope is best viewed as an ameliorating emotion, designed to fill the liminal space between need and reality.”
Hope is also nuanced.
“Our hopes may be active or passive, patient or critical, private or collective, grounded in the evidence or resolute in spite of it, socially conservative or socially transformative,” writes Darren Webb in a 2007 study published in History of the Human Sciences. “We all hope, but we experience this most human of all mental feelings in a variety of modes.”
To be sure, a few studies have shown that hope can have negative outcomes in certain populations and situations. For example, one study highlighted in the research roundup below finds that Black college students who had higher levels of hope experienced more stress due to racial discrimination compared with Black students who had lower levels of hope.
Today, hope is one of the most well-studied constructs within the field of positive psychology, according to the journal Current Opinion in Psychology, which dedicated its August 2023 issue to the subject. (Positive psychology is a branch of psychology focused on characters and behaviors that allow people to flourish.)
We’ve gathered several studies below to help you think more deeply about hope and recognize its role in your everyday lives.
Research roundup
The Role of Hope in Subsequent Health and Well-Being For Older Adults: An Outcome-Wide Longitudinal Approach
Katelyn N.G. Long, et al. Global Epidemiology, November 2020.The study: To explore the potential public health implications of hope, researchers examine the relationship between hope and physical, behavioral and psychosocial outcomes in 12,998 older adults in the U.S. with a mean age of 66.
Researchers note that most investigations on hope have focused on psychological and social well-being outcomes and less attention has been paid to its impact on physical and behavioral health, particularly among older adults.
The findings: Results show a positive association between an increased sense of hope and a variety of behavioral and psychosocial outcomes, such as fewer sleep problems, more physical activity, optimism and satisfaction with life. However, there wasn’t a clear association between hope and all physical health outcomes. For instance, hope was associated with a reduced number of chronic conditions, but not with stroke, diabetes and hypertension.
The takeaway: “The later stages of life are often defined by loss: the loss of health, loved ones, social support networks, independence, and (eventually) loss of life itself,” the authors write. “Our results suggest that standard public health promotion activities, which often focus solely on physical health, might be expanded to include a wider range of factors that may lead to gains in hope. For example, alongside community-based health and nutrition programs aimed at reducing chronic conditions like hypertension, programs that help strengthen marital relations (e.g., closeness with a spouse), provide opportunities to volunteer, help lower anxiety, or increase connection with friends may potentially increase levels of hope, which in turn, may improve levels of health and well-being in a variety of domains.”
Associated Factors of Hope in Cancer Patients During Treatment: A Systematic Literature Review
Corine Nierop-van Baalen, Maria Grypdonck, Ann van Hecke and Sofie Verhaeghe. Journal of Advanced Nursing, March 2020.The study: The authors review 33 studies, written in English or Dutch and published in the past decade, on the relationship between hope and the quality of life and well-being of patients with cancer. Studies have shown that many cancer patients respond to their diagnosis by nurturing hope, while many health professionals feel uneasy when patients’ hopes go far beyond their prognosis, the authors write.
The findings: Quality of life, social support and spiritual well-being were positively associated with hope, as measured with various scales. Whereas symptoms, psychological distress and depression had a negative association with hope. Hope didn’t seem to be affected by the type or stage of cancer or the patient’s demographics.
The takeaway: “Hope seems to be a process that is determined by a person’s inner being rather than influenced from the outside,” the authors write. “These factors are typically given meaning by the patients themselves. Social support, for example, is not about how many patients experience support, but that this support has real meaning for them.”
Characterizing Hope: An Interdisciplinary Overview of the Characteristics of Hope
Emma Pleeging, Job van Exel and Martijn Burger. Applied Research in Quality of Life, September 2021.The study: This systematic review provides an overview of the concept of hope based on 66 academic papers in ten academic fields, including economics and business studies, environmental studies, health studies, history, humanities, philosophy, political science, psychology, social science, theology and youth studies, resulting in seven themes and 41 sub-themes.
The findings: The authors boil down their findings to seven components: internal and external sources, the individual and social experience of hope, internal and external effects, and the object of hope, which can be “just about anything we can imagine,” the authors write.
The takeaway: “An important implication of these results lies in the way hope is measured in applied and scientific research,” researchers write. “When measuring hope or developing instruments to measure it, researchers could be well-advised to take note of the broader understanding of the topic, to prevent that important characteristics might be overlooked.”
Revisiting the Paradox of Hope: The Role of Discrimination Among First-Year Black College Students
Ryon C. McDermott, et al. Journal of Counseling Psychology, March 2020.The study: Researchers examine the moderating effects of hope on the association between experiencing racial discrimination, stress and academic well-being among 203 first-year U.S. Black college students. They build on a small body of evidence that suggests high levels of hope might have a negative effect on Black college students who experience racial discrimination.
The authors use data gathered as part of an annual paper-and-pencil survey of first-year college students at a university on the Gulf Coast, which the study doesn’t identify.
The findings: Researchers find that Black students who had higher levels of hope experienced more stress due to racial discrimination compared with students who had lower levels of hope. On the other hand, Black students with low levels of hope may be less likely to experience stress when they encounter discrimination.
Meanwhile, Black students who had high levels of hope were more successful in academic integration — which researchers define as satisfaction with and integration into the academic aspects of college life — despite facing discrimination. But low levels of hope had a negative impact on students’ academic well-being.
“The present study found evidence that a core construct in positive psychology, hope, may not always protect Black students from experiencing the psychological sting of discrimination, but it was still beneficial to their academic well-being,” the authors write.
The takeaway: “Our findings also highlight an urgent need to reduce discrimination on college campuses,” the researchers write. “Reducing discrimination could help Black students (and other racial minorities) avoid additional stress, as well as help them realize the full psychological and academic benefits of having high levels of hope.”
Additional reading
Hope Across Cultural Groups Lisa M. Edwards and Kat McConnell. Current Opinion in Psychology, February 2023.
The Psychology of Hope: A Diagnostic and Prescriptive Account Anthony Scioli. “Historical and Multidisciplinary Perspectives on Hope,” July 2020.
Hope Theory: Rainbows in the Mind C.R. Snyder. Psychological Inquiry, 2002
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Curing Hiccups And Headaches At Home With Actual Science
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Quick fixes for bodily annoyances
Do you ever find yourself desperately trying to cure hiccups, and advice on the Internet is like “breathe in through your ears while drinking vinegar upside-down through your nose”?
If so, you’re not alone. So, today we’re going to look at some science-based approaches to dealing with common bodily annoyances.
Hiccups
Unfortunately, most popular advices simply don’t work, and the only near-guaranteed way to cure these is with anti-convulsive medications whose side-effects may be worse than the hiccups.
However, before you head to the pharmacy, there is one breathing exercise that has a very simple scientific underpinning: 4:4 breathing. If you’re unfamiliar, it’s just:
- Breathe slowly in through your nose to a count of four
- Hold your breath for a count of four
- Breathe slowly out through your nose to a count of four
- Hold your breath for a count of four
…and repeat. The slower the better. At first, your hiccups will interrupt this, but just “keep calm and carry on”.
The reason this can work is that breathing is an autonomic function (e.g., it happens without us thinking about it) that, unlike most other autonomic functions, we can all control directly. By taking control of one, others will tend to fall into line with it.
For example, it is normal that your heart rate will tend to slow or quicken as your breathing slows or quickens, respectively.
Your hiccups? Autonomic function. Actually a very, very old evolutionary left-over trait, that’s only useful for protecting lungs while breathing underwater. In other words, it’s the bodily function thinks you’re a fish (or a tadpole-like amphibious creature) in the process of developing lungs. Unfortunately, because hiccuping doesn’t harm our chances of passing on our genes, it never got naturally de-selected so we still have it.
Anyway, the bottom line is: take control of your breathing in the aspects you can directly control, and the aspects you can’t directly control will fall into line. You may need to give it some minutes, don’t give up too quickly.
Headaches
If you ever get a headache and you don’t have painkillers or perhaps they’re not helping or you have another reason for not wanting to take them, there’s “one quick trick” that can cure most headaches in seconds.
First, the limitation: this will only cure headaches that have been caused by increased localized blood pressure in the forehead. However, that’s more than half of most common headaches.
Next, how it works…
We’re mentioning this first, because understanding how it works will give you more confidence in using it.
Your body has a wonderful homeostatic system, which is the system by which your body maintains its “Goldilocks zones” of not too hot or cold, not to acidine or alkaline, not too hydrated or dehydrated, blood pressure not too high or too low, etc. Sometimes, however, it can get confused, and needs a nudge back to where it should be.
One of the ways it maintains blood pressure is biofeedback from receptors in blood vessel walls, called baroreceptors. They are what it sounds like; they measure blood pressure internally.
In certain places, there are clusters of baroreceptors in one place. And if we press on that one place, the body will think “Oh no! Super high blood pressure in this bit!” and reduce the blood pressure immediately.
This is called the baroreflex, and that’s what you need to cure a hypertensive headache.
So, what to do:
With your thumb, carefully feel the upper inside corner of your eye socket. So, at the top, and about ¼ of the way out from the bridge of your nose. You should feel a groove. No, not like the Emperor’s New, but, an actual groove in your eye socket. That’s the supraorbital notch (or foramen), and it allows the supraorbital artery, veins, and nerve to run through.
Press it firmly (you can do both sides at once, assuming you have two thumbs) for about three seconds, and then massage it gently. Repeat as necessary, but it shouldn’t take more than about three goes to have cured the headache.
As a bonus, this is a great party trick for curing other people’s headaches, when the need arises!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Citicoline: Better Than Dietary Choline?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Citicoline: Better Than Dietary Choline?
Citicoline, also known as cytidine diphosphate-choline (or CDP-Choline, to its friends, or cytidine 5′-diphosphocholine if it wants to get fancy) is a dietary supplement that the stomach can metabolize easily for all the brain’s choline needs. What are those needs?
Choline is an essential nutrient. We technically can synthesize it, but only in minute amounts, far less than we need. Choline is a key part of the neurotransmitter acetylcholine, as well as having other functions in other parts of the body.
As for citicoline specifically… it appears to do the job better than dietary sources of choline:
❝Intriguing data, showing that on a molar mass basis citicoline is significantly less toxic than choline, are also analyzed.
It is hypothesized that, compared to choline moiety in other dietary sources such as phosphatidylcholine, choline in citicoline is less prone to conversion to trimethylamine (TMA) and its putative atherogenic N-oxide (TMAO).
Epidemiological studies have suggested that choline supplementation may improve cognitive performance, and for this application citicoline may be safer and more efficacious.❞
Source: Citicoline: A Superior Form of Choline?
Great! What does it do?
What doesn’t it do? When it comes to cognitive function, anyway, citicoline covers a lot of bases.
Short version: it improves just about every way a brain’s healthy functions can be clinically measured. From cognitive improvements in all manner of tests (far beyond just “improves memory” etc; also focus, alertness, verbal fluency, logic, computation, and more), to purely neurological things like curing tinnitus (!), alleviating mobility disorders, and undoing alcohol-related damage.
One of the reasons it’s so wide in its applications, is that it has a knock-on effect to other systems in the brain, including the dopaminergic system.
Long version: Citicoline: pharmacological and clinical review, 2022 update
(if you don’t want to sit down for a long read, we recommend skimming to the charts and figures, which are very elucidating even alone)
Spotlight study in memory
For a quick-reading example of how it helps memory specifically:
Keeping dementia at bay
For many older people looking to improve memory, it’s less a matter of wanting to perform impressive feats of memory, and more a matter of wanting to keep a sharp memory throughout our later years.
Dr. Maria Bonvicini et al. looked into this:
❝We selected seven studies including patients with mild cognitive impairment, Alzheimer’s disease or post-stroke dementia
All the studies showed a positive effect of citicoline on cognitive functions. Six studies could be included in the meta-analysis.
Overall, citicoline improved cognitive status, with pooled standardized mean differences ranging from 0.56 (95% CI: 0.37-0.75) to 1.57 (95% CI: 0.77-2.37) in different sensitivity analyses❞
The researchers concluded “yes”, and yet, called for more studies, and of higher quality. In many such studies, the heterogeneity of the subjects (often, residents of nursing homes) can be as much a problem (unclear whether the results will be applicable to other people in different situations) as it is a strength (fewer confounding variables).
Another team looked at 47 pre-existing reviews, and concluded:
❝The review found that citicoline has been proven to be a useful compound in preventing dementia progression.
Citicoline has a wide range of effects and could be an essential substance in the treatment of many neurological diseases.
Its positive impact on learning and cognitive functions among the healthy population is also worth noting.❞
Source: Application of Citicoline in Neurological Disorders: A Systematic Review
The dopamine bonus
Remember how we said that citicoline has a knock-on effect on other systems, including the dopaminergic system? This means that it’s been studied (and found meritorious) for alleviating symptoms of Parkinson’s disease:
❝Patients with Parkinson’s disease who were taking citicoline had significant improvement in rigidity, akinesia, tremor, handwriting, and speech.
Citicoline allowed effective reduction of levodopa by up to 50%.
Significant improvement in cognitive status evaluation was also noted with citicoline adjunctive therapy.❞
Source: Citicoline as Adjuvant Therapy in Parkinson’s Disease: A Systematic Review
Where to get it?
We don’t sell it, but here’s an example product on Amazon, for your convenience
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: