California Is Investing $500M in Therapy Apps for Youth. Advocates Fear It Won’t Pay Off.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With little pomp, California launched two apps at the start of the year offering free behavioral health services to youths to help them cope with everything from living with anxiety to body acceptance.
Through their phones, young people and some caregivers can meet BrightLife Kids and Soluna coaches, some who specialize in peer support or substance use disorders, for roughly 30-minute virtual counseling sessions that are best suited to those with more mild needs, typically those without a clinical diagnosis. The apps also feature self-directed activities, such as white noise sessions, guided breathing, and videos of ocean waves to help users relax.
“We believe they’re going to have not just great impact, but wide impact across California, especially in places where maybe it’s not so easy to find an in-person behavioral health visit or the kind of coaching and supports that parents and young people need,” said Gov. Gavin Newsom’s health secretary, Mark Ghaly, during the Jan. 16 announcement.
The apps represent one of the Democratic governor’s major forays into health technology and come with four-year contracts valued at $498 million. California is believed to be the first state to offer a mental health app with free coaching to all young residents, according to the Department of Health Care Services, which operates the program.
However, the rollout has been slow. Only about 15,000 of the state’s 12.6 million children and young adults have signed up for the apps, school counselors say they’ve never heard of them, and one of the companies isn’t making its app available on Android phones until summer.
Advocates for youth question the wisdom of investing taxpayer dollars in two private companies. Social workers are concerned the companies’ coaches won’t properly identify youths who need referrals for clinical care. And the spending is drawing lawmaker scrutiny amid a state deficit pegged at as much as $73 billion.
An App for That
Newsom’s administration says the apps fill a need for young Californians and their families to access professional telehealth for free, in multiple languages, and outside of standard 9-to-5 hours. It’s part of Newsom’s sweeping $4.7 billion master plan for kids’ mental health, which was introduced in 2022 to increase access to mental health and substance use support services. In addition to launching virtual tools such as the teletherapy apps, the initiative is working to expand workforce capacity, especially in underserved areas.
“The reality is that we are rarely 6 feet away from our devices,” said Sohil Sud, director of Newsom’s Children and Youth Behavioral Health Initiative. “The question is how we can leverage technology as a resource for all California youth and families, not in place of, but in addition to, other behavioral health services that are being developed and expanded.”
The virtual platforms come amid rising depression and suicide rates among youth and a shortage of mental health providers. Nearly half of California youths from the ages of 12 to 17 report having recently struggled with mental health issues, with nearly a third experiencing serious psychological distress, according to a 2021 study by the UCLA Center for Health Policy Research. These rates are even higher for multiracial youths and those from low-income families.
But those supporting youth mental health at the local level question whether the apps will move the needle on climbing depression and suicide rates.
“It’s fair to applaud the state of California for aggressively seeking new tools,” said Alex Briscoe of California Children’s Trust, a statewide initiative that, along with more than 100 local partners, works to improve the social and emotional health of children. “We just don’t see it as fundamental. And we don’t believe the youth mental health crisis will be solved by technology projects built by a professional class who don’t share the lived experience of marginalized communities.”
The apps, BrightLife Kids and Soluna, are operated by two companies: Brightline, a 5-year-old venture capital-backed startup; and Kooth, a London-based publicly traded company that has experience in the U.K. and has also signed on some schools in Kentucky and Pennsylvania and a health plan in Illinois. In the first five months of Kooth’s Pennsylvania pilot, 6% of students who had access to the app signed up.
Brightline and Kooth represent a growing number of health tech firms seeking to profit in this space. They beat out dozens of other bidders including international consulting companies and other youth telehealth platforms that had already snapped up contracts in California.
Although the service is intended to be free with no insurance requirement, Brightline’s app, BrightLife Kids, is folded into and only accessible through the company’s main app, which asks for insurance information and directs users to paid licensed counseling options alongside the free coaching. After KFF Health News questioned why the free coaching was advertised below paid options, Brightline reordered the page so that, even if a child has high-acuity needs, free coaching shows up first.
The apps take an expansive view of behavioral health, making the tools available to all California youth under age 26 as well as caregivers of babies, toddlers, and children 12 and under. When KFF Health News asked to speak with an app user, Brightline connected a reporter with a mother whose 3-year-old daughter was learning to sleep on her own.
‘It’s Like Crickets’
Despite being months into the launch and having millions in marketing funds, the companies don’t have a definitive rollout timeline. Brightline said it hopes to have deployed teams across the state to present the tools in person by midyear. Kooth said developing a strategy to hit every school would be “the main focus for this calendar year.”
“It’s a big state — 58 counties,” Bob McCullough of Kooth said. “It’ll take us a while to get to all of them.”
So far BrightLife Kids is available only on Apple phones. Brightline said it’s aiming to launch the Android version over the summer.
“Nobody’s really done anything like this at this magnitude, I think, in the U.S. before,” said Naomi Allen, a co-founder and the CEO of Brightline. “We’re very much in the early innings. We’re already learning a lot.”
The contracts, obtained by KFF Health News through a records request, show the companies operating the two apps could earn as much as $498 million through the contract term, which ends in June 2027, months after Newsom is set to leave office. And the state is spending hundreds of millions more on Newsom’s virtual behavioral health strategy. The state said it aims to make the apps available long-term, depending on usage.
The state said 15,000 people signed up in the first three months. When KFF Health News asked how many of those users actively engaged with the app, it declined to say, noting that data would be released this summer.
KFF Health News reached out to nearly a dozen California mental health professionals and youths. None of them were aware of the apps.
“I’m not hearing anything,” said Loretta Whitson, executive director of the California Association of School Counselors. “It’s like crickets.”
Whitson said she doesn’t think the apps are on “anyone’s” radar in schools, and she doesn’t know of any schools that are actively advertising them. Brightline will be presenting its tool to the counselor association in May, but Whitson said the company didn’t reach out to plan the meeting; she did.
Concern Over Referrals
Whitson isn’t comfortable promoting the apps just yet. Although both companies said they have a clinical team on staff to assist, Whitson said she’s concerned that the coaches, who aren’t all licensed therapists, won’t have the training to detect when users need more help and refer them to clinical care.
This sentiment was echoed by other school-based social workers, who also noted the apps’ duplicative nature — in some counties, like Los Angeles, youths can access free virtual counseling sessions through Hazel Health, a for-profit company. Nonprofits, too, have entered this space. For example, Teen Line, a peer-to-peer hotline operated by Southern California-based Didi Hirsch Mental Health Services, is free nationwide.
While the state is also funneling money to the schools as part of Newsom’s master plan, students and school-based mental health professionals voiced confusion at the large app investment when, in many school districts, few in-person counseling roles exist, and in some cases are dwindling.
Kelly Merchant, a student at College of the Desert in Palm Desert, noted that it can be hard to access in-person therapy at her school. She believes the community college, which has about 15,000 students, has only one full-time counselor and one part-time bilingual counselor. She and several students interviewed by KFF Health News said they appreciated having engaging content on their phone and the ability to speak to a coach, but all said they’d prefer in-person therapy.
“There are a lot of people who are seeking therapy, and people close to me that I know. But their insurances are taking forever, and they’re on the waitlist,” Merchant said. “And, like, you’re seeing all these people struggle.”
Fiscal conservatives question whether the money could be spent more effectively, like to bolster county efforts and existing youth behavioral health programs.
Republican state Sen. Roger Niello, vice chair of the Senate Budget and Fiscal Review Committee, noted that California is forecasted to face deficits for the next three years, and taxpayer watchdogs worry the apps might cost even more in the long run.
“What starts as a small financial commitment can become uncontrollable expenses down the road,” said Susan Shelley of the Howard Jarvis Taxpayers Association.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Vaping: A Lot Of Hot Air?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Vaping: A Lot Of Hot Air?
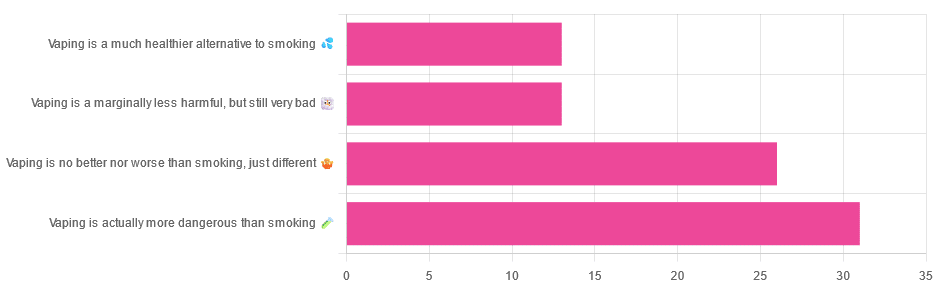
Yesterday, we asked you for your (health-related) opinions on vaping, and got the above-depicted, below-described, set of responses:
- A little over a third of respondents said it’s actually more dangerous than smoking
- A little under a third of respondents said it’s no better nor worse, just different
- A little over 10% of respondents said it’s marginally less harmful, but still very bad
- A little over 10% of respondents said it’s a much healthier alternative to smoking
So what does the science say?
Vaping is basically just steam inhalation, plus the active ingredient of your choice (e.g. nicotine, CBD, THC, etc): True or False?
False! There really are a lot of other chemicals in there.
And “chemicals” per se does not necessarily mean evil green glowing substances that a comicbook villain would market, but there are some unpleasantries in there too:
- Potential harmful health effects of inhaling nicotine-free shisha-pen vapor: a chemical risk assessment of the main components propylene glycol and glycerol
- Inflammatory and Oxidative Responses Induced by Exposure to Commonly Used e-Cigarette Flavoring Chemicals and Flavored e-Liquids without Nicotine
So, the substrate itself can cause irritation, and flavorings (with cinnamaldehyde, the cinnamon flavoring, being one of the worst) can really mess with our body’s inflammatory and oxidative responses.
Vaping can cause “popcorn lung”: True or False?
True and False! Popcorn lung is so-called after it came to attention when workers at a popcorn factory came down with it, due to exposure to diacetyl, a chemical used there.
That chemical was at that time also found in most vapes, but has since been banned in many places, including the US, Canada, the EU and the UK.
Vaping is just as bad as smoking: True or False?
False, per se. In fact, it’s recommended as a means of quitting smoking, by the UK’s famously thrifty NHS, that absolutely does not want people to be sick because that costs money:
Of course, the active ingredients (e.g. nicotine, in the assumed case above) will still be the same, mg for mg, as they are for smoking.
Vaping is causing a health crisis amongst “kids nowadays”: True or False?
True—it just happens to be less serious on a case-by-case basis to the risks of smoking.
However, it is worth noting that the perceived harmlessness of vapes is surely a contributing factor in their widespread use amongst young people—decades after actual smoking (thankfully) went out of fashion.
On the other hand, there’s a flipside to this:
Flavored vape restrictions lead to higher cigarette sales
So, it may indeed be the case of “the lesser of two evils”.
Want to know more?
For a more in-depth science-ful exploration than we have room for here…
BMJ | Impact of vaping on respiratory health
Take care!
Share This Post
-
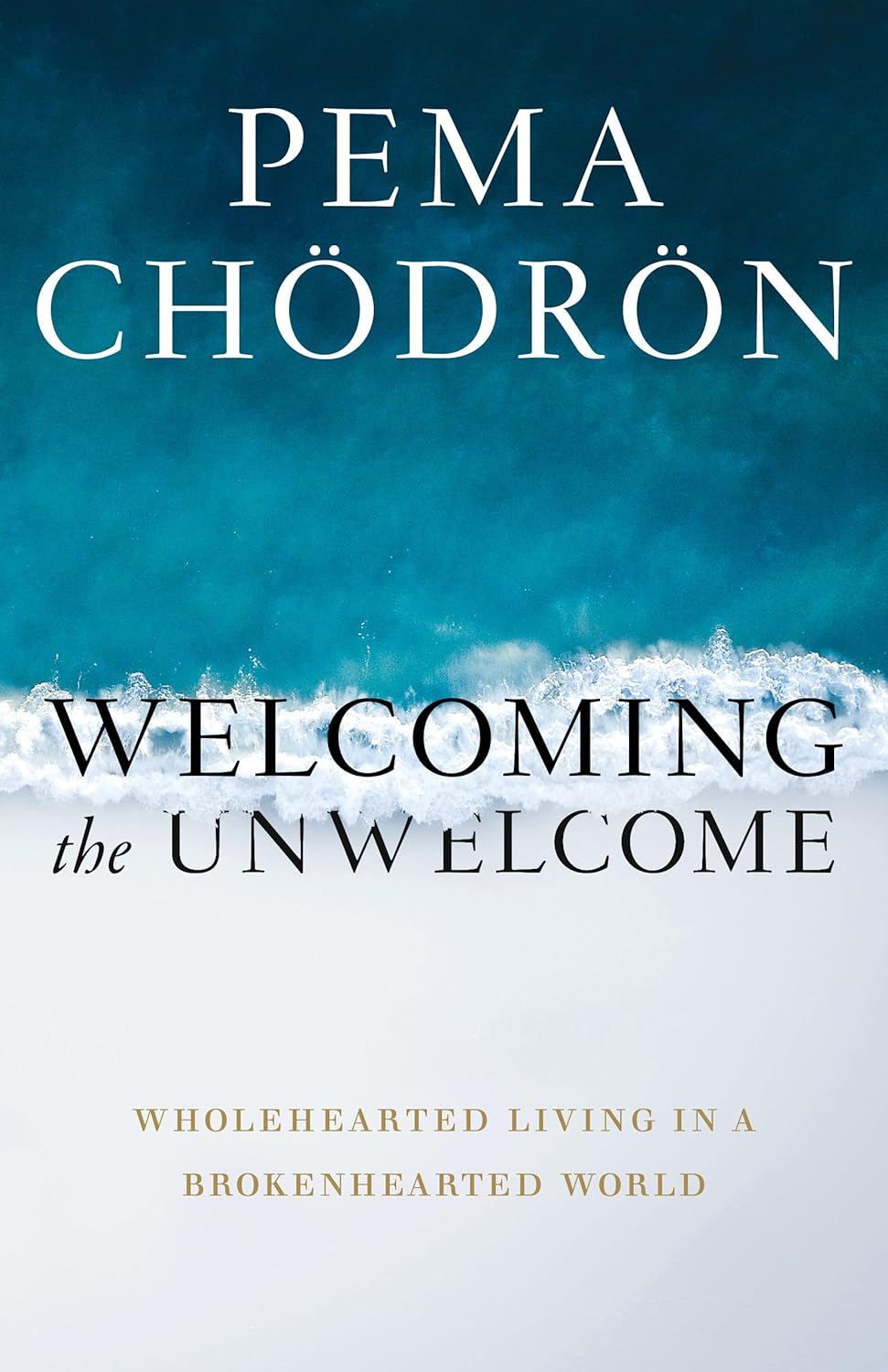
Welcoming the Unwelcome – by Pema Chödrön
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a lot in life that we don’t get to choose. Some things we have zero control over, like the weather. Others, we can only influence, like our health. Still yet others might give us an illusion of control, only to snatch it away, like a financial reversal or a bereavement.
How, then, to suffer those “slings and arrows of outrageous fortune” and come through the other side with an even mind and a whole heart?
Author Pema Chödrön has a guidebook for us.
Quick note: this book does not require the reader to have any particular religious faith to enjoy its benefits, but the author is a nun. As such, the way she describes things is generally within the frame of her religion. So that’s a thing to be aware of in case it might bother you. That said…
The largest part of her approach is one that psychology might describe as rational emotive behavioral therapy.
As such, we are encouraged to indeed “meet with triumph and disaster, and treat those two imposters just the same”, and more importantly, she lays out the tools for us to do so.
Does this mean not caring? No! Quite the opposite. It is expected, and even encouraged, that we might care very much. But: this book looks at how to care and remain compassionate, to others and to ourselves.
For Chödrön, welcoming the unwelcome is about de-toothing hardship by accepting it as a part of the complex tapestry of life, rather than something to be endured.
Bottom line: this book can greatly increase the reader’s ability to “go placidly amid the noise and haste” and bring peace to an often hectic world—starting with our own.
Share This Post
-
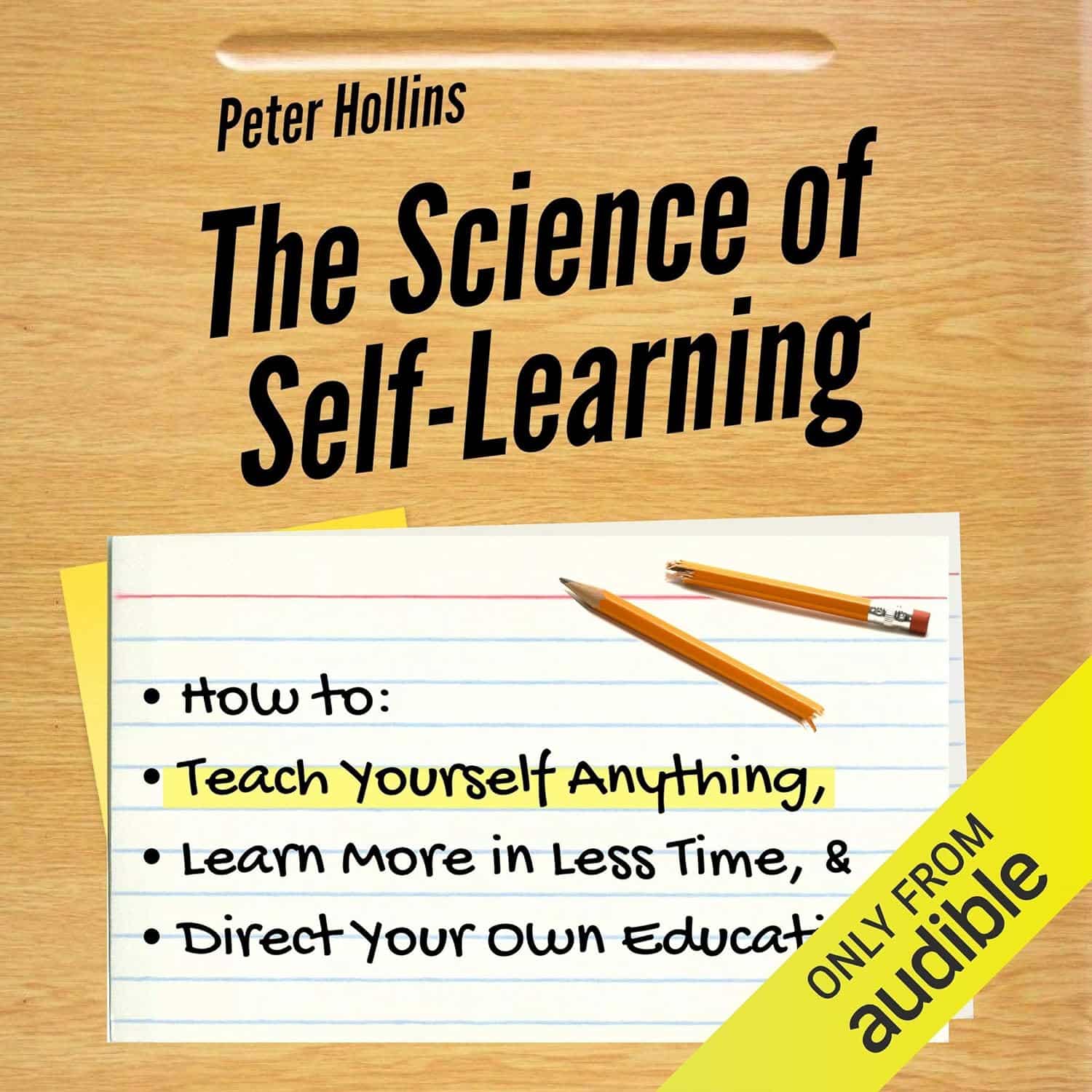
The Science of Self-Learning – by Peter Hollins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Teaching oneself new things is often the most difficult kind of bootstrapping, especially when one is unsure of such critical things as:
- Where to begin? How, for that matter, do we find where to begin?
- What can/should a learning journey look like?
- What challenges should we expect, and how will we overcome them?
Hollins answers all of these questions and more. The greatest value of this book is perhaps in its clear presentation of concrete step-by-step instructions. Hollins gives illustrated examples too, but most importantly, he gives models that can be applied to any given type of learning.
The book also covers the most difficult problems most people face when trying to learn something by themselves, including:
- Keeping oneself on-task (maintaining discipline)
- Measuring progress (self-testing beyond memorization)
- Keeping a fair pace of progress (avoiding plateaus)
- How to know when one’s knowledge is sufficient or not (avoiding Dunning-Kruger Club)
All in all, if you’re looking to learn a new subject or skill, this could be a first step that saves you a lot of time later!
Get your copy of the Science of Self-Learning on Amazon today!
Share This Post
Related Posts
-
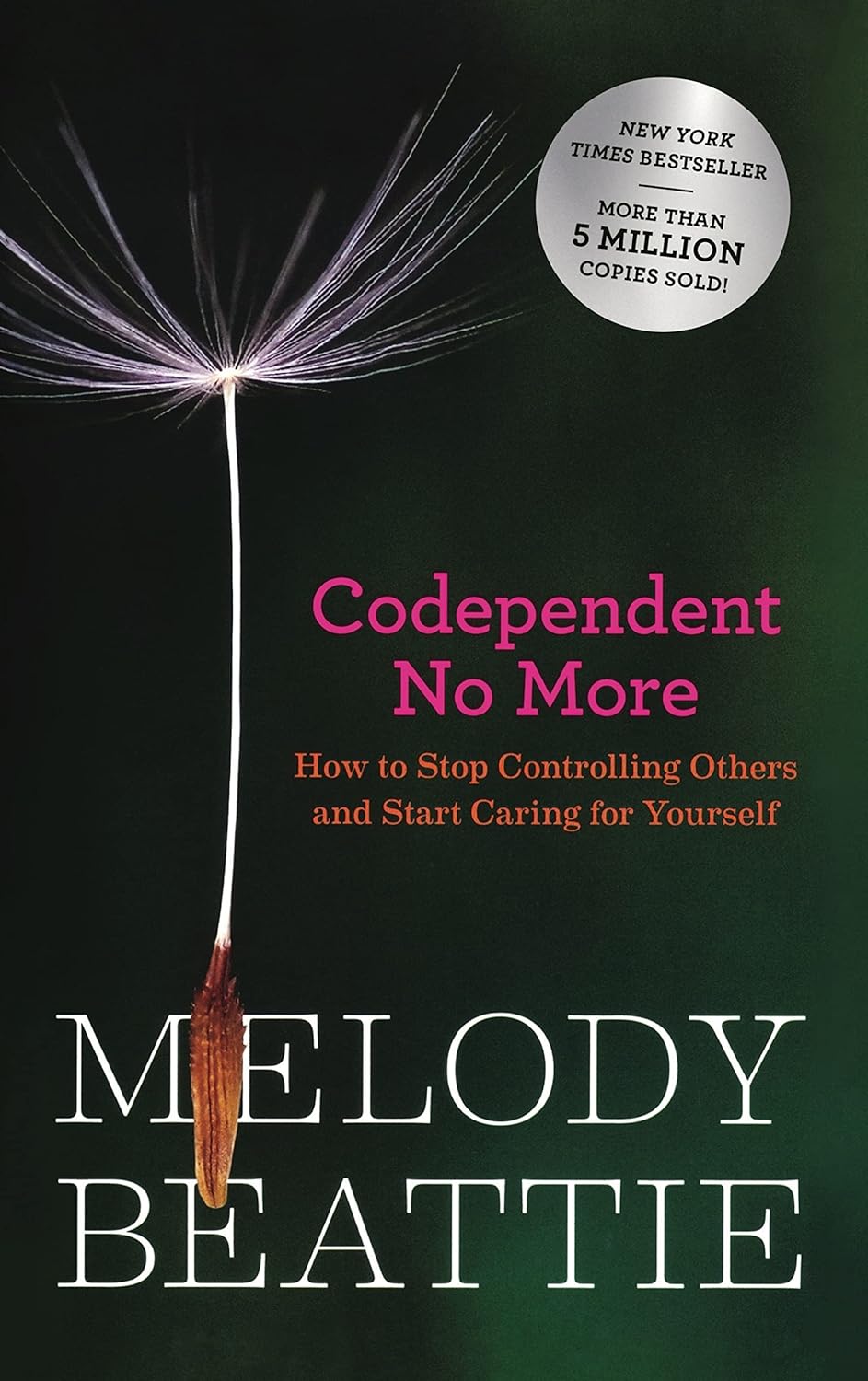
Codependent No More – by Melody Beattie
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a book review, not a book summary, but first let’s quickly cover a common misconception, because the word “codependent” gets misused a lot in popular parlance:
- What codependence isn’t: “we depend on each other and must do everything together”
- What codependence is:“person 1 has a dependency on a substance (or perhaps a behavior, such as gambling); person 2 is trying to look after person 1, and so has developed a secondary relationship with the substance/behavior. Person 2 is now said to be codependent, because it becomes all-consuming for them too, even if they’re not using the substance/behavior directly”
Funny how often it happens that the reality is more complex than the perception, isn’t it?
Melody Beattie unravels all this for us. We get a compassionate and insightful look at how we can look after ourselves, while looking after another. Perhaps most importantly: how and where to draw a line of what we can and cannot do/change for them.
Because when we love someone, of course we want to fight their battles with them, if not for them. But if we want to be their rock of strength, we can’t get lost in it too, and of course that hurts.
Beatty takes us through these ideas and more, for example:
- How to examine our own feelings even when it’s scary
- How to practice self-love and regain self-worth, while still caring for them
- How to stop being reactionary, step back, and act with purpose
If the book has any weak point, it’s that it repeatedly recommends 12-step programs, when in reality that’s just one option. But for those who wish to take another approach, this book does not require involvement in a 12-step program, so it’s not a barrier to usefulness.
Click here to check out Codependent No More and take care of yourself, too
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
People with dementia aren’t currently eligible for voluntary assisted dying. Should they be?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia is the second leading cause of death for Australians aged over 65. More than 421,000 Australians currently live with dementia and this figure is expected to almost double in the next 30 years.
There is ongoing public discussion about whether dementia should be a qualifying illness under Australian voluntary assisted dying laws. Voluntary assisted dying is now lawful in all six states, but is not available for a person living with dementia.
The Australian Capital Territory has begun debating its voluntary assisted dying bill in parliament but the government has ruled out access for dementia. Its view is that a person should retain decision-making capacity throughout the process. But the bill includes a requirement to revisit the issue in three years.
The Northern Territory is also considering reform and has invited views on access to voluntary assisted dying for dementia.
Several public figures have also entered the debate. Most recently, former Australian Chief Scientist, Ian Chubb, called for the law to be widened to allow access.
Others argue permitting voluntary assisted dying for dementia would present unacceptable risks to this vulnerable group.
Inside Creative House/Shutterstock Australian laws exclude access for dementia
Current Australian voluntary assisted dying laws exclude access for people who seek to qualify because they have dementia.
In New South Wales, the law specifically states this.
In the other states, this occurs through a combination of the eligibility criteria: a person whose dementia is so advanced that they are likely to die within the 12 month timeframe would be highly unlikely to retain the necessary decision-making capacity to request voluntary assisted dying.
This does not mean people who have dementia cannot access voluntary assisted dying if they also have a terminal illness. For example, a person who retains decision-making capacity in the early stages of Alzheimer’s disease with terminal cancer may access voluntary assisted dying.
What happens internationally?
Voluntary assisted dying laws in some other countries allow access for people living with dementia.
One mechanism, used in the Netherlands, is through advance directives or advance requests. This means a person can specify in advance the conditions under which they would want to have voluntary assisted dying when they no longer have decision-making capacity. This approach depends on the person’s family identifying when those conditions have been satisfied, generally in consultation with the person’s doctor.
Another approach to accessing voluntary assisted dying is to allow a person with dementia to choose to access it while they still have capacity. This involves regularly assessing capacity so that just before the person is predicted to lose the ability to make a decision about voluntary assisted dying, they can seek assistance to die. In Canada, this has been referred to as the “ten minutes to midnight” approach.
But these approaches have challenges
International experience reveals these approaches have limitations. For advance directives, it can be difficult to specify the conditions for activating the advance directive accurately. It also requires a family member to initiate this with the doctor. Evidence also shows doctors are reluctant to act on advance directives.
Particularly challenging are scenarios where a person with dementia who requested voluntary assisted dying in an advance directive later appears happy and content, or no longer expresses a desire to access voluntary assisted dying.
What if the person changes their mind? Jokiewalker/Shutterstock Allowing access for people with dementia who retain decision-making capacity also has practical problems. Despite regular assessments, a person may lose capacity in between them, meaning they miss the window before midnight to choose voluntary assisted dying. These capacity assessments can also be very complex.
Also, under this approach, a person is required to make such a decision at an early stage in their illness and may lose years of otherwise enjoyable life.
Some also argue that regardless of the approach taken, allowing access to voluntary assisted dying would involve unacceptable risks to a vulnerable group.
More thought is needed before changing our laws
There is public demand to allow access to voluntary assisted dying for dementia in Australia. The mandatory reviews of voluntary assisted dying legislation present an opportunity to consider such reform. These reviews generally happen after three to five years, and in some states they will occur regularly.
The scope of these reviews can vary and sometimes governments may not wish to consider changes to the legislation. But the Queensland review “must include a review of the eligibility criteria”. And the ACT bill requires the review to consider “advanced care planning”.
Both reviews would require consideration of who is able to access voluntary assisted dying, which opens the door for people living with dementia. This is particularly so for the ACT review, as advance care planning means allowing people to request voluntary assisted dying in the future when they have lost capacity.
The legislation undergoes a mandatory review. Jenny Sturm/Shutterstock This is a complex issue, and more thinking is needed about whether this public desire for voluntary assisted dying for dementia should be implemented. And, if so, how the practice could occur safely, and in a way that is acceptable to the health professionals who will be asked to provide it.
This will require a careful review of existing international models and their practical implementation as well as what would be feasible and appropriate in Australia.
Any future law reform should be evidence-based and draw on the views of people living with dementia, their family caregivers, and the health professionals who would be relied on to support these decisions.
Ben White, Professor of End-of-Life Law and Regulation, Australian Centre for Health Law Research, Queensland University of Technology; Casey Haining, Research Fellow, Australian Centre for Health Law Research, Queensland University of Technology; Lindy Willmott, Professor of Law, Australian Centre for Health Law Research, Queensland University of Technology, Queensland University of Technology, and Rachel Feeney, Postdoctoral research fellow, Queensland University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Regularity Of Sleep Can Be Even More Important Than Duration
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A recent, large (n=72,269) 8-year prospective* observational study of adults aged 40-79 has found an association between irregular sleep and major cardiovascular events.
*this means they started the study at a given point, and measured what happened for the next eight years—as opposed to a retrospective study, which would look at what had happened during the previous 8 years.
As to what qualifies as major cardiovascular events, they counted:
- Heart attack
- Cardiac arrest
- Stroke
- Cardiovascular death (any)
Irregular sleep, meanwhile, was defined per a bell curve of participants. Based on a sleep regularity index (SRI) score, those with a score of 87 or more were on the “regular” side of the curve, and those with a score of 72 or lower were on the “irregular” side of the curve.
What they found is that irregular sleep is associated with major cardiovascular events, regardless of the actual amount of sleep that people got. So in other words, you could be sleeping 9 hours per day, but if it’s a different 9 hours each day, your cardiovascular risk will still be higher.
How much higher?
- For those in the middle of the curve (so, moderate irregularity), it was 8% higher than those on the “regular” side.
- For those on the “irregular” side of the curve, it was 26% higher than those on the “regular” side.
All of the above is after taking into account confounding variables such as age, physical activity levels, discretionary screen time, fruit, vegetable, and coffee intake, alcohol consumption, smoking, mental health issues, medication use, and shift work. Which is quite something, given that shift work is a very common reason for irregular sleep schedules in a lot of people.
Limitations
While, as noted above, they did their best to account for a lot of things, this was an observational study, not an interventional study or a randomized controlled trial, and as such, it cannot truly establish cause and effect.
For example, an observational study in the 90s found that the sport most strongly associated with longevity was polo. For any unfamiliar, it’s a game played on horseback with mallets and balls. Why was this game so much better than, say, swimming? And the answer is most likely that polo is played almost entirely by very rich people. It wasn’t the sport that enhanced longevity—it was the wealth.
So similarly here, it could be for example that people who are predisposed to heart conditions, are prone to having irregular schedules. We won’t know for sure until we have interventional studies (and we probably can’t get RCTs for this, for practical reasons).
Still, it seems likely that the association is indeed causal, in which case, having a regular sleep schedule if at all possible seems like a very good way to look after one’s health.
You can read more about the study here:
Irregular sleep may elevate risk of major cardiovascular events
Practical take-away
This study strongly suggests that sleep regularity is even more important than sleep duration.
This means that there is extra reason to not sleep in past one’s normal getting-up time, even if one had a less restful night.
That’s the end of sleep that’s the most important in practical terms, too, because we can control our getting-up time, whereas we can’t really control our going-to-sleep time, because it’s perfectly possible to just lie there awake.
So, controlling the getting-up time is really the key to the whole thing. See also:
Calculate (And Enjoy) The Perfect Night’s Sleep
And for scope, you might enjoy reading:
Morning Larks vs Night Owls: How Much Can We Control Our Sleep Schedule?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: