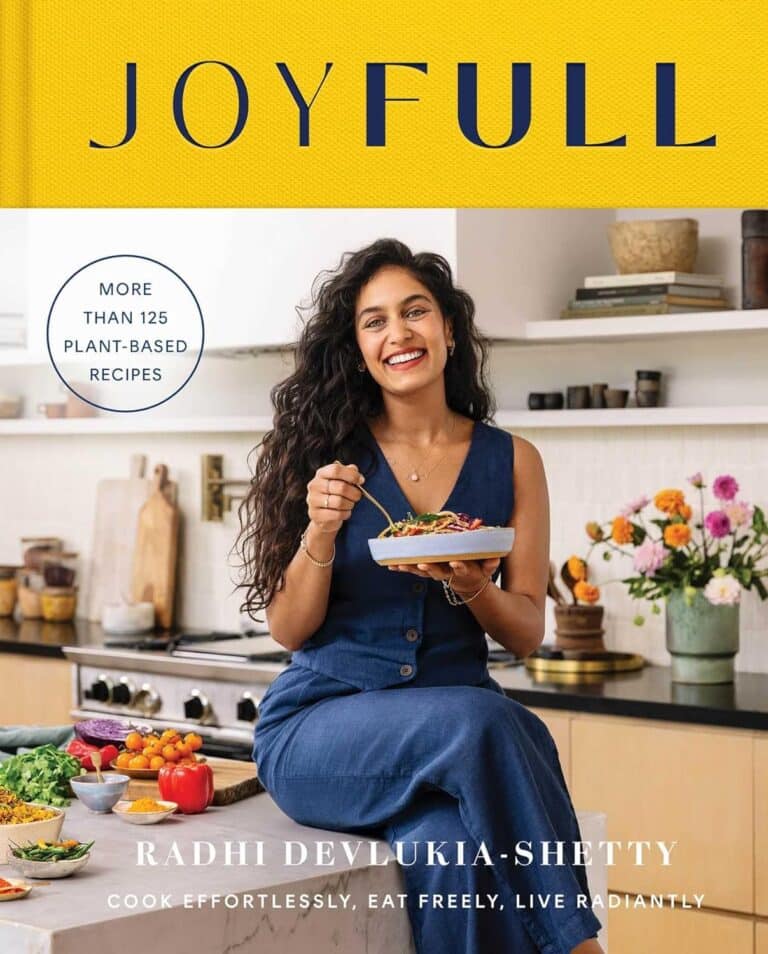
Built to Move – by Kelly starrett & Juliet Starrett
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In our everyday lives, for most of us anyway, it’s not too important to be able to run a marathon or leg-press a car. Rather more important, however, are such things as:
- being able to get up from the floor comfortably
- reach something on a high shelf without twinging a shoulder
- being able to put our socks on without making a whole plan around this task
- get accidentally knocked by an energetic dog or child and not put our back out
- etc
Starrett and Starrett, of “becoming a supple leopard” fame, lay out for us how to make sure our mobility stays great. And, if it’s not already where it needs to be, how to get there.
The “ten essential habits” mentioned in the subtitle “ten essential habits to help you move freely and live fully”, in fact also come with ten tests. No, not in the sense of arduous trials, but rather, mobility tests.
For each test, it’s explained to us how to score it out of ten (this is an objective assessment, not subjective). It’s then explained how to “level up” whatever score we got, with different advices for different levels of mobility or immobility. And if we got a ten, then of course, we just build the appropriate recommended habit into our daily life, to keep it that way.
The writing style is casual throughout, and a strong point of the book is its very clear illustrations, too.
Bottom line: if you’d like to gain/maintain good mobility (at any age), this book gives a very reliable outline for doing so.
Click here to check out Built to Move, and take care of your body!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Strawberries vs Cherries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing strawberries to cherries, we picked the cherries.
Why?
Both are great, and an argument could be made for either! But here’s our rationale:
In terms of macros, as with most fruits they are both mostly water, and have similar carbs and fiber. Nominally, cherries have the lower glycemic index, so we could call this category nominally a win for cherries, but honestly, they’re both low-GI foods and nobody is getting metabolic disease from eating strawberries, so it’s fairer to consider this category a tie.
Looking at the vitamins, strawberries have more of vitamins C, B9, E, and K, while cherries have more of vitamins A, B1, B2, B3, B5, and choline. Thus, a modest win for cherries here.
When it comes to minerals, strawberries see their day: strawberries have more iron, magnesium, manganese, and phosphorus, while cherries have more calcium, copper, and potassium. By the numbers, a win for strawberries.
So far, so tied!
What swings it into cherries’ favor is cherries’ slew of specific phytochemical benefits, including cherry-specific anti-inflammatory properties, sleep-improving abilities, and post-exercise recovery boosts, as well as anti-diabetic benefits above and beyond the normal “this is a fruit” level.
In short, both are very respectable fruits, but cherries have some extra qualities that are just special.
Of course, as ever, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Cherries’ Health Benefits Simply Pop
Enjoy!
Share This Post
-
How Your Brain Chooses What To Remember
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
During the day, your brain is simply too busy to encode memories without interfering with normal processing. At night, however…
The filing system
The brain decides which memories to keep based on significance, using sharp brain wave ripples as an internal bookmarking system. Everyday memories fade, while important events are tagged in this manner for consolidation during sleep.
How does it do this? It starts in the hippocampus, which records experiences during wakefulness and replays them repeatedly at high speed during sleep, preparing them for transfer to the neocortex.
How do we know? Uniform Manifold Approximation & Projection (UMAP) for dimension reduction is a tool that condenses 400-dimensional neural activity data into 3D for visualization. Mice navigating a maze showed hippocampal activity encoding location and learning progression; it also showed neural patterns reflecting maze layout and task mastery.
What this means in practical terms: you need to get good sleep if you don’t want to lose your memories!
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Boost Your Memory Immediately (Without Supplements)
Take care!
Share This Post
-
A short history of sunscreen, from basting like a chook to preventing skin cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australians have used commercial creams, lotions or gels to manage our skin’s sun exposure for nearly a century.
But why we do it, the preparations themselves, and whether they work, has changed over time.
In this short history of sunscreen in Australia, we look at how we’ve slathered, slopped and spritzed our skin for sometimes surprising reasons.
At first, suncreams helped you ‘tan with ease’
This early sunscreen claimed you could ‘tan with ease’.
Trove/NLASunscreens have been available in Australia since the 30s. Chemist Milton Blake made one of the first.
He used a kerosene heater to cook batches of “sunburn vanishing cream”, scented with French perfume.
His backyard business became H.A. Milton (Hamilton) Laboratories, which still makes sunscreens today.
Hamilton’s first cream claimed you could “
Sunbathe in Comfort and TAN with ease”. According to modern standards, it would have had an SPF (or sun protection factor) of 2.The mirage of ‘safe tanning’
A tan was considered a “modern complexion” and for most of the 20th century, you might put something on your skin to help gain one. That’s when “safe tanning” (without burning) was thought possible.
This 1967 Coppertone advertisement urged you to ‘tan, not burn’.
SenseiAlan/Flickr, CC BY-SASunburn was known to be caused by the UVB component of ultraviolet (UV) light. UVA, however, was thought not to be involved in burning; it was just thought to darken the skin pigment melanin. So, medical authorities advised that by using a sunscreen that filtered out UVB, you could “safely tan” without burning.
But that was wrong.
From the 70s, medical research suggested UVA penetrated damagingly deep into the skin, causing ageing effects such as sunspots and wrinkles. And both UVA and UVB could cause skin cancer.
Sunscreens from the 80s sought to be “broad spectrum” – they filtered both UVB and UVA.
Researchers consequently recommended sunscreens for all skin tones, including for preventing sun damage in people with dark skin.
Delaying burning … or encouraging it?
Up to the 80s, sun preparations ranged from something that claimed to delay burning, to preparations that actively encouraged it to get that desirable tan – think, baby oil or coconut oil. Sun-worshippers even raided the kitchen cabinet, slicking olive oil on their skin.
One manufacturer’s “sun lotion” might effectively filter UVB; another’s merely basted you like a roast chicken.
Since labelling laws before the 80s didn’t require manufacturers to list the ingredients, it was often hard for consumers to tell which was which.
At last, SPF arrives to guide consumers
In the 70s, two Queensland researchers, Gordon Groves and Don Robertson, developed tests for sunscreens – sometimes experimenting on students or colleagues. They printed their ranking in the newspaper, which the public could use to choose a product.
An Australian sunscreen manufacturer then asked the federal health department to regulate the industry. The company wanted standard definitions to market their products, backed up by consistent lab testing methods.
In 1986, after years of consultation with manufacturers, researchers and consumers, Australian Standard AS2604 gave a specified a testing method, based on the Queensland researchers’ work. We also had a way of expressing how well sunscreens worked – the sun protection factor or SPF.
This is the ratio of how long it takes a fair-skinned person to burn using the product compared with how long it takes to burn without it. So a cream that protects the skin sufficiently so it takes 40 minutes to burn instead of 20 minutes has an SPF of 2.
Manufacturers liked SPF because businesses that invested in clever chemistry could distinguish themselves in marketing. Consumers liked SPF because it was easy to understand – the higher the number, the better the protection.
Australians, encouraged from 1981 by the Slip! Slop! Slap! nationwide skin cancer campaign, could now “slop” on a sunscreen knowing the degree of protection it offered.
How about skin cancer?
It wasn’t until 1999 that research proved that using sunscreen prevents skin cancer. Again, we have Queensland to thank, specifically the residents of Nambour. They took part in a trial for nearly five years, carried out by a research team led by Adele Green of the Queensland Institute of Medical Research. Using sunscreen daily over that time reduced rates of squamous cell carcinoma (a common form of skin cancer) by about 60%.
Follow-up studies in 2011 and 2013 showed regular sunscreen use almost halved the rate of melanoma and slowed skin ageing. But there was no impact on rates of basal cell carcinoma, another common skin cancer.
By then, researchers had shown sunscreen stopped sunburn, and stopping sunburn would prevent at least some types of skin cancer.
What’s in sunscreen today?
An effective sunscreen uses one or more active ingredients in a cream, lotion or gel. The active ingredient either works:
-
“chemically” by absorbing UV and converting it to heat. Examples include PABA (para-aminobenzoic acid) and benzyl salicylate, or
-
“physically” by blocking the UV, such as zinc oxide or titanium dioxide.
Physical blockers at first had limited cosmetic appeal because they were opaque pastes. (Think cricketers with zinc smeared on their noses.)
With microfine particle technology from the 90s, sunscreen manufacturers could then use a combination of chemical absorbers and physical blockers to achieve high degrees of sun protection in a cosmetically acceptable formulation.
Where now?
Australians have embraced sunscreen, but they still don’t apply enough or reapply often enough.
Although some people are concerned sunscreen will block the skin’s ability to make vitamin D this is unlikely. That’s because even SPF50 sunscreen doesn’t filter out all UVB.
There’s also concern about the active ingredients in sunscreen getting into the environment and whether their absorption by our bodies is a problem.
Sunscreens have evolved from something that at best offered mild protection to effective, easy-to-use products that stave off the harmful effects of UV. They’ve evolved from something only people with fair skin used to a product for anyone.
Remember, slopping on sunscreen is just one part of sun protection. Don’t forget to also slip (protective clothing), slap (hat), seek (shade) and slide (sunglasses).
Laura Dawes, Research Fellow in Medico-Legal History, Australian National University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Related Posts
-
What’s the difference between ‘man flu’ and flu? Hint: men may not be exaggerating
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
The term “man flu” takes a humorous poke at men with minor respiratory infections, such as colds, who supposedly exaggerate their symptoms.
According to the stereotype, a man lies on the sofa with a box of tissues. Meanwhile his female partner, also with a snotty nose, carries on working from home, doing the chores and looking after him.
But is man flu real? Is there a valid biological reason behind men’s symptoms or are men just malingering? And how does man flu differ from flu?
baranq/Shutterstock What are the similarities?
Man flu could refer to a number of respiratory infections – a cold, flu, even a mild case of COVID. So it’s difficult to compare man flu with flu.
But for simplicity, let’s say man flu is actually a cold. If that’s the case, man flu and flu have some similar features.
Both are caused by viruses (but different ones). Both are improved with rest, fluids, and if needed painkillers, throat lozenges or decongestants to manage symptoms.
Both can share similar symptoms. Typically, more severe symptoms such as fever, body aches, violent shivering and headaches are more common in flu (but sometimes occur in colds). Meanwhile sore throats, runny noses, congestion and sneezing are more common in colds. A cough is common in both.
What are the differences?
Flu is a more serious and sometimes fatal respiratory infection caused by the influenza virus. Colds are caused by various viruses such as rhinoviruses, adenoviruses, and common cold coronaviruses, and are rarely serious.
Colds tend to start gradually while flu tends to start abruptly.Flu can be detected with laboratory or at-home tests. Man flu is not an official diagnosis.
Severe flu symptoms may be prevented with a vaccine, while cold symptoms cannot.
Serious flu infections may also be prevented or treated with antiviral drugs such as Tamiflu. There are no antivirals for colds.
OK, but is man flu real?
Again, let’s assume man flu is a cold. Do men really have worse colds than women? The picture is complicated.
One study, with the title “Man flu is not a thing”, did in fact show there were differences in men’s and women’s symptoms.
This study looked at symptoms of acute rhinosinusitis. That’s inflammation of the nasal passages and sinuses, which would explain a runny or stuffy nose, a sinus headache or face pain.
When researchers assessed participants at the start of the study, men and women had similar symptoms. But by days five and eight of the study, women had fewer or less-severe symptoms. In other words, women had recovered faster.
But when participants rated their own symptoms, we saw a somewhat different picture. Women rated their symptoms worse than how the researchers rated them at the start, but said they recovered more quickly.
All this suggests men were not exaggerating their symptoms and did indeed recover more slowly. It also suggests women feel their symptoms more strongly at the start.
Why is this happening?
It’s not straightforward to tease out what’s going on biologically.
There are differences in immune responses between men and women that provide a plausible reason for worse symptoms in men.
For instance, women generally produce antibodies more efficiently, so they respond more effectively to vaccination. Other aspects of women’s immune system also appear to work more strongly.
So why do women tend to have stronger immune responses overall? That’s probably partly because women have two X chromosomes while men have one. X chromosomes carry important immune function genes. This gives women the benefit of immune-related genes from two different chromosomes.
X chromosomes carry important immune function genes. Rost9/Shutterstock Oestrogen (the female sex hormone) also seems to strengthen the immune response, and as levels vary throughout the lifespan, so does the strength of women’s immune systems.
Men are certainly more likely to die from some infectious diseases, such as COVID. But the picture is less clear with other infections such as the flu, where the incidence and mortality between men and women varies widely between countries and particular flu subtypes and outbreaks.
Infection rates and outcomes in men and women can also depend on the way a virus is transmitted, the person’s age, and social and behavioural factors.
For instance, women seem to be more likely to practice protective behaviours such as washing their hands, wearing masks or avoiding crowded indoor spaces. Women are also more likely to seek medical care when ill.
So men aren’t faking it?
Some evidence suggests men are not over-reporting symptoms, and may take longer to clear an infection. So they may experience man flu more harshly than women with a cold.
So cut the men in your life some slack. If they are sick, gender stereotyping is unhelpful, and may discourage men from seeking medical advice.
Thea van de Mortel, Professor, Nursing, School of Nursing and Midwifery, Griffith University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Slowing the Progression of Cataracts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Understanding Cataracts
Cataracts are natural and impact everyone.
That’s a bit of a daunting opening line, but as Dr. Michele Lee, a board-certified ophthalmologist, explains, cataracts naturally develop with age, and can be accelerated by factors such as trauma, certain medications, and specific eye conditions.
We know how important your vision is to you (we’ve had great feedback about the book Vision for Life) as well as our articles on how glasses impact your eyesight and the effects of using eye drops.
While complete prevention isn’t possible, steps such as those mentioned below can be taken to slow their progression.
Here is an overview of the video’s first 3 takeaways. You can watch the whole video below.
Protect Your Eyes from Sunlight
Simply put, UV light damages lens proteins, which (significantly) contributes to cataracts. Wearing sunglasses can supposedly prevent up to 20% of cataracts caused by UV exposure.
Moderate Alcohol Consumption
We all, at some level, know that alcohol consumption doesn’t do us any good. Your eye health isn’t an exception to the rule; alcohol has been shown to contribute to cataract development.
If you’re looking at reducing your alcohol use, try reading this guide on lowering, or eradicating, alcohol consumption.
Avoid Smoking
Smokers are 2-3 times more likely to develop cataracts. Additionally, ensure good ventilation while cooking to avoid exposure to harmful indoor smoke.
See all 5 steps in the below video:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Natto vs Tempeh – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing nattō to tempeh, we picked the nattō.
Why?
Both are great, but in the battle of fermented soybeans vs fermented soybeans with extra steps, it turns out that the simplest option is the best, even if tempeh was a close runner-up:
In terms of macros, nattō has more carbs and fiber for the same protein and fat; we’ll call this category a tie or a marginal win for nattō.
In the category of vitamins, nattō has more of vitamins B1, C, E, K, and choline, while tempeh has more of vitamins B2, B3, B6, and B9. A clearer, yet still modest, win for nattō.
Minerals, however, are what really set them apart: nattō has more calcium, copper, iron, magnesium, manganese, potassium, selenium, and zinc, while tempeh has more phosphorus. An overwhelming win for nattō this time.
In short: enjoy either or both, but nattō is the more nutritionally dense option!
Want to learn more?
You might like:
21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!) ← nattō is featured as part of the diet 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: