Beyond Burger vs Beef Burger – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing the Beyond Burger to a grass-fed beef burger, we picked the Beyond Burger—but it was very close.
Why?
The macronutrient profiles of the two are almost identical, including the amount of protein, the amount of fat, and the amount of that fat that’s saturated.
Where they stand apart is in two ways:
1) Red meat is classed as a group 2A carcinogen
2) The Beyond Burger contains more sodium (about 1/5 of the daily allowance according to the AHA, or 1/4 of the daily allowance according to the WHO)
Neither of those things are great, so how to decide which is worse?
• Cancer and heart disease are both killers, with heart disease claiming more victims.
• However, we do need some sodium to live, whereas we don’t need carcinogens to live.
Tie-breaker: the sodium content in the Beyond Burger is likely to be offset by the fact that it’s a fully seasoned burger and will be eaten as-is, whereas the beef burger will doubtlessly have seasonings added before it’s eaten—which may cause it to equal or even exceed the salt content of the Beyond Burger.
The cancer risk for the beef burger, meanwhile, stays one-sided.
One thing’s for sure though: neither of them are exactly a cornerstone of a healthy diet, and either are best enjoyed as an occasional indulgence.
Some further reading:
• Lesser-Known Salt Risks
• Food Choices And Cancer Risk
• Hypertension: Factors Far More Relevant Than Salt
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lobster vs Crab – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing lobster to crab, we picked the crab.
Why?
Generally speaking, most seafood is healthy in moderation (assuming it’s well-prepared, not poisonous, and you don’t have an allergy), and for most people, these two sea creatures are indeed considered a reasonable part of a healthy balanced diet.
In terms of macros, they’re comparable in protein, and technically crab has about 2x the fat, but in both cases it’s next to nothing, so 2x almost nothing is still almost nothing. And, if we break down the lipids profiles, crab has a sufficiently smaller percentage of saturated fat (compared to monounsaturated and polyunsaturated), that crab actually has less saturated fat than lobster. In balance, the category of macros is either a tie or a slight win for crab, depending on your personal priorities.
When it comes to vitamins, crab wins easily with more of vitamins A, B1, B2, B6, B9, B12, and C, in most cases by considerable margins (we’re talking multiples of what lobster has). Lobster, meanwhile, has more of vitamin B3 (tiny margin) and vitamin B5 (pantothenic acid, as in, the vitamin that’s in basically everything edible, and thus almost impossible to be deficient in unless literally starving).
The minerals scene is more balanced; lobster has more calcium, copper, manganese, and selenium, while crab has more iron, magnesium, phosphorus, potassium, and zinc. The margins are comparable from one creature to another, so all in all the 4:5 score means a modest win for crab.
Both of these creatures are good sources of omega-3 fatty acids, but crab is better.
Lobster and crab are both somewhat high in cholesterol, but crab is the relatively lower of the two.
In short: for most people most of the time, both are fine to enjoy in moderation, but if picking one, crab is the healthier by most metrics.
Want to learn more?
You might like to read:
Shrimp vs Caviar – Which is Healthier?
Take care!
Share This Post
-
Revealed: The Soviet Secret Recipe For Success That The CIA Admits Put The US To Shame
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today’s edition of 10almonds brings you a blast from the past with a modern twist: an ancient Russian peasant food that became a Soviet staple, and today, is almost unknown in the West.
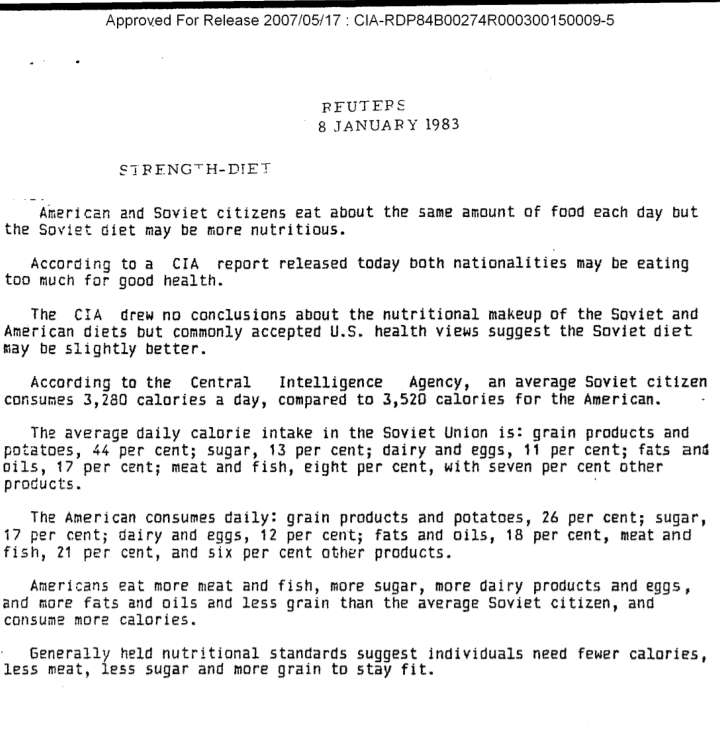
Before we get to that, let’s take a sneaky look at this declassified CIA memorandum from near the end of the Cold War:
(Click here to see a bigger version)
The take-away here is:
- Americans were eating 2–3 times more meat than Soviets
- Soviets were eating nearly double the amount of grain products and potatoes
…and both of these statistics meant that nutritionally speaking, the Soviets were doing better.
Americans also consumed more sugar and fats, which again, wasn’t the best dietary option.
But was the American diet tastier? Depends on whom you ask.
Which brings us to a literal recipe we’re going to be sharing with you today:
It’s not well-known in the West, but in Russia, it’s a famous national comfort food, a bastion of health and nutrition, and it rose to popularity because it was not only cheap and nutritious, but also, you could eat it for days without getting sick of it. And it could be easily frozen for reheating later without losing any of its appeal—it’d still be just as good.
In Russia there are sayings about it:
Щи да каша — пища наша (Shchi da kasha — pishcha nasha)
“Shchi and buckwheat are what we eat”
Top tip: buckwheat makes an excellent (and naturally sweet) alternative to porridge oats if prepared the same way!
Где щи, там и нас ищи (Gdye shchi, tam i nas ishchi)
“Where there’s shchi, us you’ll see”
Голь голью, а луковка во щах есть (Gol’ gol’yu, a lukovka vo shchakh yest’)
“I’m stark naked, but there’s shchi with onions”
There’s a very strong sentiment in Russia that really, all you need is shchi (shchi, shchi… shchi is all you need )
But what, you may ask, is shchi?
Our culinary cultural ambassador Nastja is here to offer her tried-and-tested recipe for…
…Russian cabbage soup (yes, really—bear with us now, and you can thank us later)
There are a lot of recipes for shchi (see for yourself what the Russian version of Lifehacker recommends), and we’ll be offering our favorite…
Nastja’s Nutritious and Delicious Homemade Shchi
Hi, Nastja here! I’m going to share with you my shchi recipe that is:
- Cheap
- So tasty
- Super nutritious*
- Vegan
- Gluten Free
You will also need:
- A cabbage (I use sweetheart, but any white cabbage will do)
- 1 cup (250g) red lentils (other kinds of lentils will work too)
- ½ lb or so (250–300g) tomatoes (I use baby plum tomatoes, but any kind will do)
- ½ lb or so (250–300g) mushrooms (the edible kind)
- An onion (I use a brown onion; any kind will do)
- Salt, pepper, rosemary, thyme, parsley, cumin
- Marmite or similar yeast extract (do you hate it? Me too. Trust me, it’ll be fine, you’ll love it. Omit if you’re a coward.)
- A little oil for sautéing (I use sunflower, but canola is fine, as is soy oil. Do not use olive oil or coconut oil, because the taste is too strong and the flashpoint too low)
First, what the French call mise-en-place, the prep work:
- Chop the cabbage into small strips, ⅛–¼ inch x 1 inch is a good guideline, but you can’t really go wrong unless you go to extremes
- Chop the tomatoes. If you’re using baby plum tomatoes (or cherry tomatoes), cut them in half. If using larger tomatoes, cut them into eighths (halve them, halve the halves, then halve the quarters)
- Chop the mushrooms. If using button mushrooms, half them. If using larger mushrooms, quarter them.
- Chop the onion finely.
- Gather the following kitchenware: A big pan (stock pot or similar), a sauté pan (a big wok or frying pan will do), a small frying pan (here a wok will not do), and a saucepan (a rice cook will also do)
Now, for actual cooking:
- Cook the red lentils until soft (I use a rice cooker, but a saucepan is fine) and set aside
- Sauté the cabbage, put it in the big pot (not yet on the heat!)
- Fry the mushrooms, put them in the big pot (still not yet on the heat!)
When you’ve done this a few times and/or if you’re feeling confident, you can do the above simultaneously to save time
- Blend the lentils into the water you cooked them in, and then add to the big pot.
- Turn the heat on low, and if necessary, add more water to make it into a rich soup
- Add the seasonings to taste, except the parsley. Go easy on the cumin, be generous with the rosemary and thyme, let your heart guide you with the salt and pepper.
- When it comes to the yeast extract: add about one teaspoon and stir it into the pot. Even if you don’t like Marmite, it barely changes the flavour (makes it slightly richer) and adds a healthy dose of vitamin B12.
We did not forget the tomatoes and the onion:
- Caramelize the onion (keep an eye on the big pot) and set it aside
- Fry the tomatoes and add them to the big pot
Last but definitely not least:
- Serve!
- The caramelized onion is a garnish, so put a little on top of each bowl of shchi
- The parsley is also a garnish, just add a little
Any shchi you don’t eat today will keep in the fridge for several days, or in the freezer for much longer.
*That nutritious goodness I talked about? Check it out:
- Lentils are high in protein and iron
- Cabbage is high in vitamin C and calcium
- Mushrooms are high in magnesium
- Tomatoes are good against inflammation
- Black pepper has a host of health benefits
- Yeast extract contains vitamin B12
Let us know how it went! We love to receive emails from our subscribers!
Share This Post
-
The 7 Known Risk Factors For Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A recent UK-based survey found that…
- while nearly half of adults say dementia is the disease they fear most,
- only a third of those thought you could do anything to avoid it, and
- just 1% could name the 7 known risk factors.
Quick test
Can you name the 7 known risk factors?
Please take a moment to actually try (this kind of mental stimulation is good in any case), and count them out on your fingers (or write them down), and then…
Answer (no peeking if you haven’t listed them yet)
The 7 known risk factors are:
*drumroll please*
- Smoking
- High blood pressure
- Diabetes
- Obesity
- Depression
- Lack of mental stimulation
- Lack of physical activity
How many did you get? If you got them all, well done. If not, then well, now you know, so that’s good.
Did you come here from our “Future-Proof Your Brain” article? If so, you can get back to it here ← and if you didn’t, you should check it out anyway; it’s worth it😉
Take care!
Share This Post
Related Posts
-
How much does your phone’s blue light really delay your sleep? Relax, it’s just 2.7 minutes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s one of the most pervasive messages about technology and sleep. We’re told bright, blue light from screens prevents us falling asleep easily. We’re told to avoid scrolling on our phones before bedtime or while in bed. We’re sold glasses to help filter out blue light. We put our phones on “night mode” to minimise exposure to blue light.
But what does the science actually tell us about the impact of bright, blue light and sleep? When our group of sleep experts from Sweden, Australia and Israel compared scientific studies that directly tested this, we found the overall impact was close to meaningless. Sleep was disrupted, on average, by less than three minutes.
We showed the message that blue light from screens stops you from falling asleep is essentially a myth, albeit a very convincing one.
Instead, we found a more nuanced picture about technology and sleep.
Mangostar/Shutterstock What we did
We gathered evidence from 73 independent studies with a total of 113,370 participants of all ages examining various factors that connect technology use and sleep.
We did indeed find a link between technology use and sleep, but not necessarily what you’d think.
We found that sometimes technology use can lead to poor sleep and sometimes poor sleep can lead to more technology use. In other words, the relationship between technology and sleep is complex and can go both ways.
How is technology supposed to harm sleep?
Technology is proposed to harm our sleep in a number of ways. But here’s what we found when we looked at the evidence:
- bright screen light – across 11 experimental studies, people who used a bright screen emitting blue light before bedtime fell asleep an average of only 2.7 minutes later. In some studies, people slept better after using a bright screen. When we were invited to write about this evidence further, we showed there is still no meaningful impact of bright screen light on other sleep characteristics including the total amount or quality of sleep
- arousal is a measure of whether people become more alert depending on what they’re doing on their device. Across seven studies, people who engaged in more alerting or “exciting” content (for example, video games) lost an average of only about 3.5 minutes of sleep compared to those who engaged in something less exciting (for example, TV). This tells us the content of technology alone doesn’t affect sleep as much as we think
- we found sleep disruption at night (for example, being awoken by text messages) and sleep displacement (using technology past the time that we could be sleeping) can lead to sleep loss. So while technology use was linked to less sleep in these instances, this was unrelated to being exposed to bright, blue light from screens before bedtime.
Which factors encourage more technology use?
Research we reviewed suggests people tend to use more technology at bedtime for two main reasons:
- to “fill the time” when they’re not yet sleepy. This is common for teenagers, who have a biological shift in their sleep patterns that leads to later sleep times, independent of technology use.
- to calm down negative emotions and thoughts at bedtime, for apparent stress reduction and to provide comfort.
There are also a few things that might make people more vulnerable to using technology late into the night and losing sleep.
We found people who are risk-takers or who lose track of time easily may turn off devices later and sacrifice sleep. Fear of missing out and social pressures can also encourage young people in particular to stay up later on technology.
What helps us use technology sensibly?
Last of all, we looked at protective factors, ones that can help people use technology more sensibly before bed.
The two main things we found that helped were self-control, which helps resist the short-term rewards of clicking and scrolling, and having a parent or loved one to help set bedtimes.
We found having a parent or loved one to help set bedtimes encourages sensible use of technology. fast-stock/Shutterstock Why do we blame blue light?
The blue light theory involves melatonin, a hormone that regulates sleep. During the day, we are exposed to bright, natural light that contains a high amount of blue light. This bright, blue light activates certain cells at the back of our eyes, which send signals to our brain that it’s time to be alert. But as light decreases at night, our brain starts to produce melatonin, making us feel sleepy.
It’s logical to think that artificial light from devices could interfere with the production of melatonin and so affect our sleep. But studies show it would require light levels of about 1,000-2,000 lux (a measure of the intensity of light) to have a significant impact.
Device screens emit only about 80-100 lux. At the other end of the scale, natural sunlight on a sunny day provides about 100,000 lux.
What’s the take-home message?
We know that bright light does affect sleep and alertness. However our research indicates the light from devices such as smartphones and laptops is nowhere near bright or blue enough to disrupt sleep.
There are many factors that can affect sleep, and bright, blue screen light likely isn’t one of them.
The take-home message is to understand your own sleep needs and how technology affects you. Maybe reading an e-book or scrolling on socials is fine for you, or maybe you’re too often putting the phone down way too late. Listen to your body and when you feel sleepy, turn off your device.
Chelsea Reynolds, Casual Academic/Clinical Educator and Clinical Psychologist, College of Education, Psychology and Social Work, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Resistance Beyond Weights
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Resistance, Your Way
We’ve talked before about the importance of resistance training:
Resistance Is Useful! (Especially As We Get Older)
And we’ve even talked about how to make resistance training more effective:
(High Intensity Interval Training, but make it High Intensity Resistance Training)
Which resistance training exercises are best?
There are two reasonable correct answers here:
- The resistance training exercises that you will actually do (because it’s no good knowing the best exercise ever if you’re not going to do it because it is in some way offputting to you)
- The resistance training exercises that will prevent you from getting a broken bone in the event of some accident or incident
This latter is interesting, because when people think resistance training, the usually immediate go-to exercises are often things like the bench press, or the chest machine in the gym.
But ask yourself: how often do we hear about some friend or relative who in their old age has broken their humerus?
It can happen, for sure, but it’s not as often as breaking a hip, a tarsal (ankle bones), or a carpal (wrist bones).
So, how can we train to make those bones strong?
Strong bones grow under strong muscles
When archaeologists dig up a skeleton from a thousand years ago, one of the occupations that’s easy to recognize is an archer. Why?
An archer has an unusual frequent exercise: pushing with their left arm while pulling with their right arm. This will strengthen different muscles on each side, and thus, increase bone density in different places on each arm. The left first metacarpal and right first and second metacarpals and phalanges are also a giveaway.
This is because: one cannot grow strong muscles on weak bones (or else the muscles would just break the bones), so training muscles will force the body to strengthen the relevant bones.
So: if you want strong bones, train the muscles attached to those bones
This answers the question of “how am I supposed to exercise my hips” etc.
Weights, bodyweight, resistance bands
If you go to the gym, there’s a machine for everything, and a member of gym staff will be able to advise which of their machines will strengthen which muscles.
If you train with free weights at home:
- Wrist curls (forearm supported and stationary, lifting a dumbbell in your hand, palm-upwards) will strengthen the wrist
- The farmer’s walk (carrying a heavy weight in each hand) will also strengthen your wrist
- A modified version of this involves holding the weight with just your fingertips, and then raising and lowering it by curling and uncurling your fingers)
- Lateral leg raises (you will need ankle-weights for this) will strengthen your ankles and your hips, as will hip abductions (as in today’s featured video), especially with a weight attached.
- Ankle raises (going up on your tip-toes and down again, repeat) while holding weights in your hands will strengthen your ankles
If you don’t like weights:
- Press-ups will strengthen your wrists
- Fingertip press-ups are even better: to do these, do your press-ups as normal, except that the only parts of your hands in contact with the ground are your fingertips
- This same exercise can be done the other way around, by doing pull-ups
- And that same “even better” works by doing pull-ups, but holding the bar only with one’s fingertips, and curling one’s fingers to raise oneself up
- Lateral leg raises and hip abductions can be done with a resistance band instead of with weights. The great thing about these is that whereas weights are a fixed weight, resistance bands will always provide the right amount of resistance (because if it’s too easy, you just raise your leg further until it becomes difficult again, since the resistance offered is proportional to how much tension the band is under).
Remember, resistance training is still resistance training even if “all” you’re resisting is gravity!
If it fells like work, then it’s working
As for the rest of preparing to get older?
Check out:
Training Mobility Ready For Later Life
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ovarian cancer is hard to detect. Focusing on these 4 symptoms can help with diagnosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ovarian cancers are often found when they are already advanced and hard to treat.
Researchers have long believed this was because women first experienced symptoms when ovarian cancer was already well-established. Symptoms can also be hard to identify as they’re vague and similar to other conditions.
But a new study shows promising signs ovarian cancer can be detected in its early stages. The study targeted women with four specific symptoms – bloating, abdominal pain, needing to pee frequently, and feeling full quickly – and put them on a fast track to see a specialist.
As a result, even the most aggressive forms of ovarian cancer could be detected in their early stages.
So what did the study find? And what could it mean for detecting – and treating – ovarian cancer more quickly?
Ground Picture/Shutterstock Why is ovarian cancer hard to detect early?
Ovarian cancer cannot be detected via cervical cancer screening (which used to be called a pap smear) and pelvic exams aren’t useful as a screening test.
Current Australian guidelines recommend women get tested for ovarian cancer if they have symptoms for more than a month. But many of the symptoms – such as tiredness, constipation and changes in menstruation – are vague and overlap with other common illnesses.
This makes early detection a challenge. But it is crucial – a woman’s chances of surviving ovarian cancer are associated with how advanced the cancer is when she is diagnosed.
If the cancer is still confined to the original site with no spread, the five-year survival rate is 92%. But over half of women diagnosed with ovarian cancer first present when the cancer has already metastatised, meaning it has spread to other parts of the body.
If the cancer has spread to nearby lymph nodes, the survival rate is reduced to 72%. If the cancer has already metastasised and spread to distant sites at the time of diagnosis, the rate is only 31%.
There are mixed findings on whether detecting ovarian cancer earlier leads to better survival rates. For example, a trial in the UK that screened more than 200,000 women failed to reduce deaths.
That study screened the general public, rather than relying on self-reported symptoms. The new study suggests asking women to look for specific symptoms can lead to earlier diagnosis, meaning treatment can start more quickly.
What did the new study look at?
Between June 2015 and July 2022, the researchers recruited 2,596 women aged between 16 and 90 from 24 hospitals across the UK.
They were asked to monitor for these four symptoms:
- persistent abdominal distension (women often refer to this as bloating)
- feeling full shortly after starting to eat and/or loss of appetite
- pelvic or abdominal pain (which can feel like indigestion)
- needing to urinate urgently or more often.
Women who reported at least one of four symptoms persistently or frequently were put on a fast-track pathway. That means they were sent to see a gynaecologist within two weeks. The fast track pathway has been used in the UK since 2011, but is not specifically part of Australia’s guidelines.
Some 1,741 participants were put on this fast track. First, they did a blood test that measured the cancer antigen 125 (CA125). If a woman’s CA125 level was abnormal, she was sent to do a internal vaginal ultrasound.
What did they find?
The study indicates this process is better at detecting ovarian cancer than general screening of people who don’t have symptoms. Some 12% of women on the fast-track pathway were diagnosed with some kind of ovarian cancer.
A total of 6.8% of fast-tracked patients were diagnosed with high-grade serous ovarian cancer. It is the most aggressive form of cancer and responsible for 90% of ovarian cancer deaths.
Out of those women with the most aggressive form, one in four were diagnosed when the cancer was still in its early stages. That is important because it allowed treatment of the most lethal cancer before it had spread significantly through the body.
There were some promising signs in treating those with this aggressive form. The majority (95%) had surgery and three quarters (77%) had chemotherapy. Complete cytoreduction – meaning all of the cancer appears to have been removed – was achieved in six women out of ten (61%).
It’s a promising sign that there may be ways to “catch” and target ovarian cancer before it is well-established in the body.
What does this mean for detection?
The study’s findings suggest this method of early testing and referral for the symptoms leads to earlier detection of ovarian cancer. This may also improve outcomes, although the study did not track survival rates.
It also points to the importance of public awareness about symptoms.
Clinicians should be able to recognise all of the ways ovarian cancer can present, including vague symptoms like general fatigue.
But empowering members of the general public to recognise a narrower set of four symptoms can help trigger testing, detection and treatment of ovarian cancer earlier than we thought.
This could also save GPs advising every woman who has general tiredness or constipation to undergo an ovarian cancer test, making testing and treatment more targeted and efficient.
Many women remain unaware of the symptoms of ovarian cancer. This study shows recognising them may help early detection and treatment.
Jenny Doust, Clinical Professorial Research Fellow, Australian Women and Girls’ Health Research Centre, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: