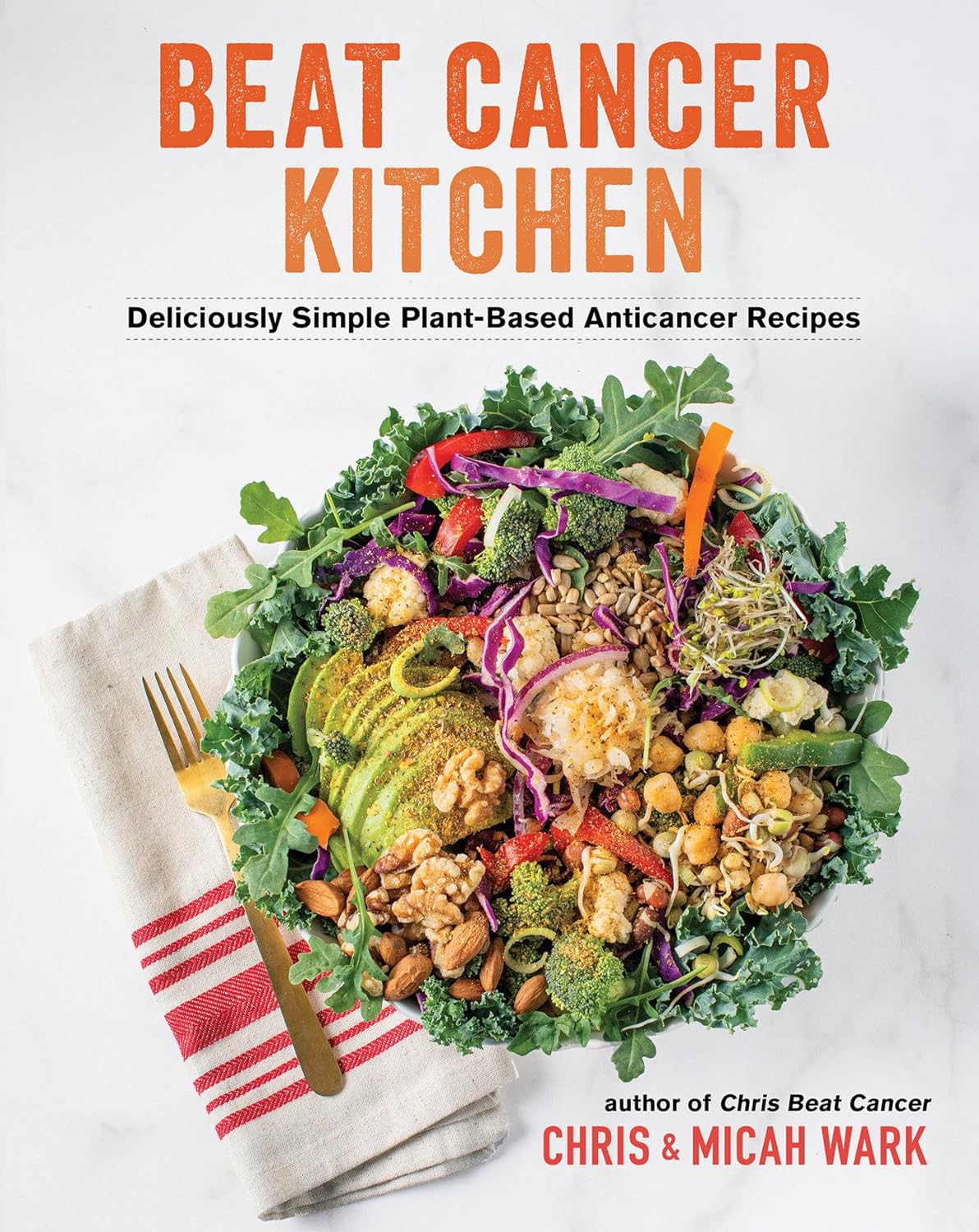
Beat Cancer Kitchen – by Chris Wark & Micah Wark
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When we eat, many things can increase our cancer risk. Some we might remember to avoid, like ultra-processed foods and red meat. Others might be more neutral when it comes to cancer, neither good nor bad.
But! Some foods also have cancer-fighting properties. Which means reducing cancer risk, and/or having an anti-proliferative effect (i.e., shrinks or at least slows growth of tumors), in the event of already having cancer.
That’s what Chris & Micah Wark are offering here; a cookbook built around anti-cancer foods—after the former beat his own cancer with the help of the latter. He had surgery, but skipped chemo, preferring to look to nutrition to keep cancer-free. Now 18 years later, and so far, so good.
The dietary advice here is entirely consistent with what we’d offer at 10almonds; it’s plant-based, and high in anti-cancer phytonutrients.
The recipes themselves (of which there are about 70-ish) are as delicious and simple as the title suggests, and/but you might want to know:
- On the one hand, many recipes are things like sauces, condiments, or dressings, which in a recipe book can sometimes feel like underdelivering on the promise of recipes when we expect full meals
- On the other hand, those things if you just purchase them ready-made are usually the things with the most ultra-processed products, thus, having anticancer homemade versions instead here can actually make a very big difference
- On the third hand, there areplenty of starters/mains/desserts too!
Bottom line: if you’re looking for an anti-cancer cookbook, this is a very good one whose ingredients aren’t obscure (which can otherwise be a problem for some books of this kind)
Click here to check out Beat Cancer Kitchen, and take good care of yourself and your loved ones!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Starfruit vs Soursop – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing starfruit to soursop, we picked the soursop.
Why?
First, by starfruit, we also mean carambola, which is a different name for the same fruit, and by soursop we also mean graviola/guyabano/guanábana, which are different namers for the same fruit. Now, as for their health qualities:
In terms of macros, the soursop has more carbs and fiber, the ratio of which also give it the lower glycemic index. So, a win for soursop here.
When it comes to vitamins, starfruit has more of vitamins A, B5, C, and E, while soursop has more of vitamins B1, B2, B3, B6, B7, B9, and K. Another win for soursop.
In the category of minerals, starfruit has slightly more copper, manganese, and zinc, while soursop has much more calcium, iron, magnesium, phosphorus, and potassium. One more win for soursop!
Adding up the sections makes for a clear and overwhelming win for soursop, but let’s address to quick safety considerations while we’re here:
- Soursop extract has been claimed to be an effective cancer treatment. It isn’t. There is no evidence for this at all; just one unscrupulous company that spread the claims.
- Soursop contains annonacin, a neurotoxin. That sounds scary, but much like with apple seeds and cyanide, the quantities you’d have to consume to suffer ill effects are absurd. Remember how capsaicin (as found in hot peppers) is also a neurotoxin, too and has many health benefits. Humans have a long and happy tradition of enjoying things that are toxic at high doses, but in small doses are neutral or even beneficial. Pretty much all things we can consume (including oxygen, and water) are toxic at sufficient doses.
In short, both of these fruits are fine and good, neither will treat cancer, but both will help to keep you in good health. As for nutritional density, the soursop wins in every category.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← soursop has no special cancer treatment properties, but actual evidence shows these fruits are beneficial (being good as a preventative, and also definitely a worthy adjunct to—but not a replacement for—mainstream anticancer therapies if you have cancer).
Take care!
Share This Post
-
The Many Health Benefits Of Garlic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Many Health Benefits of Garlic
We’re quite confident you already know what garlic is, so we’re going to leap straight in there with some science today:
First, let’s talk about allicin
Allicin is a compound in garlic that gives most of its health benefits. A downside of allicin is that it’s not very stable, so what this means is:
- Garlic is best fresh—allicin breaks down soon after garlic is cut/crushed
- So while doing the paperwork isn’t fun, buying it as bulbs is better than buying it as granules or similar
- Allicin also breaks down somewhat in cooking, so raw garlic is best
- Our philosophy is: still use it in cooking as well; just use more!
- Supplements (capsule form etc) use typically use extracts and potency varies (from not great to actually very good)
Read more about that:
- Short-term heating reduces the anti-inflammatory effects of fresh raw garlic extracts
- Allicin Bioavailability and Bioequivalence from Garlic Supplements and Garlic Foods
Now, let’s talk benefits…
Benefits to heart health
Garlic has been found to be as effective as the drug Atenolol at reducing blood pressure:
It also lowers LDL (bad cholesterol):
Benefits to the gut
We weren’t even looking for this, but as it turns out, as an add-on to the heart benefits…
Benefits to the immune system
Whether against the common cold or bringing out the heavy guns, garlic is a booster:
- Preventing the common cold with a garlic supplement: a double-blind, placebo-controlled survey
- Supplementation with aged garlic extract improves both NK and γδ-T cell function and reduces the severity of cold and flu symptoms: a randomized, double-blind, placebo-controlled nutrition intervention
Benefits to the youthfulness of body and brain
Garlic is high in antioxidants that, by virtue of reducing oxidative stress, help slow aging. This effect, combined with the cholesterol and blood pressure benefits, means it may also reduce the risk of Alzheimer’s and other forms of dementia:
- Antioxidant health effects of aged garlic extract
- Effects of garlic consumption on plasma and erythrocyte antioxidant parameters in elderly subjects
- Garlic reduces heart disease and dementia risk
There are more benefits too…
That’s all we have time to dive into study-wise today, but for the visually-inclined, here are yet more benefits to garlic (at a rate of 3–4 cloves per day):
An incredible awesome recipe using lots of garlic:
- Take small potatoes (still in their skins), cut in half
- Add enough peeled cloves of garlic so that you have perhaps a 1:10 ratio of garlic to potato by mass
- Boil (pressure-cooking is ideal) until soft, and drain
- Keeping them in the pan, add a lashing of olive oil, and any additional seasonings per your preference (consider black pepper, rosemary, thyme, parsley)
- Put a lid on the pan, and holding it closed, shake the pan vigorously
- Note: if you didn’t leave the skins on, or you chopped much larger potatoes smaller instead of cutting in half, the potatoes will break up into a rough mash now. This is actually also fine and still tastes (and honestly, looks) great, but it is different, so just be aware, so that you get the outcome you want.
- The garlic, which—unlike the potatoes—didn’t have a skin to hold it together, will now have melted over the potatoes like butter
You can serve like this (it’s delicious already) or finish up in the oven or air-fryer or under the grill, if you prefer a roasted style dish (an amazing option too).
Share This Post
- Garlic is best fresh—allicin breaks down soon after garlic is cut/crushed
-
Nudge – by Richard Thaler & Cass Sunstein
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How often in life do we make a suboptimal decision that ends up plaguing us for a long time afterwards? Sometimes, a single good or bad decision can even directly change the rest of our life.
So, it really is important that we try to optimize the decisions we do make.
Professors Richard Thaler and Cass Sunstein look at all kinds of decision-making in this book. Their goal, as per the subtitle, is “improving decisions about health, wealth, and happiness”.
For the most part, the book concentrates on “nudges”. Small factors that influence our decisions one way or another.
Most importantly: that some of them are very good reasons to be nudged; others, very bad ones. And they often look similar.
Where this book excels is in highlighting the many ways we make decisions without even thinking about it… or we think about it, but only down a prescribed, foreseen track, to an externally expected conclusion (for example, an insurance company offering three packages, but two of them exist only to direct you to the “correct” choice).
A weakness of the book is that in some aspects it’s a little inconsistent. The authors describe their economic philosophy as “libertarian paternalism”, and as libertarians they’re against mandates, except when as paternalists they’re for them. But, if we take away their labels, this boils down to “some mandates can be good and some can be bad”, which would not be so inconsistent after all.
Bottom line: if you’d like to better understand your own decision-making processes through the eyes of policy-setting economists (especially Sunstein, who worked for the White House Office of Information & Regulatory Affairs) whose job it is to make sure you make the “right” decisions, then this is a very enlightening book.
Click here to check out Nudge and improve your decision-making clarity!
Share This Post
Related Posts
-
Random Acts of Medicine – by Dr. Anupam Jena & Dr. Christopher Worsham
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We talked recently of small things that can change how productive your doctor’s appointment is, and this book is a more scientific version of that, and on a grander scale.
The author use what they call “natural experiments”, essentially observational studies, to determine what factors beyond the obvious affect health outcomes. With this approach, they address such questions as why kids with summer birthdays are more likely to get the flu, and why heart attack outcomes improve when there’s a cardiologists’ convention elsewhere. And many more such things that can seem like non-causal correlation, until one examines the causative factors, and controls (in the statistical analysis; remember this is still entirely observational, so no interventions are made) for other potential confounding factors.
They also look at what factors influence doctors’ decisions in ways they certainly shouldn’t, but they do, because doctors are as prone to biases as everyone else. And, for that matter, what factors influence patients’ decisions in ways they certainly shouldn’t—for the same reason. The authors acknowledge that they themselves are not immune, and you, dear reader, are not immune either.
Nevertheless, the practical value in this book comes from trying to at least be more aware of such things, the better to either leverage them, or at least ensure you don’t fall foul of them.
The style is conversational pop-science, making for quite light reading, albeit with many footnotes and a respectable bibliography.
Bottom line: if you’d like to understand more about the machinations that decide who lives and who dies (especially when sometimes it will be you or a loved one who lives or dies), then this is a fascinating book that that delves deeply into that.
Click here to check out Random Acts Of Medicine, and be aware!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What families should know about whooping cough
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Whooping cough is a bacterial respiratory illness that can cause long-term symptoms and even death.
- Two types of vaccines protect against it: The DTap vaccine is given to babies and children up to 6 years old, while the Tdap vaccine is given to children 7 years and older and adults.
- If you or your child has symptoms of whooping cough, isolate them from vulnerable family members and seek treatment early to reduce the risk of serious illness.
Whooping cough, also called pertussis, is a highly contagious respiratory illness that’s particularly dangerous for babies. Cases are now at least four times as high as they were at this time last year. Fortunately, vaccines are extremely effective at preventing the disease across age groups.
Read on to learn about the symptoms and risks of whooping cough, who should get vaccinated, and what to do when symptoms appear.What are the symptoms of whooping cough?
Early symptoms of whooping cough typically appear five to 10 days after exposure and may include a runny or stuffy nose, a low fever, and a mild cough. One to two weeks later, some people may experience extreme coughing fits that can cause shortness of breath, trouble sleeping, vomiting, fatigue, and rib fractures. These fits usually last one to six weeks, but they can last up to 10 weeks after infection.
About one in three babies under 1 year old who contract whooping cough require hospitalization, as they may experience life-threatening pauses in breathing (called apnea), pneumonia, and other complications. Children and adults who have asthma or are immunocompromised are also more likely to develop severe symptoms.
Which vaccines protect against whooping cough, and who is eligible?
Two types of vaccines protect against whooping cough: The DTap vaccine is given to babies and children up to 6 years old, while the Tdap vaccine is given to children 7 years and older and adults. Both vaccines protect against infections from diptheria, tetanus, and pertussis.
The Centers for Disease Control and Prevention recommends that pregnant people receive a single dose of the Tdap vaccine between 27 and 36 weeks of pregnancy, as this lowers the risk of whooping cough in babies younger than 2 months old by 78 percent.
Multiple doses are required for the best protection. Learn more about DTaP and Tdap vaccine schedules from the CDC, and talk to your health care provider about how many doses you and your children need.
What should families do when whooping cough symptoms appear?
If you or your child has symptoms of whooping cough, isolate the infected person from vulnerable family members. It’s also important to seek treatment early to reduce the risk of serious illness. Health care providers typically prescribe antibiotics to those recovering at home.
Over-the-counter cough and cold medicine is not recommended for children under 4 years old. However, limiting smoke, dust, and chemical fumes at home and using a humidifier can reduce coughing. If you are caring for someone with whooping cough who exhibits pauses in breathing or develops gray or blue skin, call 911 immediately.
For more information, talk to your health care provider.Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Brain Fog Fix – by Dr. Mike Dow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The three weeks mentioned in the subtitle is in fact a week-by-week plan:
- Adjusting diet (inclusions and exclusions) and cognitive strategies
- Focusing on sleep, exercise, and memory-boosting “brain games”
- Bringing in the social aspect, and connection to something larger than oneself
In this reviewer’s opinion, a week is too short a time to completely overhaul one’s diet; most changes need to be gradual, so doing several at once in a week is quite extreme. But, even if it takes a month for each stage instead of a week, the method is reasonable.
The nutritional advice is good, and consistent with current best science on the topic. There’s a lot about keeping even blood sugars and improving insulin sensitivity, as well as doing what is best for the heart and blood in general (e.g. fiber, managing triglycerides, doing the right kinds of exercise, etc).
As a psychotherapist, he also talks a fair bit about neurotransmitters, and making sure one’s gut and brain are fed appropriately to keep the correct balance (remembering for example that serotonin is made in the gut, and dopamine is made in the brain). Unlike many of his colleagues, he’s not a fan of medicating beyond absolute necessity.
The style is a little salesy for this reviewer’s personal taste—but then again, perhaps he made the reasonable assumption that a person reading a book entitled “the brain fog fix” needs their attention grabbing and re-grabbing every paragraph or so. As such, maybe it’s not a bad call.
Bottom line: if you have brain fog and would like to not have brain fog, this book offers a scientifically sound, evidence-based, holistic approach that can certainly improve things.
Click here to check out The Brain Fog Fix, and fix your brain fog!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: