Antibiotics? Think Thrice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Antibiotics: Useful Even Less Often Than Previously Believed (And Still Just As Dangerous)
You probably already know that antibiotics shouldn’t be taken unless absolutely necessary. Not only does taking antibiotics frivolously increase antibiotic resistance (which is bad, and kills people), but also…
It’s entirely possible for the antibiotics to not only not help, but instead wipe out your gut’s “good bacteria” that were keeping other things in check.
Those “other things” can include fungi like Candida albicans.
Candida, which we all have in us to some degree, feeds on sugar (including the sugar formed from breaking down alcohol, by the way) and refined carbs. Then it grows, and puts its roots through your intestinal walls, linking with your neural system. Then it makes you crave the very things that will feed it and allow it to put bigger holes in your intestinal walls.
Don’t believe us? Read: Candida albicans-Induced Epithelial Damage Mediates Translocation through Intestinal Barriers
(That’s scientist-speak for “Candida puts holes in your intestines, and stuff can then go through those holes”)
And as for how that comes about, it’s like we said:
See also: Candida albicans as a commensal and opportunistic pathogen in the intestine
That’s not all…
And that’s just C. albicans, never mind things like C. diff. that can just outright kill you easily.
We don’t have room to go into everything here, but you might like to check out:
Four Ways Antibiotics Can Kill You
It gets worse (now comes the new news)
So, what are antibiotics good for? Surely, for clearing up chesty coughs, lower respiratory tract infections, right? It’s certainly one of the two things that antibiotics are most well-known for being good at and often necessary for (the other being preventing/treating sepsis, for example in serious and messy wounds).
But wait…
A large, nationwide (US) observational study of people who sought treatment in primary or urgent care settings for lower respiratory tract infections found…
(drumroll please)
…the use of antibiotics provided no measurable impact on the severity or duration of coughs even if a bacterial infection was present.
Read for yourself:
And in the words of the lead author of that study,
❝Lower respiratory tract infections tend to have the potential to be more dangerous, since about 3% to 5% of these patients have pneumonia. But not everyone has easy access at an initial visit to an X-ray, which may be the reason clinicians still give antibiotics without any other evidence of a bacterial infection.❞
So, what’s to be done about this? On a large scale, Dr. Merenstein recommends:
❝Serious cough symptoms and how to treat them properly needs to be studied more, perhaps in a randomized clinical trial as this study was observational and there haven’t been any randomized trials looking at this issue since about 2012.❞
This does remind us that, while not a RCT, there is a good ongoing observational study that everyone with a smartphone can participate in:
Dr. Peter Small’s medical AI: “The Cough Doctor”
In the meantime, he advises that when COVID and SARS have been ruled out, then “basic symptom-relieving medications plus time brings a resolution to most people’s infections”.
You can read a lot more detail here:
Antibiotics aren’t effective for most lower tract respiratory infections
In summary…
Sometimes, antibiotics really are a necessary and life-saving medication. But most of the time they’re not, and given their great potential for harm, they may be best simultaneously viewed as the very dangerous threat they also are, and used only when those “heavy guns” are truly what’s required.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Link Between Introversion & Sensory Processing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve talked before about how to beat loneliness and isolation, and how that’s important for all of us, including those of us on the less social end of the scale.
However, while we all need at least the option of social contact in order to be at our best, there’s a large portion of the population who also need to be able to retreat to somewhere quiet to recover from too much social goings-on.
Clinically speaking, this sometimes gets called introversion, or at least a negative score for extroversion on the “Big Five Inventory”, the only personality-typing system that actually gets used in science. Today we’re going to be focusing on a term that typically gets applied to those generally considered introverts:
The “highly sensitive person”
This makes it sound like a very rare snowflake condition, when in fact the diagnostic criteria yield a population bell curve of 30:40:30, whereupon 30% are in the band of “high sensitivity”, 40% “normal sensitivity” and the remaining 30% “low sensitivity”.
You may note that “high” and “low” together outnumber “normal”, but statistics is like that. It is interesting to note, though, that this statistical spread renders it not a disorder, so much as simply a description.
You can read more about it here:
Sensory-processing sensitivity and its relation to introversion and emotionality
What it means in practical terms
Such a person will generally seek solitude more frequently during the day than others will, and it’s not because of misanthropy (at least, statistically speaking it’s not; can’t speak for individuals!), but rather, it’s about needing downtime after what has felt like too much sensory processing resulting:
If this need for solitude is not met (sometimes it’s simply not practicable), then it can lead to overwhelm.
Sidenote about overwhelm: pick your battles! No, pick fewer than that. Put some back. That’s still too many 😜
Back to seriousness: if you’re the sort of person to walk into a room and immediately do the Sherlock Holmes thing of noticing everything about everyone, who is doing what, what has changed about the room since last time you were there, etc… Then that’s great; it’s a sign of a sharp mind, but it’s also a lot of information to process and you’re probably going to need a little decompression afterwards:
This is the biological equivalent of needing to let an overworked computer or phone cool down after excessive high-intensity use of its CPU.
The same goes if you’re the sort of person who goes into “performance mode” when in company, is “the life and soul of the party” etc, and/or perhaps “the elegant hostess”, but needs to then collapse afterwards because it’s more of a role you play than your natural inclination.
Take care of your battery
To continue the technological metaphor from earlier, if you repeatedly overuse a device without allowing it cooldown periods, it will break down (and if it’s a certain generation of iPhone, it might explode).
Similarly, if you repeatedly overuse your own highly sensitive senses (such as being often in social environment where there’s a lot going on) without allowing yourself adequate cooldown periods, you will break down (or indeed, explode: not literally, but some people are prone to emotional outbursts after bottling things up).
None of this is good for the health, not in the short term and not in the long term, either:
With that in mind, take care to take care of yourself, meeting your actual needs instead of just those that get socially assumed.
Want to take the test?
Here’s a two-minute test (results available immediately right there on-screen; no need to give your email or anything) 😎
Want to know more?
We reviewed this book about playing to one’s strengths in the context of sensitivity, a while back, and highly recommend it:
Sensitive – by Jenn Granneman and Andre Sólo
Enjoy!
Share This Post
-
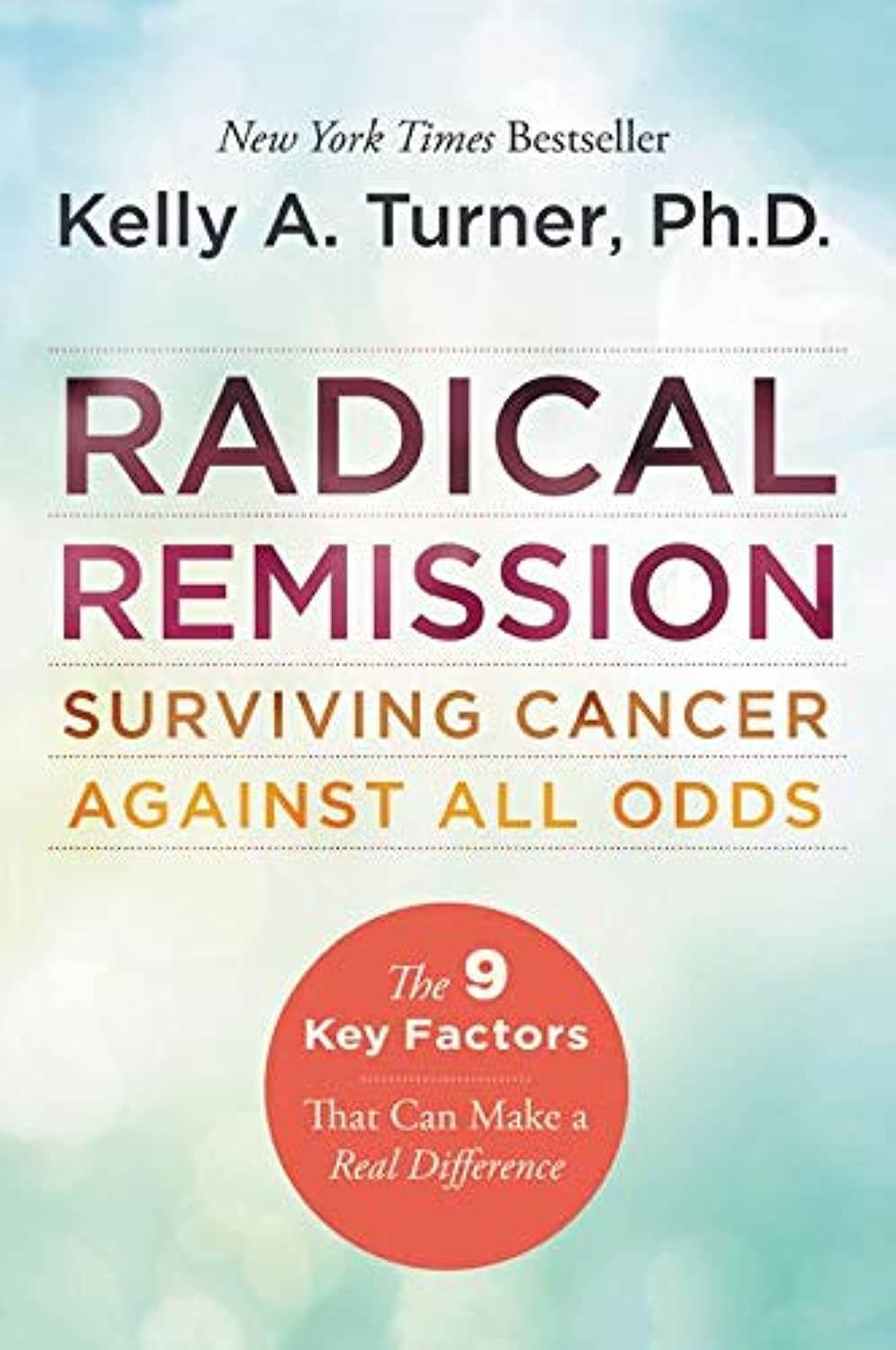
Radical Remission – by Dr. Kelly Turner
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not:an autobiographical account of the “I beat cancer and you can too” pep-talk style.
What it is: a very readable pop-science book based on the author’s own PhD research into radical remission.
She knew that a very small percentage of people experience spontaneous radical remission (or quasi-spontaneous, if the remission is attributed to lifestyle changes, and/or some alternative therapy), but a small percentage of people means a large number worldwide, so she travelled the world studying over 1,000 cases of people with late-stage cancer who had either not gone for conventional anticancer drugs, or had and then stopped, and lived to tell the tale.
While she doesn’t advocate for any particular alternative therapy, she does report on what things came to her attention. She does advocate for some lifestyle changes.
Perhaps the biggest value this book offers is in its promised “9 key factors that can make a real difference”, which are essentially her conclusions from her PhD dissertation.
There isn’t room to talk about them here in a way that wouldn’t be misleading/unhelpful for a paucity of space, so perhaps we’ll do a main feature one of these days.
Bottom line: if you have (or a loved one has) cancer, this is an incredibly sensible book to read. If you don’t, then it’s an interesting and thought-provoking book to read.
Click here to check out Radical Remission, and learn about the factors at hand!
Share This Post
-
Apples vs Carrots – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apples to carrots, we picked the carrots.
Why?
Both are sweet crunchy snacks, both rightly considered very healthy options, but one comes out clearly on top…
Both contain lots of antioxidants, albeit mostly different ones. They’re both good for this.
Looking at their macros, however, apples have more carbs while carrots have more fiber. The carb:fiber ratio in apples is already sufficient to make them very healthy, but carrots do win.
In the category of vitamins, carrots have many times more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, K, and choline. Apples are not higher in any vitamins.
In terms of minerals, carrots have a lot more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Apples are not higher in any minerals.
If “an apple a day keeps the doctor away”, what might a carrot a day do?
Want to learn more?
You might like to read:
Sugar: From Apples to Bees, and High-Fructose C’s
Take care!
Share This Post
Related Posts
-
The Inflammation Spectrum – by Dr. Will Cole
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Cole’s other book “Gut Feelings”, and now he’s back, this time to tackle inflammation.
The focus here is on understanding what things trigger inflammation in your body—personally yours, not someone else’s—by something close to the usual elimination process yes, but he offers a way of sliding into it gently instead of simply quitting all the things and gradually adding everything back in.
The next step he takes the reader through is eating not just to avoid triggering inflammation, but to actively combat it. From there, it should be possible for the reader to build an anti-inflammatory cookbook, that’s not only one’s own personal repertoire of cooking, but also specifically tailored to one’s own personal responses to different ingredients.
The style of this book is very pop-science, helpful, walking-the-reader-by-the-hand through the processes involved. Dr. Cole wants to make everything as easy as possible.
Bottom line: if your diet could use an anti-inflammatory revamp, this is a top-tier guidebook for doing just that.
Click here to check out The Inflammation Spectrum, find your food triggers and reset your system!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From Strength to Strength – by Dr. Arthur Brooks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For most professions, there are ways in which performance can be measured, and the average professional peak varies by profession, but averages are usually somewhere in the 30–45 range, with a pressure to peak between 25–35.
With a peak by age 45 or perhaps 50 at the latest (aside from some statistical outliers, of course), what then to expect at age 50+? Not long after that, there’s a reason for mandatory retirement ages in some professions.
Dr. Brooks examines the case for accepting that rather than fighting it, and/but making our weaknesses into our strengths as we go. If our fluid intelligence slows, our accumulated crystal intelligence (some might call it “wisdom“) can make up for it, for example.
But he also champions the idea of looking outside of ourselves; of the importance of growing and fostering connections; giving to those around us and receiving support in turn; not transactionally, but just as a matter of mutualism of the kind found in many other species besides our own. Indeed, Dr. Brooks gives the example of a grove of aspen trees (hence the cover art of this book) that do exactly that.
The style is very accessible in terms of language but with frequent scientific references, so very much a “best of both worlds” in terms of readability and information-density.
Bottom line: if ever you’ve wondered at what age you might outlive your usefulness, this book will do as the subtitle suggests, and help you carve out your new place.
Click here to check out From Strength To Strength, and find yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
For women with antenatal depression, micronutrients might help them and their babies – new study
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Getty Images Julia J Rucklidge, University of Canterbury; Elena Moltchanova, University of Canterbury; Roger Mulder, University of Otago, and Siobhan A Campbell, University of Canterbury
Antenatal depression affects 15% to 21% of pregnant women worldwide. It can influence birth outcomes and children’s development, as well as increase the risk of post-natal depression.
Current treatments like therapy can be inaccessible and antidepressants can carry risks for developing infants.
Over the past two decades, research has highlighted that poor nutrition is a contributing risk factor to mental health challenges. Most pregnant women in New Zealand aren’t adhering to nutritional guidelines, according to a longitudinal study. Only 3% met the recommendations for all food groups.
Another cohort study carried out in Brazil shows that ultra-processed foods (UPF) accounted for at least 30% of daily dietary energy during pregnancy, displacing healthier options.
UPFs are chemically manufactured and contain additives to improve shelf life, as well as added sugar and salt. Importantly, they are low in essential micronutrients (vitamins and minerals).
The consumption of these foods is concerning because a nutrient-poor diet during pregnancy has been linked to poorer mental health outcomes in children. This includes depression, anxiety, hyperactivity, and inattention.
Increasing nutrients in maternal diets and reducing consumption of UPFs could improve the mental health of the mother and the next generation. Good nutrition can have lifelong benefits for the offspring.
However, there are multiple factors that mean diet change alone may not in itself be sufficient to address mental health challenges. Supplementing with additional nutrients may also be important to address nutritional needs during pregnancy.
Micronutrients as treatment for depression
Our earlier research suggests micronutrient supplements for depression have benefits outside pregnancy.
But until now there have been no published randomised controlled trials specifically designed to assess the efficacy and safety of broad-spectrum micronutrients on antenatal depression and overall functioning.
The NUTRIMUM trial, which ran between 2017 and 2022, recruited 88 women in their second trimester of pregnancy who reported moderate depressive symptoms. They were randomly allocated to receive either 12 capsules (four pills, three times a day) of a broad-spectrum micronutrient supplement or an active placebo containing iodine and riboflavin for a 12-week period.
Micronutrient doses were generally between the recommended dietary allowance and the tolerable upper level.
Based on clinician ratings, micronutrients significantly improved overall psychological functioning compared to the placebo. The findings took into account all noted changes based on self-assessment and clinician observations. This includes sleep, mood regulation, coping, anxiety and side effects.
Adding micronutrients to the diet of pregnant women with antenatal depression significantly improved their overall psychological functioning. Getty Images Both groups reported similar reductions in symptoms of depression. More than three quarters of participants were in remission at the end of the trial. But 69% of participants in the micronutrient group rated themselves as “much” or “very much” improved, compared to 39% in the placebo group.
Participants taking the micronutrients also experienced significantly greater improvements in sleep and overall day-to-day functioning, compared to participants taking the placebo. There were no group differences on measures of stress, anxiety and quality of life.
Importantly, there were no group differences in reported side effects, and reports of suicidal thoughts dropped over the course of the study for both groups. Blood tests confirmed increased vitamin levels (vitamin C, D, B12) and fewer deficiencies in the micronutrient group.
Micronutrients were particularly helpful for women with chronic mental health challenges and those who had taken psychiatric medications in the past. Those with milder symptoms improved with or without the micronutrients, suggesting general care and monitoring might suffice for some women.
The benefits of micronutrients were comparable to psychotherapy but with less contact. There are no randomised controlled trials of antidepressant medication to compare these results.
Retention in the study was good (81%) and compliance excellent (90%).
Beyond maternal mental health
We followed the infants of mothers enrolled in the NUTRIMUM trial (who were therefore exposed to micronutrients during pregnancy) for 12 months, alongside infants from the general population of Aotearoa New Zealand.
This second group of infants from the general population contained a smaller sub-group who were exposed to antidepressant medication for the treatment of antenatal depression.
We assessed the neuro-behavioural development of each infant within the first four weeks of life, and temperament up to one year after birth.
These observational follow-ups showed positive effects of micronutrients on the infants’ ability to regulate their behaviour. These results were on par with or better than typical pregnancies, and better than treatments with antidepressants.
Micronutrients during pregnancy improved the neurological and behavioural development of infants. Getty Images Infants exposed to micronutrients during pregnancy were significantly better at attending to external stimuli. They were also better able to block out external stimuli during sleep. They showed fewer signs of stress and had better muscle tone compared to infants not exposed to micronutrients.
They also displayed greater ability to interact with their environment. They were better at regulating their emotional state and had fewer abnormal muscle reflexes than infants exposed to antidepressant medication in pregnancy.
Reassuringly, micronutrients had no negative impact on infant temperament.
These findings highlight the potential of micronutrients as a safe and effective alternative to traditional medication treatments for antenatal depression.
The prenatal environment sets the foundation for a child’s future. Further investigation into the benefits of micronutrient supplementation would gives us more confidence in their use for other perinatal (from the start of pregnancy to a year after birth) mental health issues. This could provide future generations with a better start to life.
We would like to acknowledge the contribution of Dr Hayley Bradley to this research project.
Julia J Rucklidge, Professor of Psychology, University of Canterbury; Elena Moltchanova, Professor of Statistics, University of Canterbury; Roger Mulder, Professor of Psychiatry, University of Otago, and Siobhan A Campbell, Intern Psychologist, Researcher – Te Puna Toiora (Mental Health and Nutrition Research Lab), University of Canterbury
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: