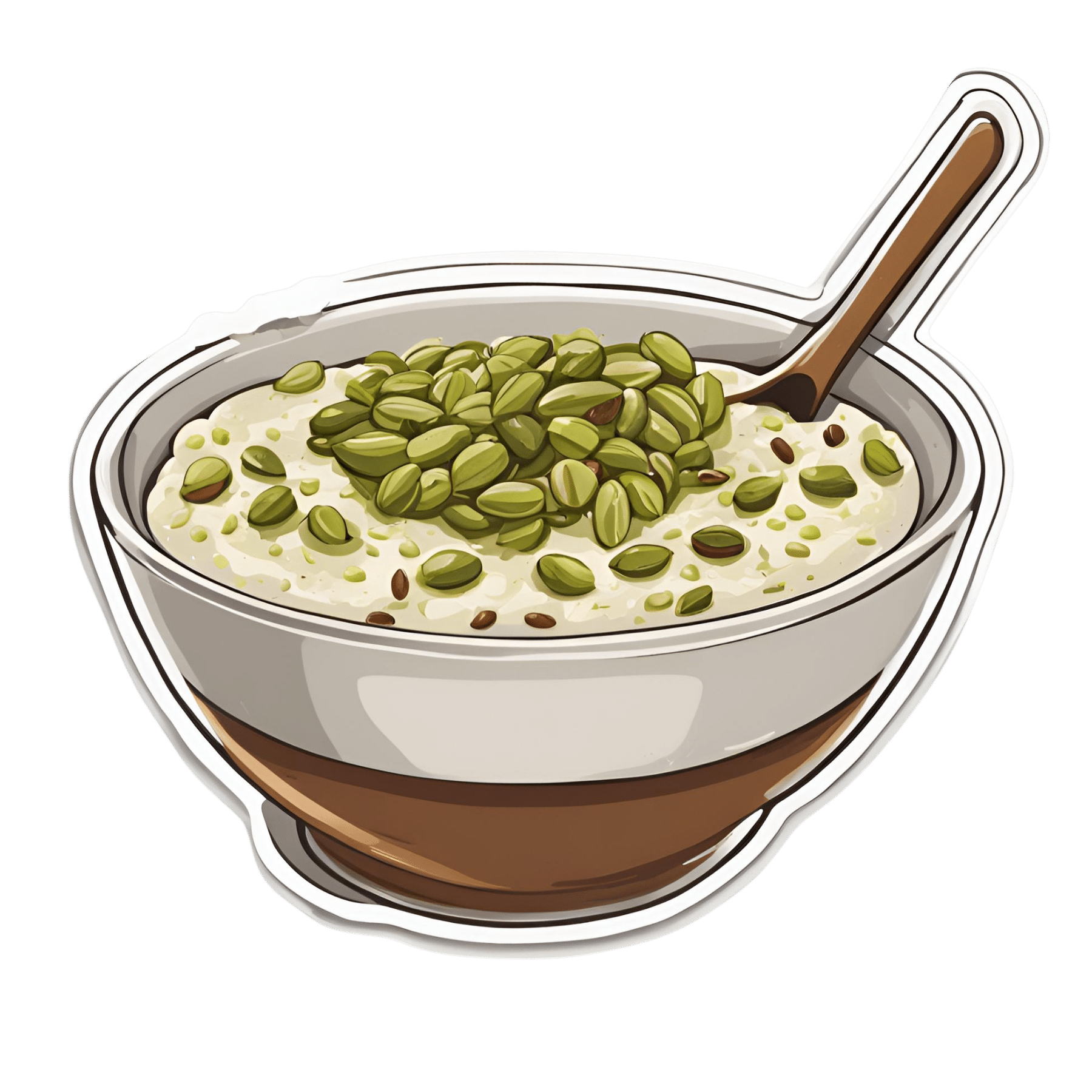
Anti-Cholesterol Cardamom & Pistachio Porridge
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This tasty breakfast’s beta-glucan content binds to cholesterol and carries it out of the body; there are lots of other nutritional benefits too!
You will need
- 1 cup coconut milk
- ⅓ cup oats
- 4 tbsp crushed pistachios
- 6 cardamom pods, crushed
- 1 tsp rose water or 4 drops edible rose essential oil
- Optional sweetener: drizzle of honey or maple syrup
- Optional garnishes: rose petals, chopped nuts, dried fruit
Method
(we suggest you read everything at least once before doing anything)
1) Heat the coconut milk, adding the oats and crushed cardamom pods. Simmer for 5–10 minutes depending on how cooked you want the oats to be.
2) Stir in the crushed pistachio nuts, as well as the rose water.
3) Serve in a bowl, adding any optional toppings:

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The Best Kind Of Fiber For Overall Health? ← it’s beta-glucan, which is fund abundantly in oats
- Pistachios vs Pecans – Which is Healthier? ← have a guess
- Can Saturated Fats Be Healthy? ← coconut can!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cranberry juice really can help with UTIs – and reduce reliance on antibiotics
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cranberry juice has been used medicinally for centuries. Our new research indicates it should be a normal aspect of urinary tract infection (UTI) management today.
While some benefits of cranberry compounds for the prevention of UTIs have been suspected for some time, it hasn’t been clear whether the benefits from cranberry juice were simply from drinking more fluid, or something in the fruit itself.
For our study, published this week, we combined and collectively assessed 3,091 participants across more than 20 clinical trials.
Our analysis indicates that increasing liquids reduces the rate of UTIs compared with no treatment, but cranberry in liquid form is even better at reducing UTIs and antibiotic use.
Julie Falk/Flickr, CC BY-NC-ND Are UTIs really that bad?
Urinary tract infections affect more than 50% of women and 20% of men in their lifetime.
Most commonly, UTIs are caused from the bug called Escherichia coli (E.coli). This bug lives harmlessly in our intestines, but can cause infection in the urinary tract. This is why, particularly for women, it is recommended people wipe from front to back after using the toilet.
An untreated UTI can move up to the kidneys and cause even more serious illness.
Even when not managing infection, many people are anxious about contracting a UTI. Sexually active women, pregnant women and older women may all be at increased risk.
Why cranberries?
To cause a UTI, the bacteria need to attach to the wall of the urinary bladder. Increasing fluids helps to flush out bacteria before it attaches (or makes its way up into the bladder).
Some beneficial compounds in cranberry, such as proanthocyanidins (also called condensed tannins), prevent the bacteria from attaching to the wall itself.
While there are treatments, over 90% of the bugs that cause UTIs exhibit some form of microbial resistance. This suggests that they are rapidly changing and some cases of UTI might be left untreatable.
The juice of cranberries has long been thought to have infection-fighting properties. duckeesue/Shutterstock What we found
Our analysis showed a 54% lower rate of UTIs from cranberry juice consumption compared to no treatment. This means that significantly fewer participants who regularly consumed cranberry juice (most commonly around 200 millilitres each day) reported having a UTI during the periods assessed in the studies we analysed.
Cranberry juice was also linked to a 49% lower rate of antibiotic use than placebo liquid and a 59% lower rate than no treatment, based on analysis of indirect and direct effects across six studies. The use of cranberry compounds, whether in drinks or tablet form, also reduced the prevalence of symptoms associated with UTIs.
While some studies we included presented conflicts of interest (such as receiving funding from cranberry companies), we took this “high risk of bias” into account when analysing the data.
The study found extra hydration helped but not to the same extent as cranberry juice. Pixelshot/Shutterstock So, when can cranberry juice help?
We found three main benefits of cranberry juice for UTIs.
1. Reduced rates of infections
Increasing fluids (for example, drinking more water) reduced the prevalence of UTIs, and taking cranberry compounds (such as tablets) was also beneficial. But the most benefits were identified from increasing fluids and taking cranberry compounds at the same time, such as with cranberry juice.
2. Reduced use of antibiotics
The data shows cranberry juice lowers the need to use antibiotics by 59%. This was identified as fewer participants in randomised cranberry juice groups required antibiotics.
Increasing fluid intake also helped reduce antibiotic use (by 25%). But this was not as useful as increasing fluids at the same time as using cranberry compounds.
Cranberry compounds alone (such as tablets without associated increases in fluid intake) did not affect antibiotic use.
3. Reducing symptoms
Taking cranberry compounds (in any form, liquid or tablet) reduced the symptoms of UTIs, as measured in the overall data, by more than five times.
Take home advice
While cranberry juice cannot treat a UTI, it can certainly be part of UTI management.
If you suspect that you have a UTI, see your GP as soon as possible.
Christian Moro, Associate Professor of Science & Medicine, Bond University and Charlotte Phelps, Senior Teaching Fellow, Medical Program, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
A person in Texas caught bird flu after mixing with dairy cattle. Should we be worried?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The United States’ Centers for Disease Control and Prevention (CDC) has issued a health alert after the first case of H5N1 avian influenza, or bird flu, seemingly spread from a cow to a human.
A farm worker in Texas contracted the virus amid an outbreak in dairy cattle. This is the second human case in the US; a poultry worker tested positive in Colorado in 2022.
The virus strain identified in the Texan farm worker is not readily transmissible between humans and therefore not a pandemic threat. But it’s a significant development nonetheless.
Some background on bird flu
There are two types of avian influenza: highly pathogenic or low pathogenic, based on the level of disease the strain causes in birds. H5N1 is a highly pathogenic avian influenza.
H5N1 first emerged in 1997 in Hong Kong and then China in 2003, spreading through wild bird migration and poultry trading. It has caused periodic epidemics in poultry farms, with occasional human cases.
Influenza A viruses such as H5N1 are further divided into variants, called clades. The unique variant causing the current epidemic is H5N1 clade 2.3.4.4b, which emerged in late 2020 and is now widespread globally, especially in the Americas.
In the past, outbreaks could be controlled by culling of infected birds, and H5N1 would die down for a while. But this has become increasingly difficult due to escalating outbreaks since 2021.
Wild animals are now in the mix
Waterfowl (ducks, swans and geese) are the main global spreaders of avian flu, as they migrate across the world via specific routes that bypass Australia. The main hub for waterfowl to migrate around the world is Quinghai lake in China.
But there’s been an increasing number of infected non-waterfowl birds, such as true thrushes and raptors, which use different flyways. Worryingly, the infection has spread to Antarctica too, which means Australia is now at risk from different bird species which fly here.
H5N1 has escalated in an unprecedented fashion since 2021, and an increasing number of mammals including sea lions, goats, red foxes, coyotes, even domestic dogs and cats have become infected around the world.
Wild animals like red foxes which live in peri-urban areas are a possible new route of spread to farms, domestic pets and humans.
Dairy cows and goats have now become infected with H5N1 in at least 17 farms across seven US states.
What are the symptoms?
Globally, there have been 14 cases of H5N1 clade 2.3.4.4b virus in humans, and 889 H5N1 human cases overall since 2003.
Previous human cases have presented with a severe respiratory illness, but H5N1 2.3.4.4b is causing illness affecting other organs too, like the brain, eyes and liver.
For example, more recent cases have developed neurological complications including seizures, organ failure and stroke. It’s been estimated that around half of people infected with H5N1 will die.
The case in the Texan farm worker appears to be mild. This person presented with conjunctivitis, which is unusual.
Food safety
Contact with sick poultry is a key risk factor for human infection. Likewise, the farm worker in Texas was likely in close contact with the infected cattle.
The CDC advises pasteurised milk and well cooked eggs are safe. However, handling of infected meat or eggs in the process of cooking, or drinking unpasteurised milk, may pose a risk.
Although there’s no H5N1 in Australian poultry or cattle, hygienic food practices are always a good idea, as raw milk or poorly cooked meat, eggs or poultry can be contaminated with microbes such as salmonella and E Coli.
If it’s not a pandemic, why are we worried?
Scientists have feared avian influenza may cause a pandemic since about 2005. Avian flu viruses don’t easily spread in humans. But if an avian virus mutates to spread in humans, it can cause a pandemic.
One concern is if birds were to infect an animal like a pig, this acts as a genetic mixing vessel. In areas where humans and livestock exist in close proximity, for example farms, markets or even in homes with backyard poultry, the probability of bird and human flu strains mixing and mutating to cause a new pandemic strain is higher.
There are a number of potential pathways to a pandemic caused by influenza. Author provided The cows infected in Texas were tested because farmers noticed they were producing less milk. If beef cattle are similarly affected, it may not be as easily identified, and the economic loss to farmers may be a disincentive to test or report infections.
How can we prevent a pandemic?
For now there is no spread of H5N1 between humans, so there’s no immediate risk of a pandemic.
However, we now have unprecedented and persistent infection with H5N1 clade 2.3.4.4b in farms, wild animals and a wider range of wild birds than ever before, creating more chances for H5N1 to mutate and cause a pandemic.
Unlike the previous epidemiology of avian flu, where hot spots were in Asia, the new hot spots (and likely sites of emergence of a pandemic) are in the Americas, Europe or in Africa.
Pandemics grow exponentially, so early warnings for animal and human outbreaks are crucial. We can monitor infections using surveillance tools such as our EPIWATCH platform.
The earlier epidemics can be detected, the better the chance of stamping them out and rapidly developing vaccines.
Although there is a vaccine for birds, it has been largely avoided until recently because it’s only partially effective and can mask outbreaks. But it’s no longer feasible to control an outbreak by culling infected birds, so some countries like France began vaccinating poultry in 2023.
For humans, seasonal flu vaccines may provide a small amount of cross-protection, but for the best protection, vaccines need to be matched exactly to the pandemic strain, and this takes time. The 2009 flu pandemic started in May in Australia, but the vaccines were available in September, after the pandemic peak.
To reduce the risk of a pandemic, we must identify how H5N1 is spreading to so many mammalian species, what new wild bird pathways pose a risk, and monitor for early signs of outbreaks and illness in animals, birds and humans. Economic compensation for farmers is also crucial to ensure we detect all outbreaks and avoid compromising the food supply.
C Raina MacIntyre, Professor of Global Biosecurity, NHMRC L3 Research Fellow, Head, Biosecurity Program, Kirby Institute, UNSW Sydney; Ashley Quigley, Senior Research Associate, Global Biosecurity, UNSW Sydney; Haley Stone, PhD Candidate, Biosecurity Program, Kirby Institute, UNSW Sydney; Matthew Scotch, Associate Dean of Research and Professor of Biomedical Informatics, College of Health Solutions, Arizona State University, and Rebecca Dawson, Research Associate, The Kirby Institute, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
8 Signs On Your Breast You Shouldn’t Ignore
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can you name the 8 signs that may indicate breast cancer? This video discusses them, and also shows what they look like on various different skintones:
Stay abreast:
Dr Simi Adedeji bids us watch out for:
- Inverted nipple: a newly inverted nipple (pointing inward or folded) should be checked by a doctor, especially if it’s a recent change.
- Flaky rash: a flaky, itchy, or red rash around the nipple or areola could indicate an underlying issue and should not be dismissed as just a skin condition.
- Tethering: skin pulling or denting, noticeable when raising your arms, may signal a deeper problem.
- Dimpling: skin resembling an orange peel (po orang sign) with dips and accentuated pores could indicate swelling or thickening and requires medical evaluation.
- Redness or heat: unusual warmth, redness, or tenderness in the breast, particularly if not breastfeeding, should be investigated.
- Nipple discharge: any unusual fluid from the nipple (be it yellow, green, milky, clear, or blood-stained) warrants attention, especially if spontaneous or only from one side.
- Change in size: sudden changes in the size or shape of one breast should not be ignored.
- Breast lump: a firm, irregular, or persistent lump in the breast, armpit, or collarbone area should be checked promptly, even if it’s not always harmful.
The above signs may indicate cancer or something else, but none of them are things that should be ignored (even if you get just one sign).
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Hormone Therapy That Reduces Breast Cancer Risk & More
Take care!
Share This Post
Related Posts
-
Guava vs Pineapple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing guava to pineapple, we picked the guava.
Why?
Pineapple is great, but guava just beats it in most ways:
In terms of macros, guava has nearly 4x the fiber and nearly 5x the protein, for the same carbs, giving it the notably lower glycemic index. An easy win for guava in this category.
In the category of vitamins, guava has a lot more of vitamins A, B2, B3, B5, B9, C, E, K, and choline, while pineapple has marginally more vitamin B1. Another clear win for guava.
When it comes to minerals, guava has more calcium, copper, magnesium, phosphorus, potassium, selenium, and zinc, while pineapple has more iron and manganese. One more win for guava.
One big thing in pineapple’s favor is that it contains bromelain, which is an enzyme* found in pineapple (and only in pineapple), that has many very healthful properties, some of them unique to bromelain (and thus: unique to pineapple)
*actually a combination of enzymes, but most often referred to collectively in the singular. But when you do see it referred to as “they”, that’s what that means.
However cool that is, we think it unfair to weight it against guava winning in every other category, so we still say guava gets the overall win.
Of course, enjoy either or both; diversity is good!
Want to learn more?
You might like:
Let’s Get Fruity: Bromelain vs Inflammation & Much More
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Rewire Your OCD Brain – by Dr. Catherine Pittman & Dr. William Youngs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
OCD is just as misrepresented in popular media as many other disorders, and in this case, it’s typically not “being a neat freak” or needing to alphabetize things, so much as having uncontrollable obsessive intrusive thoughts, and often in response to those, unwanted compulsions. This can come from unchecked spiralling anxiety, and/or PTSD, for example.
What Drs. Pittman & Young offer is an applicable set of solutions, to literally rewire the brain (insofar as synapses can be considered neural wires). Leveraging neuroplasticity to work with us rather than against us, the authors talk us through picking apart the crossed wires, and putting them back in more helpful ways.
This is not, by the way, a book of CBT, though it does touch on that too.
Mostly, the book explains—clearly and simply and sometimes with illustrations—what is going wrong for us neurologically, and how to neurologically change that.
Bottom line: whether you have OCD or suffer from anxiety or just need help dealing with obsessive thoughts, this book can help a lot in, as the title suggests, rewiring that.
Click here to check out Rewire Your OCD Brain, and banish obsessive thoughts!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Elderberries vs Gooseberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing elderberries to gooseberries, we picked the elderberries.
Why?
These are both berries more likely found in your garden or local wood than in the supermarket, but if you have convenient access to them, they’re great options for eating!
In terms of macros, elderberry has nearly 2x the carbs and/but also nearly 2x the fiber, which in glycemic index terms, mostly cancels out (although: elderberry has the slightly lower glycemic index of the two)
In the category of vitamins, both are great but elderberries are winning with more of vitamins A, B1, B2, B3, B6, and C, while gooseberries have more vitamin B5.
When it comes to minerals, elderberries again lead with more calcium, iron, phosphorus, and potassium, while gooseberries have more magnesium.
There is an extra category today, which is “extra medicinal properties”, and elderberries have extra immune-boosting qualities, whereas gooseberries—while being as polyphenol-laden as one usually expects berries to be—do not confer the same kind of benefit in this regard.
You can check out the information about elderberry’s extra properties in the links section below; meanwhile, if you’re choosing between these berries, that’s the clear winner in every category today!
Want to learn more?
You might like to read:
- Herbs for Evidence-Based Health & Healing ← including elderberry
- Does It Come In A Pill? ← it does (but it doesn’t have to)
- Beyond Supplements: The Real Immune-Boosters! ← this article focusses on not-supplements, but does also have a supplement section
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: