AI: The Doctor That Never Tires?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
AI: The Doctor That Never Tires?
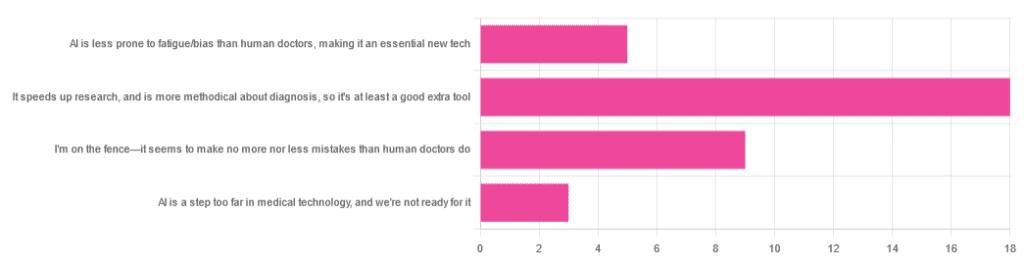
We asked you for your opinion on the use of Artificial Intelligence (AI) in healthcare, and got the above-depicted, below-described set of results:
- A little over half of respondents to the poll voted for “It speeds up research, and is more methodical about diagnosis, so it’s at least a good extra tool”
- A quarter of respondents voted for “I’m on the fence—it seems to make no more nor less mistakes than human doctors do”
- A little under a fifth of respondents voted for “AI is less prone to fatigue/bias than human doctors, making it an essential new tech”
- Three respondents voted for “AI is a step too far in medical technology, and we’re not ready for it”
Writer’s note: I’m a professional writer (you’d never have guessed, right?) and, apparently, I really did write “no more nor less mistakes”, despite the correct grammar being “no more nor fewer mistakes”. Now, I know this, and in fact, people getting less/fewer wrong is a pet hate of mine. Nevertheless, I erred.
Yet, now that I’m writing this out in my usual software, and not directly into the poll-generation software, my (AI!) grammar/style-checker is highlighting the error for me.
Now, an AI could not do my job. ChatGPT would try, and fail miserably. But can technology help me do mine better? Absolutely!
And still, I dismiss a lot of the AI’s suggestions, because I know my field and can make informed choices. I don’t follow it blindly, and I think that’s key.
AI is less prone to fatigue/bias than human doctors, making it an essential new tech: True or False?
True—with one caveat.
First, a quick anecdote from a subscriber who selected this option in the poll:
❝As long as it receives the same data inputs as my doctor (ie my entire medical history), I can see it providing a much more personalised service than my human doctor who is always forgetting what I have told him. I’m also concerned that my doctor may be depressed – not an ailment that ought to affect AI! I recently asked my newly qualified doctor goddaughter whether she would prefer to be treated by a human or AI doctor. No contest, she said – she’d go with AI. Her argument was that human doctors leap to conclusions, rather than properly weighing all the evidence – meaning AI, as long as it receives the same inputs, will be much more reliable❞
Now, an anecdote is not data, so what does the science say?
Well… It says the same:
❝Of 6695 responding physicians in active practice, 6586 provided information on the areas of interest: 3574 (54.3%) reported symptoms of burnout, 2163 (32.8%) reported excessive fatigue, and 427 (6.5%) reported recent suicidal ideation, with 255 of 6563 (3.9%) reporting a poor or failing patient safety grade in their primary work area and 691 of 6586 (10.5%) reporting a major medical error in the prior 3 months. Physicians reporting errors were more likely to have symptoms of burnout (77.6% vs 51.5%; P<.001), fatigue (46.6% vs 31.2%; P<.001), and recent suicidal ideation (12.7% vs 5.8%; P<.001).❞
See the damning report for yourself: Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors
AI, of course, does not suffer from burnout, fatigue, or suicidal ideation.
So, what was the caveat?
The caveat is about bias. Humans are biased, and that goes for medical practitioners just the same. AI’s machine learning is based on source data, and the source data comes from humans, who are biased.
See: Bias and Discrimination in AI: A Cross-Disciplinary Perspective
So, AI can perpetuate human biases and doesn’t have a special extra strength in this regard.
The lack of burnout, fatigue, and suicidal ideation, however, make a big difference.
AI speeds up research, and is more methodical about diagnosis: True or False?
True! AI is getting more and more efficient at this, and as has been pointed out, doesn’t make errors due to fatigue, and often comes to accurate conclusions near-instantaneously. To give just one example:
❝Deep learning algorithms achieved better diagnostic performance than a panel of 11 pathologists participating in a simulation exercise designed to mimic routine pathology workflow; algorithm performance was comparable with an expert pathologist interpreting whole-slide images without time constraints. The area under the curve was 0.994 (best algorithm) vs 0.884 (best pathologist).❞
About that “getting more and more efficient at this”; it’s in the nature of machine learning that every new piece of data improves the neural net being used. So long as it is getting fed new data, which it can process at rate far exceeding humans’ abilities, it will always be constantly improving.
AI makes no more nor less fewer mistakes than humans do: True or False?
False! AI makes fewer, now. This study is from 2021, and it’s only improved since then:
❝Professionals only came to the same conclusions [as each other] approximately 75 per cent of the time. More importantly, machine learning produced fewer decision-making errors than did all the professionals❞
See: AI can make better clinical decisions than humans: study
All that said, we’re not quite at Star Trek levels of “AI can do a human’s job entirely” just yet:
BMJ | Artificial intelligence versus clinicians: pros and cons
To summarize: medical AI is a powerful tool that:
- Makes healthcare more accessible
- Speeds up diagnosis
- Reduces human error
…and yet, for now at least, still requires human oversights, checks and balances.
Essentially: it’s not really about humans vs machines at all. It’s about humans and machines giving each other information, and catching any mistakes made by the other. That way, humans can make more informed decisions, and still keep a “hand on the wheel”.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Falling: Is It Due To Age Or Health Issues?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝What are the signs that a senior is falling due to health issues rather than just aging?❞
Superficial answer: having an ear infection can result in a loss of balance, and is not particularly tied to age as a risk factor
More useful answer: first, let’s consider these two true statements:
- The risks of falling (both the probability and the severity of consequences) increase with age
- Health issues (in general) tend to increase with age
With this in mind, it’s difficult to disconnect the two, as neither exist in a vacuum, and each is strongly associated with the other.
So the question is easier to answer by first flipping it, to ask:
❝What are the health issues that typically increase with age, that increase the chances of falling?❞
A non-exhaustive list includes:
- Loss of strength due to sarcopenia (reduced muscle mass)
- Loss of mobility due to increased stiffness (many causes, most of which worsen with age)
- Loss of risk-awareness due to diminished senses (for example, not seeing an obstacle until too late)
- Loss of risk-awareness due to reduced mental focus (cognitive decline producing absent-mindedness)
Note that in the last example there, and to a lesser extent the third one, reminds us that falls also often do not happen in a vacuum. There is (despite how it may sometimes feel!) no actual change in our physical relationship with gravity as we get older; most falls are about falling over things, even if it’s just one’s own feet:
The 4 Bad Habits That Cause The Most Falls While Walking
Disclaimer: sometimes a person may just fall down for no external reason. An example of why this may happen is if a person’s joint (for example an ankle or a knee) has a particular weakness that means it’ll occasionally just buckle and collapse under one’s own weight. This doesn’t even have to be a lot of weight! The weakness could be due to an old injury, or Ehlers-Danlos Syndrome (with its characteristic joint hypermobility symptoms), or something else entirely.
Now, notice how:
- all of these things can happen at any age
- all of these things are more likely to happen the older we get
- none of these things have to happen at any age
That last one’s important to remember! Aging is often viewed as an implacable Behemoth, but the truth is that it is many-faceted and every single one of those facets can be countered, to a greater or lesser degree.
Think of a room full of 80-year-olds, and now imagine that…
- One has the hearing of a 20-year-old
- One has the eyesight of a 20-year-old
- One has the sharp quick mind of a 20-year-old
- One has the cardiovascular fitness of a 20-year-old
…etc. Now, none of those things in isolation is unthinkable, so remember, there is no magic law of the universe saying we can’t have each of them:
Age & Aging: What Can (And Can’t) We Do About It?
Which means: that goes for the things that increase the risk of falling, too. In other words, we can combat sarcopenia with protein and resistance training, maintain our mobility, look after our sensory organs as best we can, nourish our brain and keep it sharp, etc etc etc:
Train For The Event Of Your Life! (Mobility As A Long-Term “Athletic” Goal For Personal Safety)
Which doesn’t mean: that we will necessarily succeed in all areas. Your writer here, broadly in excellent health, and whose lower body is still a veritable powerhouse in athletic terms, has a right ankle and left knee that will sometimes just buckle (yay, the aforementioned hypermobility).
So, it becomes a priority to pre-empt the consequences of that, for example:
- being able to fall with minimal impact (this is a matter of knowing how, and can be learned from “soft” martial arts such as aikido), and
- ensuring the skeleton can take a knock if necessary (keeping a good balance of vitamins, minerals, protein, etc; keeping an eye on bone density).
See also:
Fall Special ← appropriate for the coming season, but it’s about avoiding falling, and reducing the damage of falling if one does fall, including some exercises to try at home.
Take care!
Share This Post
-
Why Some Friendships Last And Others Don’t
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Friendships matter a lot, playing a significant role in our wellbeing, physical as well as mental. They bring additional meaning to our lives, help us cope with setbacks, and hopefully will be at our side through the highs and lows of life. And yet, for something that’s in principle good for everyone involved, there can be problems:
Friend to the end?
Firstly, some people find it harder to make (and then further deepen) friendships with others, which can be for a whole host of reasons.
Approaching new people can feel intimidating, but it’s a common struggle. Research shows that people often underestimate how much others enjoy their company, a phenomenon known as the “liking gap.” By reminding ourselves that others are likely to appreciate our presence and expecting to be well-received (the “acceptance prophecy”), we can approach social interactions with greater confidence.
As relationships grow, they often deepen through companionship and closeness:
- Companionship arises from shared hobbies, interests, or values, and it builds rapport.
- Closeness involves sharing thoughts, feelings, and experiences, which can build intimacy together.
An important key to these is consistency, which—whether through regular chats, honoring plans, or showing support—helps strengthen bonds, even in long-distance friendships (something often considered a barrier to closeness).
Even the strongest friendships can face challenges, of course. Conflicts may arise from a lack of support during difficult moments, or worse, betrayal. Or it could all be a misunderstanding. These situations are best addressed through honest, non-judgmental conversations. Avoiding defensiveness or accusations, and instead focusing on sharing feelings and understanding the other person’s perspective, can turn these tough discussions into opportunities for growth and stronger connections.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Beat Loneliness & Isolation
Take care!
Share This Post
-
Nori vs Wakame – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing nori to wakame, we picked the nori.
Why?
It was close, and both of these seaweed options are great!
In terms of macros, nori has more protein while wakame has more carbs; they’re about equal on fiber. While the difference in protein and carbs isn’t big, out of the two we’ll prioritize protein, and thus say nori gets a notional win here—but as it’s so close, one could just as easily call it a tie.
In the category of vitamins both are very rich in many minerals, but nori has more of vitamins A, B1, B2, B6, B12*, and C, while wakame has more of vitamins B5, B9, K, and choline. Thus, a 6:4 victory for nori.
*Yes, nori is one of those rare vegan foods that naturally contain vitamin B12; it’s because of the composition of the algae that this seaweed is made of, which includes some beneficial B12-making bacteria. Meanwhile, wakame is “just” a kelp, so it doesn’t have B12.
When it comes to minerals, nori has more potassium and zinc, while wakame has more calcium and magnesium. They’re equal on other minerals, except: it’s worth noting that wakame is moderately high in sodium, while nori has very little sodium. So, either a tie-breaking win for nori, or just a tie.
Adding up the sections gives nori the overall win; it’s only the margin of the win that’s reasonably debatable. Still, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
- A Deeper Dive Into Seaweed
- Spirulina vs Nori – Which is Healthier? ← guess which won!
- 21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!) ← nori and wakame both feature (very favorably) in this case study
Enjoy!
Share This Post
Related Posts
-
What happens when I stop taking a drug like Ozempic or Mounjaro?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hundreds of thousands of people worldwide are taking drugs like Ozempic to lose weight. But what do we actually know about them? This month, The Conversation’s experts explore their rise, impact and potential consequences.
Drugs like Ozempic are very effective at helping most people who take them lose weight. Semaglutide (sold as Wegovy and Ozempic) and tirzepatide (sold as Zepbound and Mounjaro) are the most well known in the class of drugs that mimic hormones to reduce feelings of hunger.
But does weight come back when you stop using it?
The short answer is yes. Stopping tirzepatide and semaglutide will result in weight regain in most people.
So are these medications simply another (expensive) form of yo-yo dieting? Let’s look at what the evidence shows so far.
It’s a long-term treatment, not a short course
If you have a bacterial infection, antibiotics will help your body fight off the germs causing your illness. You take the full course of medication, and the infection is gone.
For obesity, taking tirzepatide or semaglutide can help your body get rid of fat. However it doesn’t fix the reasons you gained weight in the first place because obesity is a chronic, complex condition. When you stop the medications, the weight returns.
Perhaps a more useful comparison is with high blood pressure, also known as hypertension. Treatment for hypertension is lifelong. It’s the same with obesity. Medications work, but only while you are taking them. (Though obesity is more complicated than hypertension, as many different factors both cause and perpetuate it.)
Obesity drugs only work while you’re taking them. KK Stock/Shutterstock Therefore, several concurrent approaches are needed; taking medication can be an important part of effective management but on its own, it’s often insufficient. And in an unwanted knock-on effect, stopping medication can undermine other strategies to lose weight, like eating less.
Why do people stop?
Research trials show anywhere from 6% to 13.5% of participants stop taking these drugs, primarily because of side effects.
But these studies don’t account for those forced to stop because of cost or widespread supply issues. We don’t know how many people have needed to stop this medication over the past few years for these reasons.
Understanding what stopping does to the body is therefore important.
So what happens when you stop?
When you stop using tirzepatide or semaglutide, it takes several days (or even a couple of weeks) to move out of your system. As it does, a number of things happen:
- you start feeling hungry again, because both your brain and your gut no longer have the medication working to make you feel full
When you stop taking it, you feel hungry again. Stock-Asso/Shutterstock - blood sugars increase, because the medication is no longer acting on the pancreas to help control this. If you have diabetes as well as obesity you may need to take other medications to keep these in an acceptable range. Whether you have diabetes or not, you may need to eat foods with a low glycemic index to stabilise your blood sugars
- over the longer term, most people experience a return to their previous blood pressure and cholesterol levels, as the weight comes back
- weight regain will mostly be in the form of fat, because it will be gained faster than skeletal muscle.
While you were on the medication, you will have lost proportionally less skeletal muscle than fat, muscle loss is inevitable when you lose weight, no matter whether you use medications or not. The problem is, when you stop the medication, your body preferentially puts on fat.
Is stopping and starting the medications a problem?
People whose weight fluctuates with tirzepatide or semaglutide may experience some of the downsides of yo-yo dieting.
When you keep going on and off diets, it’s like a rollercoaster ride for your body. Each time you regain weight, your body has to deal with spikes in blood pressure, heart rate, and how your body handles sugars and fats. This can stress your heart and overall cardiovascular system, as it has to respond to greater fluctuations than usual.
Interestingly, the risk to the body from weight fluctuations is greater for people who are not obese. This should be a caution to those who are not obese but still using tirzepatide or semaglutide to try to lose unwanted weight.
How can you avoid gaining weight when you stop?
Fear of regaining weight when stopping these medications is valid, and needs to be addressed directly. As obesity has many causes and perpetuating factors, many evidence-based approaches are needed to reduce weight regain. This might include:
- getting quality sleep
- exercising in a way that builds and maintains muscle. While on the medication, you will likely have lost muscle as well as fat, although this is not inevitable, especially if you exercise regularly while taking it
Prioritise building and maintaining muscle. EvMedvedeva/Shutterstock - addressing emotional and cultural aspects of life that contribute to over-eating and/or eating unhealthy foods, and how you view your body. Stigma and shame around body shape and size is not cured by taking this medication. Even if you have a healthy relationship with food, we live in a culture that is fat-phobic and discriminates against people in larger bodies
- eating in a healthy way, hopefully continuing with habits that were formed while on the medication. Eating meals that have high nutrition and fibre, for example, and lower overall portion sizes.
Many people will stop taking tirzepatide or semaglutide at some point, given it is expensive and in short supply. When you do, it is important to understand what will happen and what you can do to help avoid the consequences. Regular reviews with your GP are also important.
Read the other articles in The Conversation’s Ozempic series here.
Natasha Yates, General Practitioner, PhD Candidate, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why are people on TikTok talking about going for a ‘fart walk’? A gastroenterologist weighs in
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Fart walks” have become a cultural phenomenon, after a woman named Mairlyn Smith posted online a now-viral video about how she and her husband go on walks about 60 minutes after dinner and release their gas.
Smith, known on TikTok as @mairlynthequeenoffibre and @mairlynsmith on Instagram, has since appeared on myriad TV and press interviews extolling the benefits of a fart walk. Countless TikTok and Instagram users and have now shared their own experiences of feeling better after taking up the #fartwalk habit.
So what’s the evidence behind the fart walk? And what’s the best way to do it?
CandyBox Images/Shutterstock Exercise can help get the gas out
We know exercise can help relieve bloating by getting gas moving and out of our bodies.
Researchers from Barcelona, Spain in 2006 asked eight patients complaining of bloating, seven of whom had irritable bowel syndrome, to avoid “gassy” foods such as beans for two days and to fast for eight hours before their study.
Each patient was asked to sit in an armchair, in order to avoid any effects of body position on the movement of gas. Gas was pumped directly into their small bowel via a thin plastic tube that went down their mouth, and the gas expelled from the body was collected into a bag via a tube placed in the rectum. This way, the researchers could determine how much gas was retained in the gut.
The patients were then asked to pedal on a modified exercise bike while remaining seated in their armchairs.
The researchers found that much less gas was retained in the patients’ gut when they exercised. They determined exercise probably helped the movement and release of intestinal gas.
Walking may have another bonus; it may trigger a nerve reflex that helps propel foods and gas contents through the gut.
Walking can also increase internal abdominal pressure as you use your abdominal muscles to stay upright and balance as you walk. This pressure on the colon helps to push intestinal gas out.
Proper fart walk technique
One study from Iran studied the effects of walking in 94 individuals with bloating.
They asked participants to carry out ten to 15 minutes of slow walking (about 1,000 steps) after eating lunch and dinner. They filled out gut symptom questionnaires before starting the program and again at the end of the four week program.
The researchers found walking after meals resulted in improvements to gut symptoms such as belching, farting, bloating and abdominal discomfort.
Now for the crucial part: in the Iranian study, there was a particular way in which participants were advised to walk. They were asked to clasp hands together behind their back and to flex their neck forward.
The clasped hands posture leads to more internal abdominal pressure and therefore more gentle squeezing out of gas from the colon. The flexed neck posture decreases the swallowing of air during walking.
This therefore is the proper fart walk technique, based on science.
Could walking with your hands behind your back yield better or more farts? candy candy/Shutterstock What about constipation?
A fart walk can help with constipation.
One study involved middle aged inactive patients with chronic constipation, who did a 12 week program of brisk walking at least 30 minutes a day – combined with 11 minutes of strength and flexibility exercises.
This program, the researchers found, improved constipation symptoms through reduced straining, less hard stools and more complete evacuation.
It also appears that the more you walk the better the benefits for gut symptoms.
In patients with irritable bowel syndrome, one study increasing the daily step count to 9,500 steps from 4,000 steps led to a 50% reduction in the severity of their symptoms.
And just 30 minutes of a fart walk has been shown to improve blood sugar levels after eating.
Walking after eating can help keep your blood sugar levels under control. IndianFaces/Shutterstock What if I can’t get outside the house?
If getting outside the house after dinner is impossible, could you try walking slowly on a treadmill or around the house for 1,000 steps?
If not, perhaps you could borrow an idea from the Barcelona research: sit back in an armchair and pedal using a modified exercise bike. Any type of exercise is better than none.
Whatever you do, don’t be a couch potato! Research has found more leisure screen time is linked to a greater risk of developing gut diseases.
We also know physical inactivity during leisure time and eating irregular meals are linked to a higher risk of abdominal pain, bloating and altered bowel motions.
Try the fart walk today
It may not be for everyone but this simple physical activity does have good evidence behind it. A fart walk can improve common symptoms such as bloating, abdominal discomfort and constipation.
It can even help lower blood sugar levels after eating.
Will you be trying a fart walk today?
Vincent Ho, Associate Professor and clinical academic gastroenterologist, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Best Mobility Exercises For Each Joint
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Stiff joints and tight muscles limit movement, performance, and daily activities. They also increase the risk of injury, and increase recovery time if the injury happens. So, it’s pretty important to take care of that!
Here’s how
Key to joint health involves understanding mobility, flexibility, and stability:
- Mobility: active joint movement through a range of motion.
- Flexibility: muscle lengthening passively through a range of motion.
- Stability: body’s ability to return to position after disturbance.
Different body parts have different needs when it comes to prioritizing mobility, flexibility, and stability exercises. So, with that in mind, here’s what to do for your…
- Wrists: flexibility and stability (e.g., wrist circles, loaded flexions/extensions).
- Elbows: Stability is key; exercises like wrist and shoulder movements benefit elbows indirectly.
- Shoulders: mobility and stability; exercises include prone arm circles, passive hangs, active prone raises, easy bridges, and stick-supported movements.
- Spine: mobility and stability; recommended exercises include cat-cow and quadruped reach.
- Hips: mobility and flexibility through deep squat hip rotations; beginners can use hands for support.
- Knees: stability; exercises include elevated pistols, Bulgarian split squats, lunges, and single-leg balancing.
- Ankles: flexibility and stability; exercises include lunges, prying goblet squats, and deep squats with support if necessary.
For more on all of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Building & Maintaining Mobility
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: