Five Advance Warnings of Multiple Sclerosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Five Advance Warnings of Multiple Sclerosis
First things first, a quick check-in with regard to how much you know about multiple sclerosis (MS):
- Do you know what causes it?
- Do you know how it happens?
- Do you know how it can be fixed?
If your answer to the above questions is “no”, then take solace in the fact that modern science doesn’t know either.
What we do know is that it’s an autoimmune condition, and that it results in the degradation of myelin, the “insulator” of nerves, in the central nervous system.
- How exactly this is brought about remains unclear, though there are several leading hypotheses including autoimmune attack of myelin itself, or disruption to the production of myelin.
- Treatments look to reduce/mitigate inflammation, and/or treat other symptoms (which are many and various) on an as-needed basis.
If you’re wondering about the prognosis after diagnosis, the scientific consensus on that is also “we don’t know”:
Read: Personalized medicine in multiple sclerosis: hope or reality?
this paper, like every other one we considered putting in that spot, concludes with basically begging for research to be done to identify biomarkers in a useful fashion that could help classify many distinct forms of MS, rather than the current “you have MS, but who knows what that will mean for you personally because it’s so varied” approach.
The Five Advance Warning Signs
Something we do know! First, we’ll quote directly the researchers’ conclusion:
❝We identified 5 health conditions associated with subsequent MS diagnosis, which may be considered not only prodromal but also early-stage symptoms.
However, these health conditions overlap with prodrome of two other autoimmune diseases, hence they lack specificity to MS.❞
So, these things are a warning, five alarm bells, but not necessarily diagnostic criteria.
Without further ado, the five things are:
- depression
- sexual disorders
- constipation
- cystitis
- urinary tract infections
❝This association was sufficiently robust at the statistical level for us to state that these are early clinical warning signs, probably related to damage to the nervous system, in patients who will later be diagnosed with multiple sclerosis.
The overrepresentation of these symptoms persisted and even increased over the five years after diagnosis.❞
Read the paper for yourself:
Hot off the press! Published only yesterday!
Want to know more about MS?
Here’s a very comprehensive guide:
National clinical guideline for diagnosis and management of multiple sclerosis
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lime-Charred Cauliflower Popcorn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Called “popcorn” for its appearance and tasty-snackness, this one otherwise bears little relation to the usual movie theater snack, and it’s both tastier and healthier. All that said, it can be eaten on its own as a snack (even with a movie, if you so wish), or served as one part of a many-dish banquet, or (this writer’s favorite) as a delicious appetizer that also puts down a healthy bed of fiber ready for the main course to follow it.
You will need
- 1 cauliflower, cut into small (popcorn-sized) florets
- 2 tbsp extra virgin olive oil
- 1 tbsp lime pickle
- 1 tsp cumin seeds
- 1 tsp smoked paprika
- 1 tsp chili flakes
- 1 tsp black pepper, coarse ground
- ½ tsp ground turmeric
Method
(we suggest you read everything at least once before doing anything)
1) Preheat your oven as hot as it will go
2) Mix all the ingredients in a small bowl except the cauliflower, to form a marinade
3) Drizzle the marinade over the cauliflower in a larger bowl (i.e. big enough for the cauliflower), and mix well until the cauliflower is entirely, or at least almost entirely, coated. Yes, it’s not a lot of marinade but unless you picked a truly huge cauliflower, the proportions we gave will be enough, and you want the end result to be crisp, not dripping.
4) Spread the marinaded cauliflower florets out on a baking tray lined with baking paper. Put it in the oven on the middle shelf, so it doesn’t cook unevenly, but keeping the temperature as high as it goes.
5) When it is charred and crispy golden, it’s done—this should take about 20 minutes, but we’ll say ±5 minutes depending on your oven, so do check on it periodically—and time to serve (it is best enjoyed warm).
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- We must do a main feature on the merits of cruciferous vegetables! Watch this space.
- All About Olive Oils (Extra Virgin & Otherwise)
- Capsaicin For Weight Loss And Against Inflammation
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Take care!
Share This Post
-
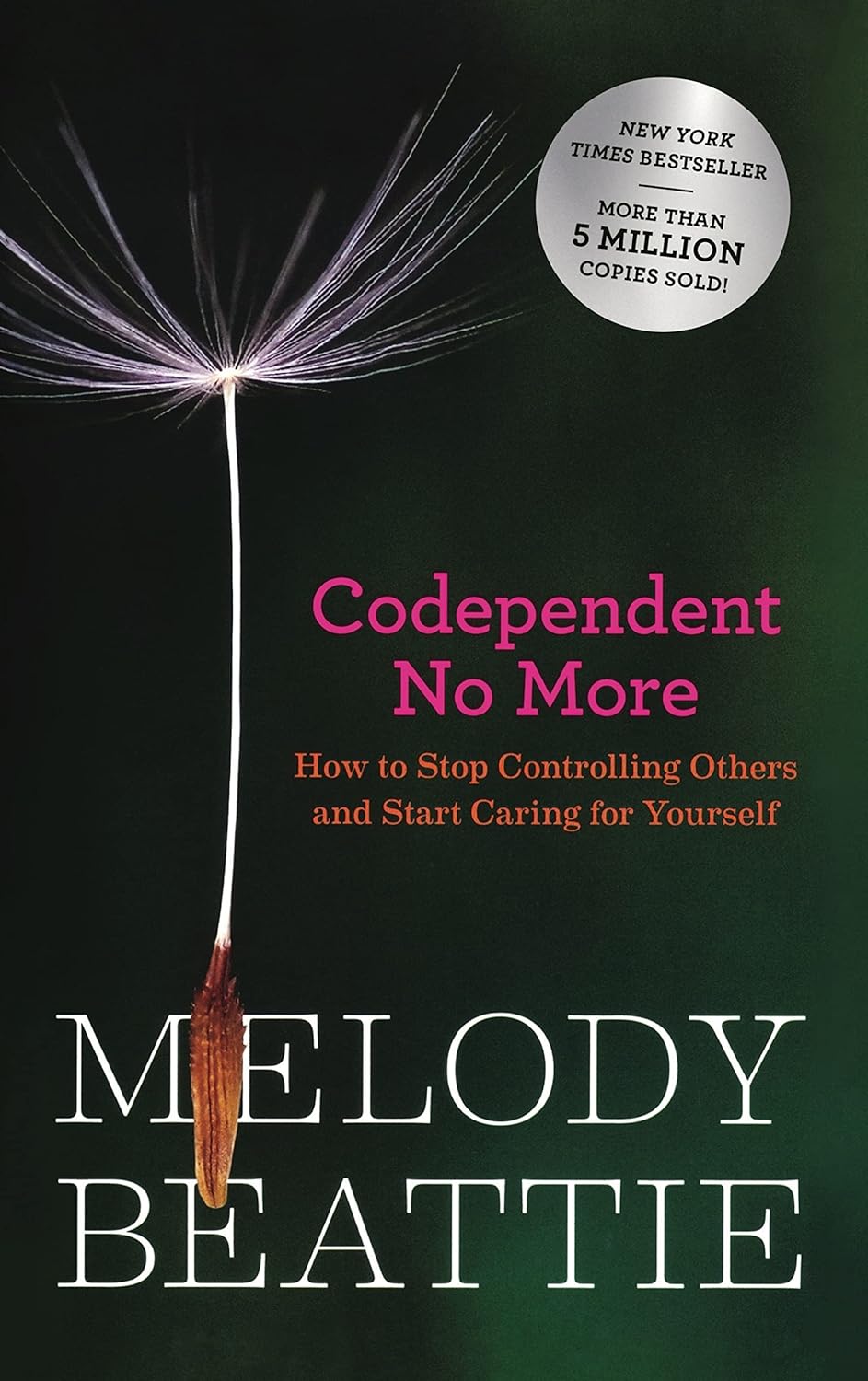
Codependent No More – by Melody Beattie
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a book review, not a book summary, but first let’s quickly cover a common misconception, because the word “codependent” gets misused a lot in popular parlance:
- What codependence isn’t: “we depend on each other and must do everything together”
- What codependence is:“person 1 has a dependency on a substance (or perhaps a behavior, such as gambling); person 2 is trying to look after person 1, and so has developed a secondary relationship with the substance/behavior. Person 2 is now said to be codependent, because it becomes all-consuming for them too, even if they’re not using the substance/behavior directly”
Funny how often it happens that the reality is more complex than the perception, isn’t it?
Melody Beattie unravels all this for us. We get a compassionate and insightful look at how we can look after ourselves, while looking after another. Perhaps most importantly: how and where to draw a line of what we can and cannot do/change for them.
Because when we love someone, of course we want to fight their battles with them, if not for them. But if we want to be their rock of strength, we can’t get lost in it too, and of course that hurts.
Beatty takes us through these ideas and more, for example:
- How to examine our own feelings even when it’s scary
- How to practice self-love and regain self-worth, while still caring for them
- How to stop being reactionary, step back, and act with purpose
If the book has any weak point, it’s that it repeatedly recommends 12-step programs, when in reality that’s just one option. But for those who wish to take another approach, this book does not require involvement in a 12-step program, so it’s not a barrier to usefulness.
Click here to check out Codependent No More and take care of yourself, too
Share This Post
-
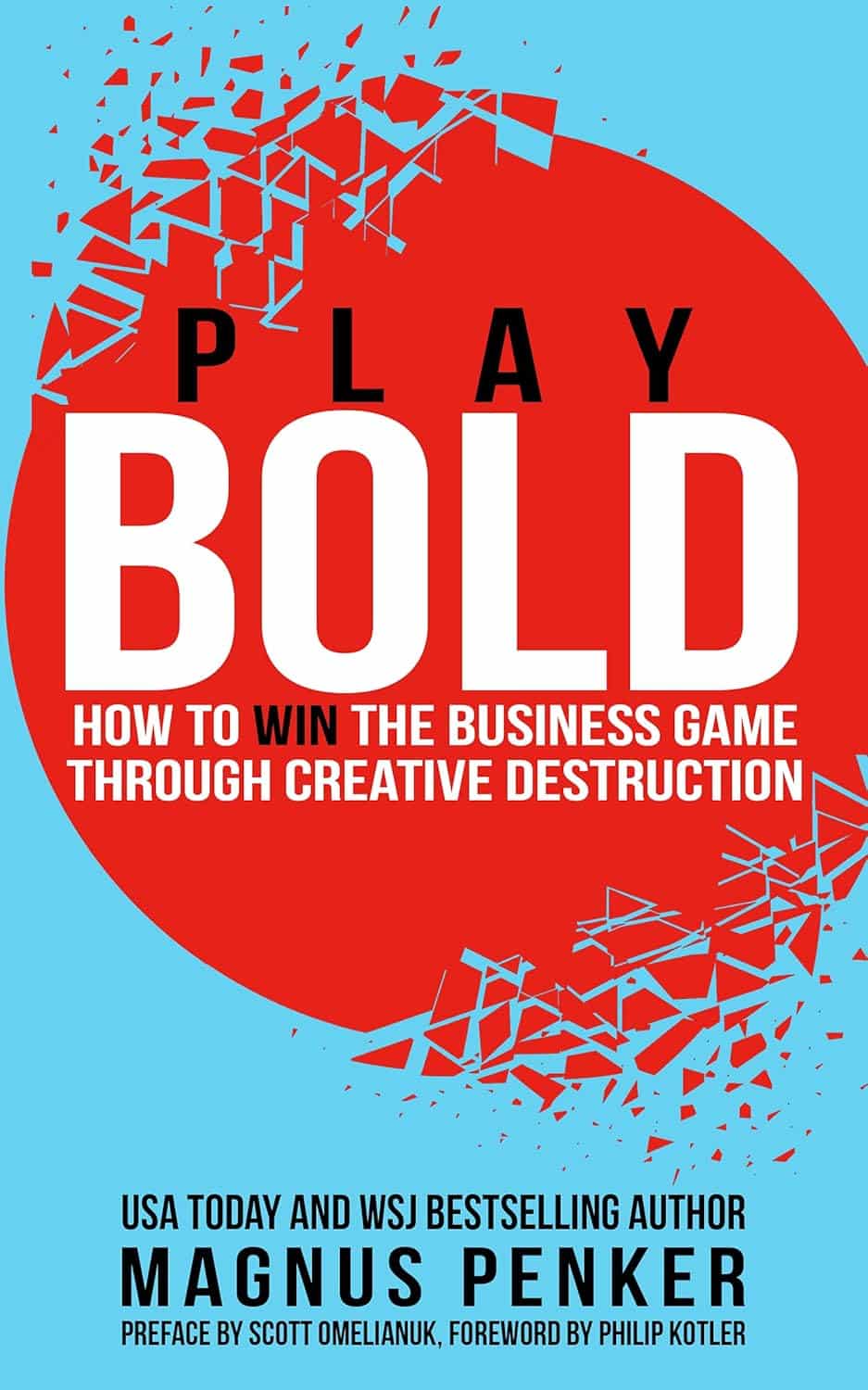
Play Bold – by Magnus Penker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is very different to what you might expect, from the title.
We often see: “play bold, believe in yourself, the universe rewards action” etc… Instead, this one is more: “play bold, pay attention to the data, use these metrics, learn from what these businesses did and what their results were”, etc.
We often see: “here’s an anecdote about a historical figure and/or celebrity who made a tremendous bluff and it worked out well so you should too” etc… Instead, this one is more: “see how what we think of as safety is actually anything but! And how by embracing change quickly (or ideally: proactively), we can stay ahead of disaster that may otherwise hit us”.
Penker’s background is also relevant here. He has decades of experience, having “launched 10 start-ups and acquired, turned around, and sold over 30 SMEs all over Europe”. Importantly, he’s also “still in the game”… So, unlike many authors whose last experience in the industry was in the 1970s and who wonder why people aren’t reaping the same rewards today!
Penker is the therefore opposite of many who advocate to “play bold” but simply mean “fail fast, fail often”… While quietly relying on their family’s capital and privilege to leave a trail of financial destruction behind them, and simultaneously gloating about their imagined business expertise.
In short: boldness does not equate to foolhardiness, and foolhardiness does not equate to boldness.
As for telling the difference? Well, for that we recommend reading the book—It’s a highly instructive one.
Take The First Bold Step Of Checking Out This Book On Amazon!
Share This Post
Related Posts
-
Hearty Healthy Ukrainian Borscht
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the West, borscht is often thought of as Russian, but it is Ukrainian in origin and popular throughout much of Eastern Europe, with many local variations. Today’s borscht is a vegetarian (and vegan, depending on your choice of cooking fat) borscht from Kyiv, and it’s especially good for the gut, heart, and blood sugars.
You will need
- 1 quart vegetable stock; ideally you made this yourself from vegetable offcuts you kept in the freezer, but failing that, your supermarket should have low-sodium stock cubes
- 4 large beets, peeled and cut into matchsticks
- 1 can white beans (cannellini beans are ideal), drained and rinsed
- 1 cup sauerkraut
- 1 large onion, finely chopped
- 1 green bell pepper, roughly chopped
- 1 large russet potato, peeled and cut into large chunks
- 3 small carrots, tops removed and cut into large chunks
- 1 tbsp tomato paste
- ½ bulb garlic, finely chopped
- 2 tsp black pepper, coarse ground
- 1 bunch fresh dill, chopped. If you cannot get fresh, substitute with parsley (1 bunch fresh, chopped, or 1 tbsp dried). Do not use dried dill; it won’t work.
- A little fat for cooking; this one’s a tricky and personal decision. Butter is traditional, but would make this recipe impossible to cook without going over the recommended limit for saturated fat. Avocado oil is healthy, relatively neutral in taste, and has a high smoke point, though that latter shouldn’t be necessary here if you are attentive with the stirring. Extra virgin olive oil is also a healthy choice, but not as neutral in flavor and does have a lower smoke point. Coconut oil has arguably too strong a taste and a low smoke point. Seed oils are very heart-unhealthy. All in all, avocado oil is a respectable choice from all angles except tradition.
- On standby: a little vinegar (your preference what kind)
Salt is conspicuous by its absence, but there should be enough already from the other ingredients, especially the sauerkraut.
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a large sauté pan (cast iron is perfect if you have it), add the onion and pepper, and stir until the onion is becoming soft.
2) Add the carrots and beets and stir until they are becoming soft. If you need to add a little more oil, that’s fine.
3) Add the tomato paste, and stir in well.
4) Add a little (about ½ cup) of the vegetable stock and stir in well until you get a consistent texture with the tomato paste.
5) Add the sauerkraut and the rest of the broth, and cook for about 20 minutes.
6) Add the potatoes and cook for another 10 minutes.
7) Add the beans and cook for another 5 minutes.
8) Add the garlic, black pepper, and herbs. Check that everything is cooked (poke a chunk of potato with a fork) and that the seasoning is to your liking. The taste should be moderately sour from the sauerkraut; if it is sweet, you can stir in a little vinegar now to correct that.
9) Serve! Ukrainian borscht is most often served hot (unlike Lithuanian borscht, which is almost always served cold), but if the weather’s warm, it can certainly be enjoyed cold too:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Eat More (Of This) For Lower Blood Pressure
- No, Beetroot Isn’t Vegetable Viagra. But Here’s What It Can Do
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Break the Cycle – by Dr. Mariel Buqué
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Intergenerational trauma comes in two main varieties: epigenetic, and behavioral.
This book covers both. There’s a lot more we can do about the behavioral side than the epigenetic, but that’s not to say that Dr. Buqué doesn’t have useful input in the latter kind too.
If you’ve read other books on epigenetic trauma, then there’s nothing new here—though the refresher is always welcome.
On the behavioral side, Dr. Buqué gives a strong focus on practical techniques, such as specific methods of journaling to isolate trauma-generated beliefs and resultant behaviors, with a view to creating one’s own trauma-informed care, cutting through the cycle, and stopping it there.
Which, of course, will not only be better for you, but also for anyone who will be affected by how you are (e.g. now/soon, hopefully better).
As a bonus, if you see the mistakes your parents made and are pretty sure you didn’t pass them on, this book can help you troubleshoot for things you missed, and also to improve your relationship with your own childhood.
Bottom line: if you lament how things were, and do wish/hope to do better in terms of mental health for yourself now and generations down the line, this book is a great starting point.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
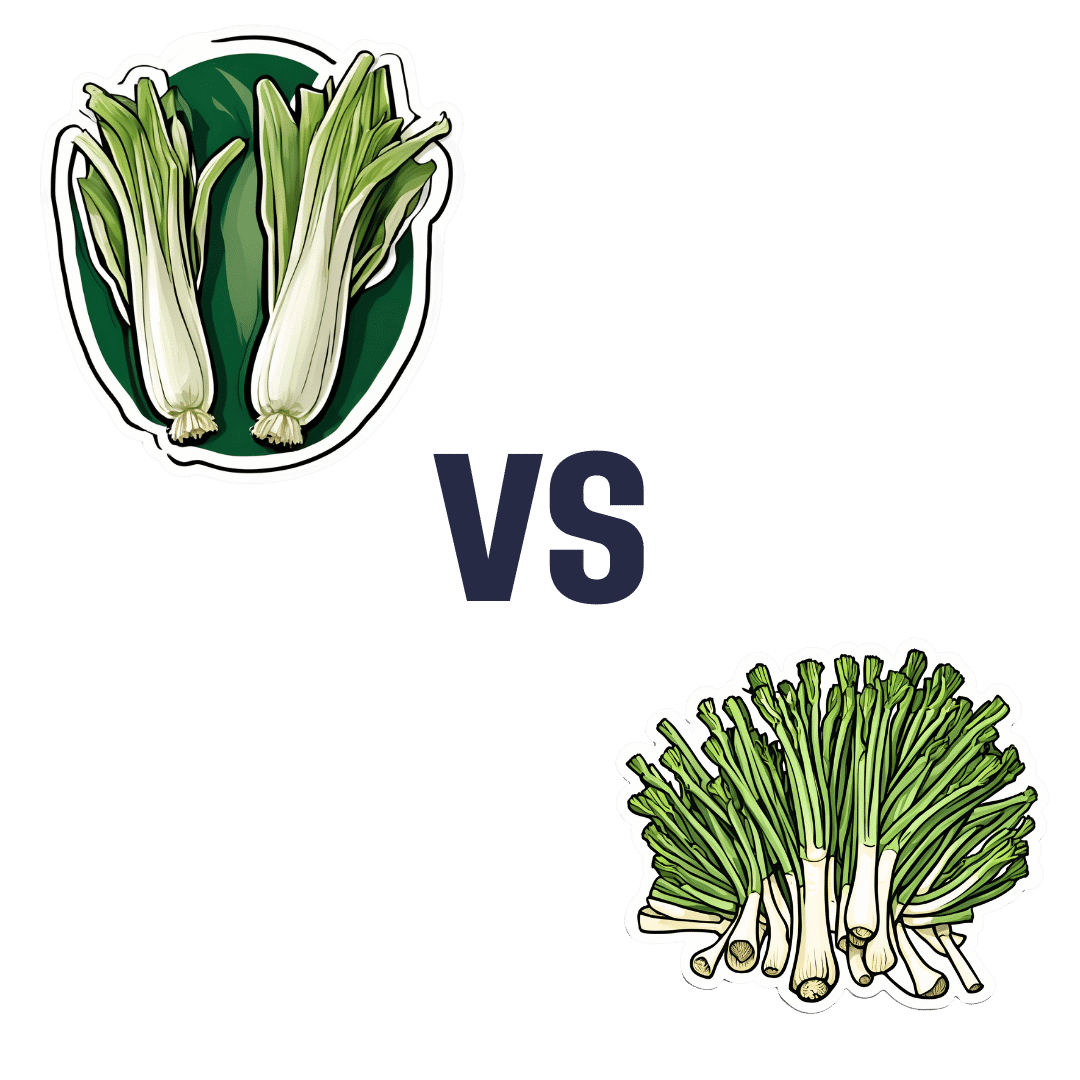
Leek vs Scallions – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing leek to scallions, we picked the leek.
Why?
In terms of macros, scallions might have a point: scallions have the lower glycemic index, thanks to leek having more carbs for the same amount of fiber. That said, leek already has a low glycemic index, so this is not a big deal.
When it comes to vitamins, leek has more of vitamins B1, B2, B3, B5, B6, B9, E, and choline, while scallions have more of vitamins A, C, and K. Noteworthily, a cup of chopped leek already provides the daily dose of vitamins A and K, and the difference in levels of vitamin C is minimal. All in all, an easy 8:3 win for leeks here, even without taking that into account.
In the category of minerals, leek has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and selenium, while scallions have a little more zinc.
Both of these allium-family plants (i.e., related to garlic) have an abundance of polyphenols, especially kaempferol.
Of course, enjoy whatever goes best with your meal, but if you’re looking for nutritional density, then leek is where it’s at.
Want to learn more?
You might like to read:
The Many Health Benefits Of Garlic
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: