Is ADHD Being Over-Diagnosed For Cash?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is ADHD Being Systematically Overdiagnosed?
The BBC’s investigative “Panorama” program all so recently did a documentary in which one of their journalists—who does not have ADHD—went to three private clinics and got an ADHD diagnosis from each of them:
- The BBC documentary: Private ADHD Clinics Exposed (28 mins)
- Their “5 Minutes” version: ADHD Undercover: How I Was Misdiagnosed (6 mins)
So… Is it really a case of show up, pay up, and get a shiny new diagnosis?
The BBC Panorama producers cherry-picked 3 private providers, and during those clinical assessments, their journalist provided answers that would certainly lead to a diagnosis.
This was contrasted against a three-hour assessment with an NHS psychiatrist—something that rarely happens in the NHS. Which prompts the question…
How did he walk into a 3-hour psychiatrist assessment, when most people have to wait in long waiting lists for a much more cursory appointment first with assorted gatekeepers, before going on another long waiting list, for an also-much-shorter appointment with a psychiatrist?
That would be because the NHS psychiatrist was given advance notification that this was part of an investigation and would be filmed (the private clinics were not gifted the same transparency)
So, maybe just a tad unequal treatment!
In case you’re wondering, here’s what that very NHS psychiatrist had to say on the topic:
Is it really too easy to be diagnosed with ADHD?
(we’ll give you a hint—remember Betteridge’s Law!)
❝Since the documentary aired, I have heard from people concerned that GPs could now be more likely to question legitimate diagnoses.
But as an NHS psychiatrist it is clear to me that the root of this issue is not overdiagnosis.
Instead, we are facing the combined challenges of remedying decades of underdiagnosis and NHS services that were set up when there was little awareness of ADHD.❞
~ Dr. Mike Smith, Psychiatrist
The ADHD foundation, meanwhile, has issued its own response, saying:
❝We are disappointed that BBC Panorama has opted to broadcast a poorly researched, sensationalist piece of television journalism.❞
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pomegranate vs Cherries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pomegranate to cherries, we picked the pomegranate.
Why?
In terms of macros, pomegranate is slightly higher in carbs, and/but 4x higher in fiber. That’s already a good start for pomegranates. Lest we be accused of cherry-picking, though, we’ll mention that pomegranate is also slightly higher in protein and fat, for what it’s worth—which is not a lot. As with most fruits, the protein and fat numbers are low importance next to the carb:fiber ratio.
When it comes to vitamins, pomegranate has more of vitamins B1, B2, B5, B6, B9. E. K, and choline. On the other hand, cherries have more of vitamins A and B3. The two fruits are equal in vitamin C. This all makes for a clear win for pomegranate.
In the category of minerals, pomegranate boasts more copper, magnesium, phosphorus, potassium, selenium, and zinc. In contrast, cherries have slightly more calcium. Another win for pomegranate.
Both of these fruits have beneficial polyphenols, each with a slightly different profile, but neither pressingly better than the other.
In short: as ever with healthy foods, enjoy both—diversity is good! But if you’re going to pick on, we recommend the pomegranate.
Want to learn more?
You might like to read:
- Pomegranate Peel’s Potent Potential ← so don’t throw it away!
- Cherries’ Very Healthy Wealth Of Benefits!
Take care!
Share This Post
-
Pumpkin Seeds vs Watermelon Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pumpkin seeds to watermelon seeds, we picked the watermelon.
Why?
Starting with the macros: pumpkin seeds have a lot more carbs, while watermelon seeds have a lot more protein, despite pumpkin seeds being famous for such. They’re about equal on fiber. In terms of fats, watermelon seeds are higher in fats, and yes, these are healthy fats, mostly polyunsaturated.
When it comes to vitamins, pumpkin seeds are marginally higher in vitamins A and C, while watermelon seeds are a lot higher in vitamins B1, B2, B3, B5, B6, and B9. An easy win for watermelon seeds here.
In the category of minerals, despite being famous for zinc, pumpkin seeds are higher only in potassium, while watermelon seeds are higher in iron, magnesium, manganese, and phosphorus; the two seeds are equal on calcium, copper, and zinc. Another win for watermelon seeds.
In short, enjoy both, but watermelon has more to offer. Of course, if buying just the seeds and not the whole fruit, it’s generally easier to find pumpkin seeds than watermelon seeds, so do bear in mind that pumpkin seeds’ second place isn’t that bad here—it’s just a case of a very nutritious food looking bad by standing next to an even better one.
Want to learn more?
You might like to read:
Seed Saving Secrets – by Alice Mirren
Take care!
Share This Post
-
Why it’s a bad idea to mix alcohol with some medications
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anyone who has drunk alcohol will be familiar with how easily it can lower your social inhibitions and let you do things you wouldn’t normally do.
But you may not be aware that mixing certain medicines with alcohol can increase the effects and put you at risk.
When you mix alcohol with medicines, whether prescription or over-the-counter, the medicines can increase the effects of the alcohol or the alcohol can increase the side-effects of the drug. Sometimes it can also result in all new side-effects.
How alcohol and medicines interact
The chemicals in your brain maintain a delicate balance between excitation and inhibition. Too much excitation can lead to convulsions. Too much inhibition and you will experience effects like sedation and depression.
Alcohol works by increasing the amount of inhibition in the brain. You might recognise this as a sense of relaxation and a lowering of social inhibitions when you’ve had a couple of alcoholic drinks.
With even more alcohol, you will notice you can’t coordinate your muscles as well, you might slur your speech, become dizzy, forget things that have happened, and even fall asleep.
Alcohol can affect the way a medicine works.
Jonathan Kemper/UnsplashMedications can interact with alcohol to produce different or increased effects. Alcohol can interfere with the way a medicine works in the body, or it can interfere with the way a medicine is absorbed from the stomach. If your medicine has similar side-effects as being drunk, those effects can be compounded.
Not all the side-effects need to be alcohol-like. Mixing alcohol with the ADHD medicine ritalin, for example, can increase the drug’s effect on the heart, increasing your heart rate and the risk of a heart attack.
Combining alcohol with ibuprofen can lead to a higher risk of stomach upsets and stomach bleeds.
Alcohol can increase the break-down of certain medicines, such as opioids, cannabis, seizures, and even ritalin. This can make the medicine less effective. Alcohol can also alter the pathway of how a medicine is broken down, potentially creating toxic chemicals that can cause serious liver complications. This is a particular problem with paracetamol.
At its worst, the consequences of mixing alcohol and medicines can be fatal. Combining a medicine that acts on the brain with alcohol may make driving a car or operating heavy machinery difficult and lead to a serious accident.
Who is at most risk?
The effects of mixing alcohol and medicine are not the same for everyone. Those most at risk of an interaction are older people, women and people with a smaller body size.
Older people do not break down medicines as quickly as younger people, and are often on more than one medication.
Older people also are more sensitive to the effects of medications acting on the brain and will experience more side-effects, such as dizziness and falls.
Smaller and older people are often more affected.
Alfonso Scarpa/UnsplashWomen and people with smaller body size tend to have a higher blood alcohol concentration when they consume the same amount of alcohol as someone larger. This is because there is less water in their bodies that can mix with the alcohol.
What drugs can’t you mix with alcohol?
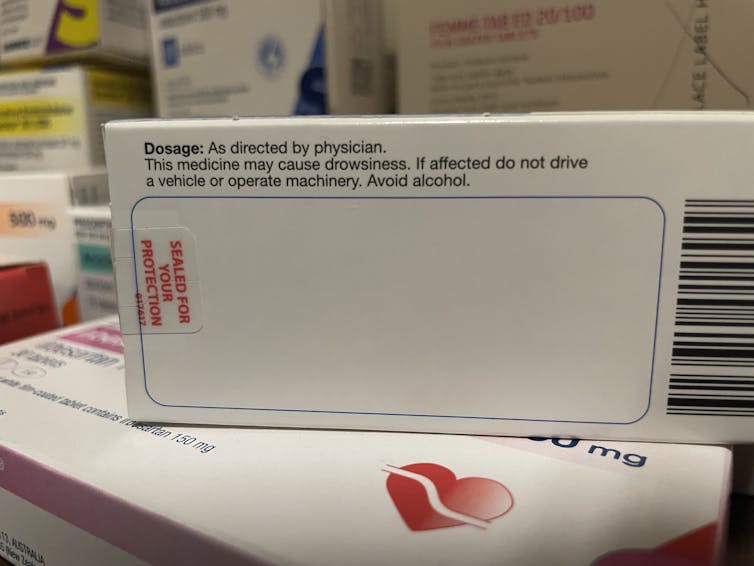
You’ll know if you can’t take alcohol because there will be a prominent warning on the box. Your pharmacist should also counsel you on your medicine when you pick up your script.
The most common alcohol-interacting prescription medicines are benzodiazepines (for anxiety, insomnia, or seizures), opioids for pain, antidepressants, antipsychotics, and some antibiotics, like metronidazole and tinidazole.
Medicines will carry a warning if you shouldn’t take them with alcohol.
Nial WheateIt’s not just prescription medicines that shouldn’t be mixed with alcohol. Some over-the-counter medicines that you shouldn’t combine with alcohol include medicines for sleeping, travel sickness, cold and flu, allergy, and pain.
Next time you pick up a medicine from your pharmacist or buy one from the local supermarket, check the packaging and ask for advice about whether you can consume alcohol while taking it.
If you do want to drink alcohol while being on medication, discuss it with your doctor or pharmacist first.
Nial Wheate, Associate Professor of the School of Pharmacy, University of Sydney; Jasmine Lee, Pharmacist and PhD Candidate, University of Sydney; Kellie Charles, Associate Professor in Pharmacology, University of Sydney, and Tina Hinton, Associate Professor of Pharmacology, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
How Much Alcohol Does It Take To Increase Cancer Risk?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Alcohol is, of course, unhealthy. Not even the famous “small glass of red” is recommended:
Alcohol also increases all-cause mortality at any dose (even “low-risk drinking”):
Alcohol Consumption Patterns and Mortality Among Older Adults
…and the World Health Organization has declared that the only safe amount of alcohol is zero:
WHO: No level of alcohol consumption is safe for our health
But what of alcohol and cancer? According to the American Association of Cancer Research’s latest report, more than half of Americans do not know that alcohol increases the risk of cancer:
Source: AACR Cancer Progress Report
Why/how does alcohol increase the risk of cancer?
There’s an obvious aspect and a less obvious but very important aspect:
- The obvious: alcohol damages almost every system in the body, and so it’s little surprise if that includes systems whose job it is to keep us safe from cancer.
- The less obvious: alcohol is largely metabolized by certain enzymes that have an impact on DNA repair, such as alcohol dehydrogenases and aldehyde dehydrogenases, amongst others, and noteworthily, acetaldehyde (the main metabolite of alcohol) is itself genotoxic.
Read more: Alcohol & Cancer
This is important, because it means alcohol also increases the risk of cancers other than the obvious head/neck, laryngeal, esophageal, liver, and colorectal cancers.
However, those cancers are of course the most well-represented of alcohol-related cancers, along with breast cancer (this has to do with alcohol’s effect on estrogen metabolism).
If you’re curious about the numbers, and the changes in risk if one reduces/quits/reprises drinking:
❝The increased alcohol-related cancer incidence was associated with dose; those who changed from nondrinking to mild (adjusted hazard ratio [aHR], 1.03; 95% CI, 1.00-1.06), moderate (aHR, 1.10; 95% CI, 1.02-1.18), or heavy (aHR, 1.34; 95% CI, 1.23-1.45) drinking levels had an associated higher risk than those who did not drink.
Those with mild drinking levels who quit drinking had a lower risk of alcohol-related cancer (aHR, 0.96; 95% CI, 0.92-0.99) than those who sustained their drinking levels.
Those with moderate (aHR, 1.07; 95% CI, 1.03-1.12) or heavy (aHR, 1.07; 95% CI, 1.02-1.12) drinking levels who quit drinking had a higher all cancer incidence than those who sustained their levels, but when quitting was sustained, this increase in risk disappeared.
Results of this study showed that increased alcohol consumption was associated with higher risks for alcohol-related and all cancers, whereas sustained quitting and reduced drinking were associated with lower risks of alcohol-related and all cancers.
Alcohol cessation and reduction should be reinforced for the prevention of cancer.❞
Source: Association Between Changes in Alcohol Consumption and Cancer Risk
Worried it’s too late?
If you’re reading this (and thus, evidently, still alive), it isn’t. It’s never too late (nor too early) to reduce, or ideally stop, drinking. Even if you already have cancer, drinking more alcohol will only exacerbate things, and abstaining from alcohol will improve your chances of recovery.
For a reassuring timeline of recovery from alcohol-related damage, see:
What Happens To Your Body When You Stop Drinking Alcohol
Want to stop, but have tried before and find it daunting?
There are a few ways to make it a lot easier:
Rethinking Drinking: How To Reduce Or Quit Alcohol
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Top 5 Foods Seniors Should Eat To Sleep Better Tonight (And 5 To Avoid)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Breus, a sleep specialist, advises:
A prescription for rest
Dr. Breus’s top 5 foods to eat for a good night’s sleep are:
1) Chia seeds: high in fiber, protein, omega-3s, calcium, magnesium, phosphorus, and tryptophan, they help raise melatonin levels for better sleep. The high fiber content also reduces late-night snacking, and in any case, it’s recommended to eat them 2–3 hours before bed. As for how, they can be added to smoothies, baked goods, salads, or made into chia seed pudding.
2) Nuts (especially pistachios & almonds): both of these nuts are rich in B vitamins and melatonin, so take your pick! He does recommend, however, no more than ¼ cup about 1.5 hours before bed. Either can be eaten as-is or with an unsweetened Greek yogurt.
3) Bananas (especially banana tea): contain magnesium, especially in the peel. Boil an organic banana (with peel) in water and drink the water, which provides magnesium and helps improve sleep. It’s recommended to drink it about an hour before bed.
10almonds tip: he doesn’t mention this, but if you prefer, you can also simply eat it—banana peel is perfectly edible, and is not tough when cooked. If you’ve ever had plantains, you’ll know how they are, and bananas (and their peel) are much softer than plantains. Boiling is fine, or alternatively you can wrap them in foil and bake them. The traditional way is to cook them in the leaves, but chances are you live somewhere that doesn’t grow bananas locally and so they didn’t come with leaves, so foil is fine.
4) Tart cherries: are rich in melatonin, antioxidants, and other anti-inflammatory compounds, which all help with falling asleep faster and reducing night awakenings. Can be consumed as juice, dried fruit, or tart cherry extract capsules. Suggested intake: once in the morning and once an hour before bed.
5) Kiwis: are high in serotonin, which aids melatonin production and sleep. This also helps regulate cortisol levels (lower cortisol promotes sleep). He recommends eating kiwi fruit about 2 hours before bed.
Also, in the category of foods (or rather: food types) to avoid before bed…
- High quantities of red meat: can disrupt sleep-related amino acid balance.
- Acidic foods: can cause acid reflux.
- High sugar foods: can slow melatonin production when consumed in the evening.
- Caffeine-rich foods & drinks: includes chocolate and coffee; avoid in the evening.
- Large meals before bed: digestion is less efficient when lying down, causing sleep disruption.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Calculate (And Enjoy) The Perfect Night’s Sleep ← Our “Expert Insights” main feature on Dr. Breus
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When should you get the updated COVID-19 vaccine?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Updated COVID-19 vaccines are now available: They’re meant to give you the best protection against the strain of the virus that is making people severely sick and also causing deaths.
Many people were infected during the persistent summer wave, which may leave you wondering when you should get the updated vaccine. The short answer is that it depends on when you last got infected or vaccinated and on your particular level of risk.
We heard from six experts—including medical doctors and epidemiologists—about when they recommend getting an updated vaccine. Read on to learn what they said. And to make it easy, check out the flowchart below.
A flowchart to help you decide when is the best time to get the 2024-2025 updated COVID-19 vaccine. If I was infected with COVID-19 this summer, when should I get the updated vaccine?
All the experts we spoke to agreed that if you were infected this summer, you should wait at least three months since you were infected to get vaccinated.
“Generally, an infection may be protective for about three months,” Dr. Ziyad Al-Aly, chief of research and development at the Veterans Affairs St. Louis Health Care System, tells PGN. “If they got infected three or more months ago, it is a good idea to get vaccinated sooner than later.”
This three-month rule applies if you got vaccinated over the summer, which may be the case for some immunocompromised people, adds Dr. Peter Chin-Hong, professor of medicine at the University of California, San Francisco.
If I didn’t get infected with COVID-19 this summer, when should I get vaccinated?
Most of the experts we talked to say that if you didn’t get infected with COVID-19 this summer, you should get the vaccine as soon as possible. Dr. Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine, emphasizes that if this applies to you, you should get vaccinated as soon as possible, especially given the current COVID-19 surge.
Al-Aly agrees. “Vaccine-derived immunity lasts for several months, and it should cover the winter season. Plus, the current vaccine is a KP.2-adapted vaccine, so it will work most optimally against KP.2 and related subvariants [such as] KP.3 that are circulating now,” Al-Aly says. “We don’t know when the virus will mutate to a variant that is not compatible with the KP.2 vaccine.”
Al-Aly adds that if you’d rather take the protection you can get right now, “It may make more sense to get vaccinated sooner than later.”
This especially applies if you’re over 65 or immunocompromised and you haven’t received a COVID-19 vaccine in a year or more because, as Chin-Hong adds, “that is the group that is being hospitalized and disproportionately dying now.”
Some experts—including epidemiologist Katelyn Jetelina, author of newsletter Your Local Epidemiologist—also say that if you’re younger than 65 and not immunocompromised, you can consider waiting and aiming to get vaccinated before Halloween to get the best protection in the winter, when we’re likely to experience another wave because of the colder weather, gathering indoors, and the holidays.
“I am more worried about the winter than the summer, so I would think of October (some time before Halloween) as the ‘Goldilocks moment’—not too early, not too late, but just right,” Chin-Hong adds. Time it “such that your antibodies peak during the winter when COVID-19 cases are expected to exceed what we are seeing this summer.”
My children are starting school—should I get them vaccinated now?
According to most experts we spoke to, now is a good time to get your children vaccinated.
Jennifer Nuzzo, professor of epidemiology and director of the Pandemic Center at the Brown University School of Public Health, adds that “with COVID-19 infection levels as high as they are and increased exposures in school,” now is a particularly good time to get an updated vaccine if people haven’t gotten COVID-19 recently.
Additionally, respiratory viruses spike when kids are back in school, so “doing everything you can to reduce your child’s risk of infection can help protect families and communities,” says epidemiologist Jessica Malaty Rivera, science communications advisor at the de Beaumont Foundation.
For more information, talk to your health care provider.
(Disclosure: The de Beaumont Foundation is a partner of The Public Good Projects, the organization that owns Public Good News.)
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: