Long-Covid Patients Are Frustrated That Federal Research Hasn’t Found New Treatments
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Erica Hayes, 40, has not felt healthy since November 2020 when she first fell ill with covid.
Hayes is too sick to work, so she has spent much of the last four years sitting on her beige couch, often curled up under an electric blanket.
“My blood flow now sucks, so my hands and my feet are freezing. Even if I’m sweating, my toes are cold,” said Hayes, who lives in Western Pennsylvania. She misses feeling well enough to play with her 9-year-old son or attend her 17-year-old son’s baseball games.
Along with claiming the lives of 1.2 million Americans, the covid-19 pandemic has been described as a mass disabling event. Hayes is one of millions of Americans who suffer from long covid. Depending on the patient, the condition can rob someone of energy, scramble the autonomic nervous system, or fog their memory, among many other http://symptoms.in/ addition to the brain fog and chronic fatigue, Hayes’ constellation of symptoms includes frequent hives and migraines. Also, her tongue is constantly swollen and dry.
“I’ve had multiple doctors look at it and tell me they don’t know what’s going on,” Hayes said about her tongue.
Estimates of prevalence range considerably, depending on how researchers define long covid in a given study, but the Centers for Disease Control and Prevention puts it at 17 million adults.
Despite long covid’s vast reach, the federal government’s investment in researching the disease — to the tune of $1.15 billion as of December — has so far failed to bring any new treatments to market.
This disappoints and angers the patient community, who say the National Institutes of Health should focus on ways to stop their suffering instead of simply trying to understand why they’re suffering.
“It’s unconscionable that more than four years since this began, we still don’t have one FDA-approved drug,” said Meighan Stone, executive director of the Long COVID Campaign, a patient-led advocacy organization. Stone was among several people with long covid who spoke at a workshop hosted by the NIH in September where patients, clinicians, and researchers discussed their priorities and frustrations around the agency’s approach to long-covid research.
Some doctors and researchers are also critical of the agency’s research initiative, called RECOVER, or Researching COVID to Enhance Recovery. Without clinical trials, physicians specializing in treating long covid must rely on hunches to guide their clinical decisions, said Ziyad Al-Aly, chief of research and development with the VA St Louis Healthcare System.
“What [RECOVER] lacks, really, is clarity of vision and clarity of purpose,” said Al-Aly, saying he agrees that the NIH has had enough time and money to produce more meaningful progress.
Now the NIH is starting to determine how to allocate an additional $662 million of funding for long-covid research, $300 million of which is earmarked for clinical trials. These funds will be allocated over the next four http://years.at/ the end of October, RECOVER issued a request for clinical trial ideas that look at potential therapies, including medications, saying its goal is “to work rapidly, collaboratively, and transparently to advance treatments for Long COVID.”
This turn suggests the NIH has begun to respond to patients. This has stirred cautious optimism among those who say that the agency’s approach to long covid has lacked urgency in the search for effective treatments.Stone calls this $300 million a down payment. She warns it’s going to take a lot more money to help people like Hayes regain some degree of health.“There really is a burden to make up this lost time now,” Stone said.
The NIH told KFF Health News and NPR via email that it recognizes the urgency in finding treatments. But to do that, there needs to be an understanding of the biological mechanisms that are making people sick, which is difficult to do with post-infectious conditions.
That’s why it has funded research into how long covid affects lung function, or trying to understand why only some people are afflicted with the condition.
Good Science Takes Time
In December 2020, Congress appropriated $1.15 billion for the NIH to launch RECOVER, raising hopes in the long-covid patient community.
Then-NIH Director Francis Collins explained that RECOVER’s goal was to better understand long covid as a disease and that clinical trials of potential treatments would come later.
According to RECOVER’s website, it has funded eight clinical trials to test the safety and effectiveness of an experimental treatment or intervention. Just one of those trials has published results.
On the other hand, RECOVER has supported more than 200 observational studies, such as research on how long covid affects pulmonary function and on which symptoms are most common. And the initiative has funded more than 40 pathobiology studies, which focus on the basic cellular and molecular mechanisms of long covid.
RECOVER’s website says this research has led to crucial insights on the risk factors for developing long covid and on understanding how the disease interacts with preexisting conditions.
It notes that observational studies are important in helping scientists to design and launch evidence-based clinical trials.
Good science takes time, said Leora Horwitz, the co-principal investigator for the RECOVER-Adult Observational Cohort at New York University. And long covid is an “exceedingly complicated” illness that appears to affect nearly every organ system, she said.
This makes it more difficult to study than many other diseases. Because long covid harms the body in so many ways, with widely variable symptoms, it’s harder to identify precise targets for treatment.
“I also will remind you that we’re only three, four years into this pandemic for most people,” Horwitz said. “We’ve been spending much more money than this, yearly, for 30, 40 years on other conditions.”
NYU received nearly $470 million of RECOVER funds in 2021, which the institution is using to spearhead the collection of data and biospecimens from up to 40,000 patients. Horwitz said nearly 30,000 are enrolled so far.
This vast repository, Horwitz said, supports ongoing observational research, allowing scientists to understand what is happening biologically to people who don’t recover after an initial infection — and that will help determine which clinical trials for treatments are worth undertaking.
“Simply trying treatments because they are available without any evidence about whether or why they may be effective reduces the likelihood of successful trials and may put patients at risk of harm,” she said.
Delayed Hopes or Incremental Progress?
The NIH told KFF Health News and NPR that patients and caregivers have been central to RECOVER from the beginning, “playing critical roles in designing studies and clinical trials, responding to surveys, serving on governance and publication groups, and guiding the initiative.”But the consensus from patient advocacy groups is that RECOVER should have done more to prioritize clinical trials from the outset. Patients also say RECOVER leadership ignored their priorities and experiences when determining which studies to fund.
RECOVER has scored some gains, said JD Davids, co-director of Long COVID Justice. This includes findings on differences in long covid between adults and kids.But Davids said the NIH shouldn’t have named the initiative “RECOVER,” since it wasn’t designed as a streamlined effort to develop treatments.
“The name’s a little cruel and misleading,” he said.
RECOVER’s initial allocation of $1.15 billion probably wasn’t enough to develop a new medication to treat long covid, said Ezekiel J. Emanuel, co-director of the University of Pennsylvania’s Healthcare Transformation Institute.
But, he said, the results of preliminary clinical trials could have spurred pharmaceutical companies to fund more studies on drug development and test how existing drugs influence a patient’s immune response.
Emanuel is one of the authors of a March 2022 covid roadmap report. He notes that RECOVER’s lack of focus on new treatments was a problem. “Only 15% of the budget is for clinical studies. That is a failure in itself — a failure of having the right priorities,” he told KFF Health News and NPR via email.
And though the NYU biobank has been impactful, Emanuel said there needs to be more focus on how existing drugs influence immune response.
He said some clinical trials that RECOVER has funded are “ridiculous,” because they’ve focused on symptom amelioration, for example to study the benefits of over-the-counter medication to improve sleep. Other studies looked at non-pharmacological interventions, such as exercise and “brain training” to help with cognitive fog.
People with long covid say this type of clinical research contributes to what many describe as the “gaslighting” they experience from doctors, who sometimes blame a patient’s symptoms on anxiety or depression, rather than acknowledging long covid as a real illness with a physiological basis.
“I’m just disgusted,” said long-covid patient Hayes. “You wouldn’t tell somebody with diabetes to breathe through it.”
Chimére L. Sweeney, director and founder of the Black Long Covid Experience, said she’s even taken breaks from seeking treatment after getting fed up with being told that her symptoms were due to her diet or mental health.
“You’re at the whim of somebody who may not even understand the spectrum of long covid,” Sweeney said.
Insurance Battles Over Experimental Treatments
Since there are still no long-covid treatments approved by the Food and Drug Administration, anything a physician prescribes is classified as either experimental — for unproven treatments — or an off-label use of a drug approved for other conditions. This means patients can struggle to get insurance to cover prescriptions.
Michael Brode, medical director for UT Health Austin’s Post-COVID-19 Program — said he writes many appeal letters. And some people pay for their own treatment.
For example, intravenous immunoglobulin therapy, low-dose naltrexone, and hyperbaric oxygen therapy are all promising treatments, he said.
For hyperbaric oxygen, two small, randomized controlled studies show improvements for the chronic fatigue and brain fog that often plague long-covid patients. The theory is that higher oxygen concentration and increased air pressure can help heal tissues that were damaged during a covid infection.
However, the out-of-pocket cost for a series of sessions in a hyperbaric chamber can run as much as $8,000, Brode said.
“Am I going to look a patient in the eye and say, ‘You need to spend that money for an unproven treatment’?” he said. “I don’t want to hype up a treatment that is still experimental. But I also don’t want to hide it.”
There’s a host of pharmaceuticals that have promising off-label uses for long covid, said microbiologist Amy Proal, president and chief scientific officer at the Massachusetts-based PolyBio Research Foundation. For instance, she’s collaborating on a clinical study that repurposes two HIV drugs to treat long covid.
Proal said research on treatments can move forward based on what’s already understood about the disease. For instance, she said that scientists have evidence — partly due to RECOVER research — that some patients continue to harbor small amounts of viral material after a covid infection. She has not received RECOVER funds but is researching antivirals.
But to vet a range of possible treatments for the millions suffering now — and to develop new drugs specifically targeting long covid — clinical trials are needed. And that requires money.
Hayes said she would definitely volunteer for an experimental drug trial. For now, though, “in order to not be absolutely miserable,” she said she focuses on what she can do, like having dinner with her http://family.at/ the same time, Hayes doesn’t want to spend the rest of her life on a beige couch.
RECOVER’s deadline to submit research proposals for potential long-covid treatments is Feb. 1.
This article is from a partnership that includes NPR and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Has Nobody Told Me This Before? – by Dr. Julie Smith
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superficially, this can be called a “self-help” book, but that undersells it rather. It’s a professionally-written (as in, by a professional psychologist) handbook full of resources. Its goal? Optimizing your mental health to help you stay resilient no matter what life throws your way.
While the marketing of this book is heavily centered around Dr. Smith’s Internet Celebrity™ status, a lot of her motivation for writing it seems to be precisely so that she can delve deeper into the ideas that her social media “bites” don’t allow room for.
Many authors of this genre pad their chapters with examples; there are no lengthy story-telling asides here, and her style doesn’t need them. She knows her field well, and knows well how to communicate the ideas that may benefit the reader.
The main “meat” of the book? Tips, tricks, guides, resources, systems, flowcharts, mental frameworks, and “if all else fails, do this” guidance. The style of the book is clear and simple, with very readable content that she keeps free from jargon without “dumbing down” or patronizing the reader.
All in all, a fine set of tools for anyone’s “getting through life” toolbox.
Get Your Personal Copy Of “Why Has Nobody Told Me This Before?” on Amazon Now!
Share This Post
-
Yoga that Helps You on the Loo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How This Video Helps You Poo
When you’re feeling a bit bloated, Yoga With Bird’s 10-minute yoga routine promises to help you release…your gas. And, perhaps, more.
From a tabletop flow to soothing twists, each pose allows you to sync your breath with movement, helping to promote organic relief.
With options to modify with pillows for extra support, this video (below) caters to everyone needing a digestive reset.
Other Toilet Tricks
If yoga isn’t your thing, or you’re interested in trying to use different methods to make your visits to the bathroom a bit easier, we’ve spoken about the ways to manage gut health, and use of probiotics or fiber, and even the prevention of hemorrhoids.
Namaste and goodbye to bloat!
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
Pasteurization: What It Does And Doesn’t Do
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pasteurization’s Effect On Risks & Nutrients
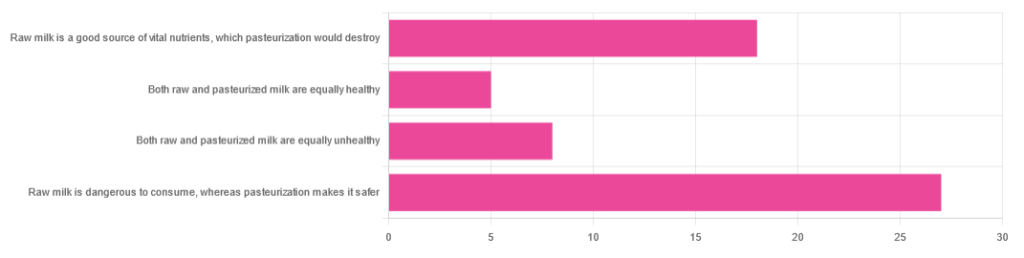
In Wednesday’s newsletter, we asked you for your health-related opinions of raw (cow’s) milk, and got the above-depicted, below-described, set of responses:
- About 47% said “raw milk is dangerous to consume, whereas pasteurization makes it safer”
- About 31% said “raw milk is a good source of vital nutrients which pasteurization would destroy”
- About 14% said “both raw milk and pasteurized milk are equally unhealthy”
- About 9% said “both raw milk and pasteurized milk are equally healthy”
Quite polarizing! So, what does the science say?
“Raw milk is dangerous to consume, whereas pasteurization makes it safer: True or False?”
True! Coincidentally, the 47% who voted for this are mirrored by the 47% of the general US population in a similar poll, deciding between the options of whether raw milk is less safe to drink (47%), just as safe to drink (15%), safer to drink (9%), or not sure (30%):
Public Fails to Appreciate Risk of Consuming Raw Milk, Survey Finds
As for what those risks are, by the way, unpasteurized dairy products are estimated to cause 840x more illness and 45x more hospitalizations than pasteurized products.
This is because unpasteurized milk can (and often does) contain E. coli, Listeria, Salmonella, Cryptosporidium, and other such unpleasantries, which pasteurization kills.
Source for both of the above claims:
(we know the title sounds vague, but all this information is easily visible in the abstract, specifically, the first two paragraphs)
Raw milk is a good source of vital nutrients which pasteurization would destroy: True or False?
False! Whether it’s a “good” source can be debated depending on other factors (e.g., if we considered milk’s inflammatory qualities against its positive nutritional content), but it’s undeniably a rich source. However, pasteurization doesn’t destroy or damage those nutrients.
Incidentally, in the same survey we linked up top, 16% of the general US public believed that pasteurization destroys nutrients, while 41% were not sure (and 43% knew that it doesn’t).
Note: for our confidence here, we are skipping over studies published by, for example, dairy farming lobbies and so forth. Those do agree, by the way, but nevertheless we like sources to be as unbiased as possible. The FDA, which is not completely unbiased, has produced a good list of references for this, about half of which we would consider biased, and half unbiased; the clue is generally in the journal names. For example, Food Chemistry and the Journal of Food Science and Journal of Nutrition are probably less biased than the International Dairy Association and the Journal of Dairy Science:
FDA | Raw Milk Misconceptions and the Danger of Raw Milk Consumption
this page covers a lot of other myths too, more than we have room to “bust” here, but it’s very interesting reading and we recommend to check it out!
Notably, we also weren’t able to find any refutation by counterexample on PubMed, with the very slight exception that some studies sometimes found that in the case of milks that were of low quality, pasteurization can reduce the vitamin E content while increasing the vitamin A content. For most milks however, no significant change was found, and in all cases we looked at, B-vitamins were comparable and vitamin D, popularly touted as a benefit of cow’s milk, is actually added later in any case. And, importantly, because this is a common argument, no change in lipid profiles appears to be findable either.
In science, when something has been well-studied and there aren’t clear refutations by counterexample, and the weight of evidence is clearly very much tipped into one camp, that usually means that camp has it right.
Milk generally is good/bad for the health: True or False?
True or False, depending on what we want to look at. It’s definitely not good for inflammation, but the whole it seems to be cancer-neutral and only increases heart disease risk very slightly:
- Keep Inflammation At Bay ← short version is milk is bad, fermented milk products are fine in moderation
- Is Dairy Scary? ← short version is that milk is neither good nor terrible; fermented dairy products however are health-positive in numerous ways when consumed in moderation
You may be wondering…
…how this goes for the safety of dairy products when it comes to the bird flu currently affecting dairy cows, so:
Take care!
Share This Post
Related Posts
-
Is TikTok right? Can adding a teaspoon of cinnamon to your coffee help you burn fat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cinnamon has been long used around the world in both sweet and savoury dishes and drinks.
But a new TikTok trend claims adding a teaspoon of cinnamon to your daily coffee (and some cocoa to make it more palatable) for one week can help you burn fat. Is there any truth to this?
Evannovostro/Shutterstock Not all cinnamon is the same
There are two types of cinnamon, both of which come from grinding the bark of the cinnamomum tree and may include several naturally occurring active ingredients.
Cassia cinnamon is the most common type available in grocery stores. It has a bitter taste and contains higher levels of one of the active ingredient cinnamaldehyde, a compound that gives cinnamon its flavour and odour. About 95% of cassia cinnamon is cinnamaldehyde.
The other is Ceylon cinnamon, which tastes sweeter. It contains about 50-60% cinnamaldehyde.
Does cinnamon burn fat? What does the research say?
A review of 35 studies examined whether consuming cinnamon could affect waist circumference, which is linked to increased body fat levels. It found cinnamon doses below 1.5 grams per day (around half a teaspoon) decreased waist circumference by 1.68cm. However, consuming more than 1.5g/day did not have a significant effect.
A meta-analysis of 21 clinical trials with 1,480 total participants found cinnamon also reduced body mass index (BMI) by 0.40kg/m² and body weight by 0.92kg. But it did not change the participants’ composition of fat or lean mass.
Another umbrella review, which included all the meta-analyses, found a small effect of cinnamon on weight loss. Participants lost an average of 0.67kg and reduced their BMI by 0.45kg/m².
The effect appears small. Radu Sebastian/Shutterstock So overall, the weight loss we see from these high-quality studies is very small, ranging anywhere from two to six months and mostly with no change in body composition.
The studies included people with different diseases, and most were from the Middle East and/or the Indian subcontinent. So we can’t be certain we would see this effect in people with other health profiles and in other countries. They were also conducted over different lengths of time from two to six months.
The supplements were different, depending on the study. Some had the active ingredient extracted from cinnamon, others used cinnamon powder. Doses varied from 0.36g to 10g per day.
They also used the two different types of cinnamon – but none of the studies used cinnamon from the grocery store.
How could cinnamon result in small amounts of weight loss?
There are several possible mechanisms.
It appears to allow blood glucose (sugar) to enter the body’s cells more quickly. This lowers blood glucose levels and can make insulin work more effectively.
It also seems to improve the way we break down fat when we need it for energy.
Finally, it may make us feel fuller for longer by slowing down how quickly the food is released from our stomach into the small intestine.
What are the risks?
Cinnamon is generally regarded as safe when used as a spice in cooking and food.
However, in recent months the United States and Australia have issued health alerts about the level of lead and other heavy metals in some cinnamon preparations.
Lead enters as a contaminant during growth (from the environment) and in harvesting. In some cases, it has been suggested there may have been intentional contamination.
Some people can have side effects from cinnamon, including gastrointestinal pain and allergic reactions.
One of the active ingredients, coumarin, can be toxic for some people’s livers. This has prompted the European Food Authority to set a limit of 0.1mg/kg of body weight.
Cassia cinnamon contains up to 1% of coumarin, and the Ceylon variety contains much less, 0.004%. So for people weighing above 60kg, 2 teaspoons (6g) of cassia cinnamon would bring them over the safe limit.
What about the coffee and cocoa?
Many people may think coffee can also help us lose weight. However there isn’t good evidence to support this yet.
An observational study found drinking one cup of regular coffee was linked to a reduction in weight that is gained over four years, but by a very small amount: an average of 0.12kg.
Good-quality cocoa and dark chocolate have also been shown to reduce weight. But again, the weight loss was small (between 0.2 and 0.4kg) and only after consuming it for four to eight weeks.
So what does this all mean?
Using cinnamon may have a very small effect on weight, but it’s unlikely to deliver meaningful weight loss without other lifestyle adjustments.
We also need to remember these trials used products that differ from the cinnamon we buy in the shops. How we store and how long we keep cinnamon might also impact or degrade the active ingredients.
And consuming more isn’t going to provide additional benefit. In fact, it could increase your risk of side effects.
So if you enjoy the taste of cinnamon in your coffee, continue to add it, but given its strong taste, you’re likely to only want to add a little.
And no matter how much we’d like this to be true, we certainly won’t gain any fat-loss benefits by consuming cinnamon on doughnuts or in buns, due to their high kilojoule count.
If you want to lose weight, there are evidence-backed approaches that won’t spoil your morning coffee.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alpha, beta, theta: what are brain states and brain waves? And can we control them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s no shortage of apps and technology that claim to shift the brain into a “theta” state – said to help with relaxation, inward focus and sleep.
But what exactly does it mean to change one’s “mental state”? And is that even possible? For now, the evidence remains murky. But our understanding of the brain is growing exponentially as our methods of investigation improve.
Brain-measuring tech is evolving
Currently, no single approach to imaging or measuring brain activity gives us the whole picture. What we “see” in the brain depends on which tool we use to “look”. There are myriad ways to do this, but each one comes with trade-offs.
We learnt a lot about brain activity in the 1980s thanks to the advent of magnetic resonance imaging (MRI).
Eventually we invented “functional MRI”, which allows us to link brain activity with certain functions or behaviours in real time by measuring the brain’s use of oxygenated blood during a task.
We can also measure electrical activity using EEG (electroencephalography). This can accurately measure the timing of brain waves as they occur, but isn’t very accurate at identifying which specific areas of the brain they occur in.
Alternatively, we can measure the brain’s response to magnetic stimulation. This is very accurate in terms of area and timing, but only as long as it’s close to the surface.
What are brain states?
All of our simple and complex behaviours, as well as our cognition (thoughts) have a foundation in brain activity, or “neural activity”. Neurons – the brain’s nerve cells – communicate by a sequence of electrical impulses and chemical signals called “neurotransmitters”.
Neurons are very greedy for fuel from the blood and require a lot of support from companion cells. Hence, a lot of measurement of the site, amount and timing of brain activity is done via measuring electrical activity, neurotransmitter levels or blood flow.
We can consider this activity at three levels. The first is a single-cell level, wherein individual neurons communicate. But measurement at this level is difficult (laboratory-based) and provides a limited picture.
As such, we rely more on measurements done on a network level, where a series of neurons or networks are activated. Or, we measure whole-of-brain activity patterns which can incorporate one or more so-called “brain states”.
According to a recent definition, brain states are “recurring activity patterns distributed across the brain that emerge from physiological or cognitive processes”. These states are functionally relevant, which means they are related to behaviour.
Brain states involve the synchronisation of different brain regions, something that’s been most readily observed in animal models, usually rodents. Only now are we starting to see some evidence in human studies.
Various kinds of states
The most commonly-studied brain states in both rodents and humans are states of “arousal” and “resting”. You can picture these as various levels of alertness.
Studies show environmental factors and activity influence our brain states. Activities or environments with high cognitive demands drive “attentional” brain states (so-called task-induced brain states) with increased connectivity. Examples of task-induced brain states include complex behaviours such as reward anticipation, mood, hunger and so on.
In contrast, a brain state such as “mind-wandering” seems to be divorced from one’s environment and tasks. Dropping into daydreaming is, by definition, without connection to the real world.
We can’t currently disentangle multiple “states” that exist in the brain at any given time and place. As mentioned earlier, this is because of the trade-offs that come with recording spatial (brain region) versus temporal (timing) brain activity.
Brain states vs brain waves
Brain state work can be couched in terms such as alpha, delta and so forth. However, this is actually referring to brain waves which specifically come from measuring brain activity using EEG.
EEG picks up on changing electrical activity in the brain, which can be sorted into different frequencies (based on wavelength). Classically, these frequencies have had specific associations:
- gamma is linked with states or tasks that require more focused concentration
- beta is linked with higher anxiety and more active states, with attention often directed externally
- alpha is linked with being very relaxed, and passive attention (such as listening quietly but not engaging)
- theta is linked with deep relaxation and inward focus
- and delta is linked with deep sleep.
Brain wave patterns are used a lot to monitor sleep stages. When we fall asleep we go from drowsy, light attention that’s easily roused (alpha), to being relaxed and no longer alert (theta), to being deeply asleep (delta).
Can we control our brain states?
The question on many people’s minds is: can we judiciously and intentionally influence our brain states?
For now, it’s likely too simplistic to suggest we can do this, as the actual mechanisms that influence brain states remain hard to detangle. Nonetheless, researchers are investigating everything from the use of drugs, to environmental cues, to practising mindfulness, meditation and sensory manipulation.
Controversially, brain wave patterns are used in something called “neurofeedback” therapy. In these treatments, people are given feedback (such as visual or auditory) based on their brain wave activity and are then tasked with trying to maintain or change it. To stay in a required state they may be encouraged to control their thoughts, relax, or breathe in certain ways.
The applications of this work are predominantly around mental health, including for individuals who have experienced trauma, or who have difficulty self-regulating – which may manifest as poor attention or emotional turbulence.
However, although these techniques have intuitive appeal, they don’t account for the issue of multiple brain states being present at any given time. Overall, clinical studies have been largely inconclusive, and proponents of neurofeedback therapy remain frustrated by a lack of orthodox support.
Other forms of neurofeedback are delivered by MRI-generated data. Participants engaging in mental tasks are given signals based on their neural activity, which they use to try and “up-regulate” (activate) regions of the brain involved in positive emotions. This could, for instance, be useful for helping people with depression.
Another potential method claimed to purportedly change brain states involves different sensory inputs. Binaural beats are perhaps the most popular example, wherein two different wavelengths of sound are played in each ear. But the evidence for such techniques is similarly mixed.
Treatments such as neurofeedback therapy are often very costly, and their success likely relies as much on the therapeutic relationship than the actual therapy.
On the bright side, there’s no evidence these treatment do any harm – other than potentially delaying treatments which have been proven to be beneficial.
Susan Hillier, Professor: Neuroscience and Rehabilitation, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Antihistamines’ Generation Gap
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are You Ready For Allergy Season?
For those of us in the Northern Hemisphere, fall will be upon us soon, and we have a few weeks to be ready for it. A common seasonal ailment is of course seasonal allergies—it’s not serious for most of us, but it can be very annoying, and can disrupt a lot of our normal activities.
Suddenly, a thing that notionally does us no real harm, is making driving dangerous, cooking take three times as long, sex laughable if not off-the-table (so to speak), and the lightest tasks exhausting.
So, what to do about it?
Antihistamines: first generation
Ye olde antihistamines such as diphenhydramine and chlorpheniramine are probably not what to do about it.
They are small molecules that cross the blood-brain barrier and affect histamine receptors in the central nervous system. This will generally get the job done, but there’s a fair bit of neurological friendly-fire going on, and while they will produce drowsiness, the sleep will usually be of poor quality. They also tax the liver rather.
If you are using them and not experiencing unwanted side effects, then don’t let us stop you, but do be aware of the risks.
See also: Long-term use of diphenhydramine ← this is the active ingredient in Benadryl in the US and Canada, but safety regulations in many other countries mean that Benadryl has different, safer active ingredients elsewhere.
Antihistamines: later generations
We’re going to aggregate 2nd gen, 3rd gen, and 4th gen antihistamines here, because otherwise we’ll be writing a history article and we don’t have room for that. But suffice it to say, later generations of antihistamines do not come with the same problems.
Instead of going in all-guns-blazing to the CNS like first-gens, they are more specific in their receptor-targetting, resulting in negligible collateral damage:
Special shout-out to cetirizine and loratadine, which are the drugs behind half the brand names you’ll see on pharmacy shelves around most of the world these days (including many in the US and Canada).
Note that these two are very often discussed in the same sentence, sit next to each other on the shelf, and often have identical price and near-identical packaging. Their effectiveness (usually: moderate) and side effects (usually: low) are similar and comparable, but they are genuinely different drugs that just happen to do more or less the same thing.
This is relevant because if one of them isn’t working for you (and/or is creating an unwanted side effect), you might want to try the other one.
Another honorable mention goes to fexofenadine, for which pretty much all the same as the above goes, though it gets talked about less (and when it does get mentioned, it’s usually by its most popular brand name, Allegra).
Finally, one that’s a little different and also deserving of a special mention is azelastine. It was recently (ish, 2021) moved from being prescription-only to being non-prescription (OTC), and it’s a nasal spray.
It can cause drowsiness, but it’s considered safe and effective for most people. Its main benefit is not really the difference in drug, so much as the difference in the route of administration (nasal rather than oral). Because the drug is in liquid spray form, it can be absorbed through the mucus lining of the nose and get straight to work on blocking the symptoms—in contrast, oral antihistamines usually have to go into your stomach and take their chances there (we say “usually”, because there are some sublingual antihistamines that dissolve under the tongue, but they are less common.)
Better than antihistamines?
Writer’s note: at this point, I was given to wonder: “wait, what was I squirting up my nose last time anyway?”—because, dear readers, at the time I got it I just bought one of every different drug on the shelf, desperate to find something that worked. What worked for me, like magic, when nothing else had, was beclometasone dipropionate, which a) smelled delightfully of flowers, which might just be the brand I got, b) needs replacing now because I got it in March 2023 and it expired July 2024, and c) is not an antihistamine at all.
But, that brings us to the final chapter for today: systemic corticosteroids
They’re not ok for everyone (check with your doctor if unsure), and definitely should not be taken if immunocompromised and/or currently suffering from an infection (including colds, flu, COVID, etc) unless your doctor tells you otherwise (and even then, honestly, double-check).
But! They can work like magic when other things don’t. Unlike antihistamines, which only block the symptoms, systemic corticosteroids tackle the underlying inflammation, which can stop the whole thing in its tracks.
Here’s how they measure up against antihistamines:
❝The results of this systematic review, together with data on safety and cost effectiveness, support the use of intranasal corticosteroids over oral antihistamines as first line treatment for allergic rhinitis.❞
~ Dr. Robert Puy et al.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: