Strong At Every Age: 15 Habits To Level Up Your Health & Fitness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not every increase in health and fitness needs to look like a training montage from the “Rocky” movies!
Making progress every day
We’ll not keep the 15 habits a secret; they are:
- Follow the one-minute rule: commit to just one minute of action—this makes starting easier, and often you’ll end up doing more once you’ve got started.
- Make the habit exciting: add fun elements to make the habit more enjoyable, like using new gear or accessories.
- Do it first: prioritize new habits by doing them early in the day to ensure they get done.
- Share the love: pair new habits with activities you already enjoy, where practical, to do “temptation bundling”.
- Embrace the uncomfortable: get used to discomfort daily to grow and build resilience for bigger changes.
- Do as little as possible: start small with habits, to minimize resistance and focus on consistency.
- Think how to be lazy: simplify processes and use shortcuts; there are no extra prizes for it having been difficult!
- Make the appointment: schedule habits with set dates and times, to increase accountability.
- Let habits evolve: adapt habits to fit current circumstances; that way you can still stay consistent over time.
- Plan ahead: prepare in advance to avoid setbacks—what could stop you from succeeding, and how can you pre-empt that?
- Pause to reflect: regularly evaluate what works and what doesn’t, to adjust and improve.
- Shut off your brain: avoid overthinking and start taking action now, not later, to build momentum.
- Question and learn: stay curious and open to learning, or else you will plateau quickly!
- Ask why: understand the deeper reasons behind any resistance, and make clear for yourself the value of the habit.
- Love your failures: embrace any setbacks as learning opportunities and, as such, stepping stones to success.
For more on all of each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Really Pick Up (And Keep!) Those Habits
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Body Scrubs: Benefits, Risks, and Guidance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I was wondering whether I should be using a body scrub in the shower, rather than just soap. What should guide me in the choice of a body scrub, and are there any risks to be aware of?❞
Body scrubs are great for giving skin a healthy glow, but are best used sparingly—over-exfoliation leads to the opposite effect (unhappy skin, premature skin aging, etc).
As for contents:
- microplastics are now banned in most places, but you might want to check any products (and their containers!) are BPA-free, pthalate free, etc.
- fragrances in body scrubs are usually a bad idea, and many essential oils have been shown to be endocrine-disruptors, which you do not want:
About the microplastics, harmful artificial chemicals in general, and what constitutes “etc”:
About the fragrances’ (including “natural” essential oils’) endocrine-disrupting shenanigans:
Endocrine-disrupting chemicals: an Endocrine Society scientific statement
So, what might you want to use instead?
If you’re feeling adventurous, you might like to try treating yourself to a pineapple-based mask instead (a muslin cloth soaked in pineapple juice will work just fine; please don’t waterboard yourself though), as the bromelain enzymes (found very generously in pineapple juice) break down dead cells without the need for scrubbing.
Another option is a homemade salt- or sugar-scrub. Put your salt or sugar into a jar, add enough warm water to cover it, leave it for about a day, adding more water if it seems in danger of drying out, until it recrystallizes with a high water content keeping it malleable to the touch; congratulations, you now have a very simple scrub. This should still not be used more than, say, once per week, though.
Last but not least, you might consider investing in a konjac sponge; they gently remove dead skin without damaging living skin. Here’s an example product on Amazon, for your convenience
For more on gentle-yet-effective skincare, you might like to read:
Clean: The New Science of Skin and the Beauty of Doing Less
Enjoy!
Share This Post
-
Cannellini Protein Gratin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A healthier twist on a classic, the protein here comes not only from the cannellini beans, but also from (at the risk of alienating French readers) a béchamel sauce that is not made using the traditional method involving flour and butter, but instead, has cashew protein as a major constituent.
You will need
- 3 medium potatoes, chopped (no need to peel them; you can if you want, but many of the nutrients are there and they’re not a problem for the recipe)
- 1 can cannellini beans (also called white kidney beans)
- 1 medium onion, chopped
- 2 stalks celery, sliced
- 1 carrot, chopped
- ½ bulb garlic, minced (or more, if you like)
- 1 jalapeño, chopped
- 2 tbsp tomato paste
- 1 tbsp chia seeds
- 2 tsp black pepper, coarse ground
- Extra virgin olive oil, for frying
For the béchamel sauce:
- ½ cup milk (we recommend a neutral-tasting plant milk, such as unsweetened soy, but go with your preference)
- ⅓ cup cashews, soaked in hot water for at least 5 minutes (longer is fine) and drained
- ¼ cup nutritional yeast
- 1 tsp garlic powder
- 1 tsp dried thyme
Method
(we suggest you read everything at least once before doing anything)
Note: it will be a bonus if you can use a pan that is good both for going on the hob and in the oven, such as a deep cast iron skillet, or a Dutch oven. If you don’t have something like that though, it’s fine, just use a sauté pan or similar, and then transfer to an oven dish for the oven part—we’ll mention this again when we get to it.
1) Preheat the oven to 250℉/175℃.
2) Heat the pan, adding some oil and then the oven; fry it for about 5 minutes, stirring often.
3) Add the potatoes, celery, carrot, garlic, and jalapeño, stirring for another 2 minutes.
4) Add the tomato paste, along with 1 cup water, the chia seeds, and the black pepper, and cook for a further 15 minutes, stirring occasionally as necessary.
5) Add the cannellini beans, and cook for another 15 minutes, stirring occasionally as necessary.
6) Blend all the ingredients for the béchamel sauce, processing it until it is smooth.
7) If you are using an oven-safe pan, pour the béchamel sauce over the bean mixture (don’t stir it; the sauce should remain on top) and transfer it to the oven. Don’t use a lid.
If you’re not using an oven safe pan, first transfer the bean mixture to an oven dish, then pour the béchamel sauce over the bean mixture (don’t stir it; the sauce should remain on top) and put it in the oven. Don’t use a lid.
8) Bake for about 15 minutes, or until turning golden-brown on top.
9) Serve! It can be enjoyed on its own, or with salad and/or rice. See also, our Tasty Versatile Rice Recipe.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- What Matters Most For Your Heart?
- The Many Health Benefits Of Garlic
- Easily Digestible Vegetarian Protein Sources
- Is Dairy Scary?
- Cashew Nuts vs Coconut – Which is Healthier?
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
Take care!
Share This Post
-
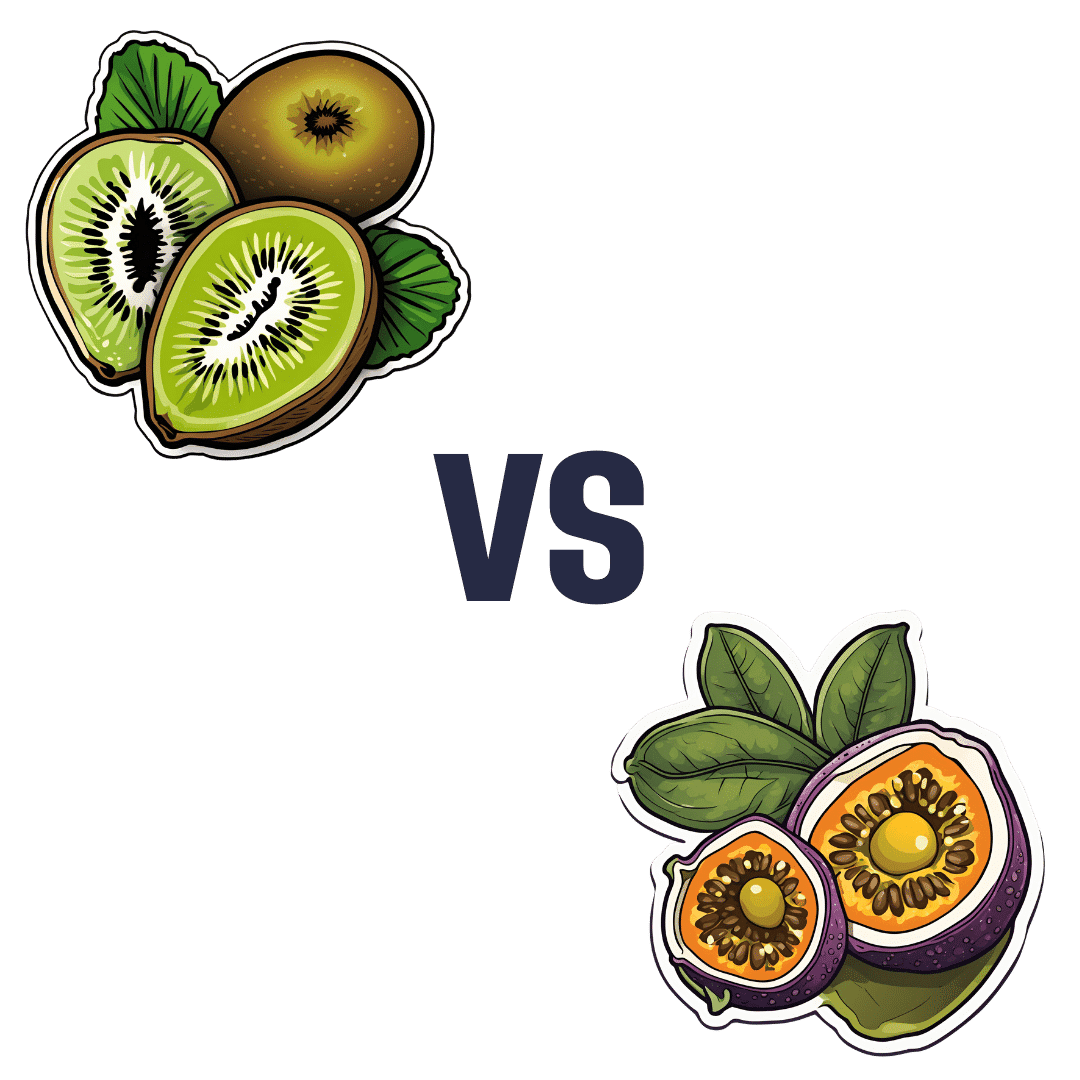
Kiwi vs Passion Fruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to passion fruit, we picked the passion fruit.
Why?
This fruit is so passionate about delivery nutrient-dense goodness, that at time of writing, nothing has beaten it yet!
In terms of macros, passion fruit has a little more protein, as well as 50% more carbs, and/but more than 3x the fiber. That last stat is particularly impressive, and also results in passion fruit having a much lower glycemic index, too. In short, a clear win for passion fruit in the macros category.
In the category of vitamins, kiwi has more of vitamins B9, C, E, and K, while passion fruit has more of vitamins A, B2, B3, and B6, making for a tie this time.
As for minerals, kiwi has more calcium, copper, manganese, and zinc, while passion fruit has more iron, magnesium, phosphorus, potassium, and selenium, resulting in a modest, marginal win for passion fruit in this category.
Adding up the categories gives a convincing win for passion fruit, but by all means enjoy either or both; diversity is good! And kiwi has its merits too (for example, it’s particularly high in vitamin K, appropriately enough).
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer
Enjoy!
Share This Post
Related Posts
-
Cancer is increasingly survivable – but it shouldn’t depend on your ability to ‘wrangle’ the health system
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One in three of us will develop cancer at some point in our lives. But survival rates have improved to the point that two-thirds of those diagnosed live more than five years.
This extraordinary shift over the past few decades introduces new challenges. A large and growing proportion of people diagnosed with cancer are living with it, rather than dying of it.
In our recently published research we examined the cancer experiences of 81 New Zealanders (23 Māori and 58 non-Māori).
We found survivorship not only entailed managing the disease, but also “wrangling” a complex health system.
Surviving disease or surviving the system
Our research focused on those who had lived longer than expected (four to 32 years since first diagnosis) with a life-limiting or terminal diagnosis of cancer.
Common to many survivors’ stories was the effort it took to wrangle the system or find others to advocate on their behalf, even to get a formal diagnosis and treatment.
By wrangling we refer to the practices required to traverse complex and sometimes unwelcoming systems. This is an often unnoticed but very real struggle that comes on top of managing the disease itself.
The common focus of the healthcare system is on symptoms, side effects of treatment and other biological aspects of cancer. But formal and informal care often falls by the wayside, despite being key to people’s everyday experiences.
Survival is often linked to someone’s social connections and capacity to access funds. Getty Images The inequities of cancer survivorship are well known. Analyses show postcodes and socioeconomic status play a strong role in the prevalence of cancer and survival.
Less well known, but illustrated in our research, is that survival is also linked to people’s capacity to manage the entire healthcare system. That includes accessing a diagnosis or treatment, or identifying and accessing alternative treatments.
Survivorship is strongly related to material resources, social connections, and understandings of how the health system works and what is available. For instance, one participant who was contemplating travelling overseas to get surgery not available in New Zealand said:
We don’t trust the public system. So thankfully we had private health insurance […] But if we went overseas, health insurance only paid out to $30,000 and I think the surgery was going to be a couple of hundred thousand. I remember Dad saying and crying and just being like, I’ll sell my business […] we’ll all put in money. It was really amazing.
Assets of survivorship
In New Zealand, the government agency Pharmac determines which medications are subsidised. Yet many participants were advised by oncologists or others to “find ways” of taking costly, unsubsidised medicines.
This often meant finding tens of thousands of dollars with no guarantees. Some had the means, but for others it meant drawing on family savings, retirement funds or extending mortgages. This disproportionately favours those with access to assets and influences who survives.
But access to economic capital is only one advantage. People also have cultural resources – often described as cultural capital.
In one case, a participant realised a drug company was likely to apply to have a medicine approved. They asked their private oncologist to lobby on their behalf to obtain the drug through a compassionate access scheme, without having to pay for it.
Others gained community support through fundraising from clubs they belonged to. But some worried about where they would find the money, or did not want to burden their community.
I had my doctor friend and some others that wanted to do some public fundraising. But at the time I said, “Look, most of the people that will be contributing are people from my community who are poor already, so I’m not going to do that option”.
Accessing alternative therapies, almost exclusively self-funded, was another layer of inequity. Some felt forced to negotiate the black market to access substances such as marijuana to treat their cancer or alleviate the side effects of orthodox cancer treatment.
Cultural capital is not a replacement for access to assets, however. Māori survivorship was greatly assisted by accessing cultural resources, but often limited by lack of material assets.
Persistence pays
The last thing we need when faced with the possibility of cancer is to have to push for formal diagnosis and care. Yet this was a common experience.
One participant was told nothing could be found to explain their abdominal pain – only to find later they had pancreatic cancer. Another was told their concerns about breathing problems were a result of anxiety related to a prior mental health history, only to learn later their earlier breast cancer had spread to their lungs.
Persistence is another layer of wrangling and it often causes distress.
Once a diagnosis was given, for many people the public health system kicked in and delivered appropriate treatment. However, experiences were patchy and variable across New Zealand.
Issues included proximity to hospitals, varying degrees of specialisation available, and the requirement of extensive periods away from home and whānau. This reflects an ongoing unevenness and lack of fairness in the current system.
When facing a terminal or life-limiting diagnosis, the capacity to wrangle the system makes a difference. We shouldn’t have to wrangle, but facing this reality is an important first step.
We must ensure it doesn’t become a continuing form of inequity, whereby people with access to material resources and social and cultural connections can survive longer.
Kevin Dew, Professor of Sociology, Te Herenga Waka — Victoria University of Wellington; Alex Broom, Professor of Sociology & Director, Sydney Centre for Healthy Societies, University of Sydney; Chris Cunningham, Professor of Maori & Public Health, Massey University; Elizabeth Dennett, Associate Professor in Surgery, University of Otago; Kerry Chamberlain, Professor of Social and Health Psychology, Massey University, and Richard Egan, Associate Professor in Health Promotion, University of Otago
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
WHO Overturns Dogma on Airborne Disease Spread. The CDC Might Not Act on It.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The World Health Organization has issued a report that transforms how the world understands respiratory infections like covid-19, influenza, and measles.
Motivated by grave missteps in the pandemic, the WHO convened about 50 experts in virology, epidemiology, aerosol science, and bioengineering, among other specialties, who spent two years poring through the evidence on how airborne viruses and bacteria spread.
However, the WHO report stops short of prescribing actions that governments, hospitals, and the public should take in response. It remains to be seen how the Centers for Disease Control and Prevention will act on this information in its own guidance for infection control in health care settings.
The WHO concluded that airborne transmission occurs as sick people exhale pathogens that remain suspended in the air, contained in tiny particles of saliva and mucus that are inhaled by others.
While it may seem obvious, and some researchers have pushed for this acknowledgment for more than a decade, an alternative dogma persisted — which kept health authorities from saying that covid was airborne for many months into the pandemic.
Specifically, they relied on a traditional notion that respiratory viruses spread mainly through droplets spewed out of an infected person’s nose or mouth. These droplets infect others by landing directly in their mouth, nose, or eyes — or they get carried into these orifices on droplet-contaminated fingers. Although these routes of transmission still happen, particularly among young children, experts have concluded that many respiratory infections spread as people simply breathe in virus-laden air.
“This is a complete U-turn,” said Julian Tang, a clinical virologist at the University of Leicester in the United Kingdom, who advised the WHO on the report. He also helped the agency create an online tool to assess the risk of airborne transmission indoors.
Peg Seminario, an occupational health and safety specialist in Bethesda, Maryland, welcomed the shift after years of resistance from health authorities. “The dogma that droplets are a major mode of transmission is the ‘flat Earth’ position now,” she said. “Hurray! We are finally recognizing that the world is round.”
The change puts fresh emphasis on the need to improve ventilation indoors and stockpile quality face masks before the next airborne disease explodes. Far from a remote possibility, measles is on the rise this year and the H5N1 bird flu is spreading among cattle in several states. Scientists worry that as the H5N1 virus spends more time in mammals, it could evolve to more easily infect people and spread among them through the air.
Traditional beliefs on droplet transmission help explain why the WHO and the CDC focused so acutely on hand-washing and surface-cleaning at the beginning of the pandemic. Such advice overwhelmed recommendations for N95 masks that filter out most virus-laden particles suspended in the air. Employers denied many health care workers access to N95s, insisting that only those routinely working within feet of covid patients needed them. More than 3,600 health care workers died in the first year of the pandemic, many due to a lack of protection.
However, a committee advising the CDC appears poised to brush aside the updated science when it comes to its pending guidance on health care facilities.
Lisa Brosseau, an aerosol expert and a consultant at the Center for Infectious Disease Research and Policy in Minnesota, warns of a repeat of 2020 if that happens.
“The rubber hits the road when you make decisions on how to protect people,” Brosseau said. “Aerosol scientists may see this report as a big win because they think everything will now follow from the science. But that’s not how this works and there are still major barriers.”
Money is one. If a respiratory disease spreads through inhalation, it means that people can lower their risk of infection indoors through sometimes costly methods to clean the air, such as mechanical ventilation and using air purifiers, and wearing an N95 mask. The CDC has so far been reluctant to press for such measures, as it updates foundational guidelines on curbing airborne infections in hospitals, nursing homes, prisons, and other facilities that provide health care. This year, a committee advising the CDC released a draft guidance that differs significantly from the WHO report.
Whereas the WHO report doesn’t characterize airborne viruses and bacteria as traveling short distances or long, the CDC draft maintains those traditional categories. It prescribes looser-fitting surgical masks rather than N95s for pathogens that “spread predominantly over short distances.” Surgical masks block far fewer airborne virus particles than N95s, which cost roughly 10 times as much.
Researchers and health care workers have been outraged about the committee’s draft, filing letters and petitions to the CDC. They say it gets the science wrong and endangers health. “A separation between short- and long-range distance is totally artificial,” Tang said.
Airborne viruses travel much like cigarette smoke, he explained. The scent will be strongest beside a smoker, but those farther away will inhale more and more smoke if they remain in the room, especially when there’s no ventilation.
Likewise, people open windows when they burn toast so that smoke dissipates before filling the kitchen and setting off an alarm. “You think viruses stop after 3 feet and drop to the ground?” Tang said of the classical notion of distance. “That is absurd.”
The CDC’s advisory committee is comprised primarily of infection control researchers at large hospital systems, while the WHO consulted a diverse group of scientists looking at many different types of studies. For example, one analysis examined the puff clouds expelled by singers, and musicians playing clarinets, French horns, saxophones, and trumpets. Another reviewed 16 investigations into covid outbreaks at restaurants, a gym, a food processing factory, and other venues, finding that insufficient ventilation probably made them worse than they would otherwise be.
In response to the outcry, the CDC returned the draft to its committee for review, asking it to reconsider its advice. Meetings from an expanded working group have since been held privately. But the National Nurses United union obtained notes of the conversations through a public records request to the agency. The records suggest a push for more lax protection. “It may be difficult as far as compliance is concerned to not have surgical masks as an option,” said one unidentified member, according to notes from the committee’s March 14 discussion. Another warned that “supply and compliance would be difficult.”
The nurses’ union, far from echoing such concerns, wrote on its website, “The Work Group has prioritized employer costs and profits (often under the umbrella of ‘feasibility’ and ‘flexibility’) over robust protections.” Jane Thomason, the union’s lead industrial hygienist, said the meeting records suggest the CDC group is working backward, molding its definitions of airborne transmission to fit the outcome it prefers.
Tang expects resistance to the WHO report. “Infection control people who have built their careers on this will object,” he said. “It takes a long time to change people’s way of thinking.”
The CDC declined to comment on how the WHO’s shift might influence its final policies on infection control in health facilities, which might not be completed this year. Creating policies to protect people from inhaling airborne viruses is complicated by the number of factors that influence how they spread indoors, such as ventilation, temperature, and the size of the space.
Adding to the complexity, policymakers must weigh the toll of various ailments, ranging from covid to colds to tuberculosis, against the burden of protection. And tolls often depend on context, such as whether an outbreak happens in a school or a cancer ward.
“What is the level of mortality that people will accept without precautions?” Tang said. “That’s another question.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From Dr. Oz to Heart Valves: A Tiny Device Charted a Contentious Path Through the FDA
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In 2013, the FDA approved an implantable device to treat leaky heart valves. Among its inventors was Mehmet Oz, the former television personality and former U.S. Senate candidate widely known as “Dr. Oz.”
In online videos, Oz has called the process that brought the MitraClip device to market an example of American medicine firing “on all cylinders,” and he has compared it to “landing a man on the moon.”
MitraClip was designed to spare patients from open-heart surgery by snaking hardware into the heart through a major vein. Its manufacturer, Abbott, said it offered new hope for people severely ill with a condition called mitral regurgitation and too frail to undergo surgery.
“It changed the face of cardiac medicine,” Oz said in a video.
But since MitraClip won FDA approval, versions of the device have been the subject of thousands of reports to the agency about malfunctions or patient injuries, as well as more than 1,100 reports of patient deaths, FDA records show. Products in the MitraClip line have been the subject of three recalls. A former employee has alleged in a federal lawsuit that Abbott promoted the device through illegal inducements to doctors and hospitals. The case is pending, and Abbott has denied illegally marketing the device.
The MitraClip story is, in many ways, a cautionary tale about the science, business, and regulation of medical devices.
Manufacturer-sponsored research on the device has long been questioned. In 2013, an outside adviser to the FDA compared some of the data marshaled in support of its approval to “poop.”
The FDA expanded its approval of MitraClip to a wider set of patients in 2019, based on a clinical trial in which Abbott was deeply involved and despite conflicting findings from another study.
In the three recalls, the first of which warned of potentially deadly consequences, neither the manufacturer nor the FDA withdrew inventory from the market. The company told doctors it was OK for them to continue using the recalled products.
In response to questions for this article, both Abbott and the FDA described MitraClip as safe and effective.
“With MitraClip, we’re addressing the needs of people with MR who often have no other options,” Abbott spokesperson Brent Tippen said. “Patients suffering from mitral regurgitation have severely limited quality of life. MitraClip can significantly improve survival, freedom for hospitalization and quality of life via a minimally invasive, now common procedure.”
An FDA spokesperson, Audra Harrison, said patient safety “is the FDA’s highest priority and at the forefront of our work in medical device regulation.”
She said reports to the FDA about malfunctions, injuries, and deaths that the device may have caused or contributed to are “consistent” with study results the FDA reviewed for its 2013 and 2019 approvals.
In other words: They were expected.
Inspiration in Italy
When a person has mitral regurgitation, blood flows backward through the mitral valve. Severe cases can lead to heart failure.
With MitraClip, flaps of the valve — known as “leaflets” — are clipped together at one or more points to achieve a tighter seal when they close. The clips are deployed via a catheter threaded through a major vein, typically from an incision in the groin. The procedure offers an alternative to connecting the patient to a heart-lung machine and repairing or replacing the mitral valve in open-heart surgery.
Oz has said in online videos that he got the idea after hearing a doctor describe a surgical technique for the mitral valve at a conference in Italy. “And on the way home that night, on a plane heading back to Columbia University, where I was on the faculty, I wrote the patent,” he told KFF Health News.
A patent obtained by Columbia in 2001, one of several associated with MitraClip, lists Oz first among the inventors.
But a Silicon Valley-based startup, Evalve, would develop the device. Evalve was later acquired by Abbott for about $400 million.
“I think the engineers and people at Evalve always cringe a little bit when they see Mehmet taking a lot of, you know, basically claiming responsibility for what was a really extraordinary team effort, and he was a small to almost no player in that team,” one of the company’s founders, cardiologist Fred St. Goar, told KFF Health News.
Oz did not respond to a request for comment on that statement.
As of 2019, the MitraClip device cost $30,000 per procedure, according to an article in a medical journal. According to the Abbott website, more than 200,000 people around the world have been treated with MitraClip.
Oz filed a financial disclosure during his unsuccessful run for the U.S. Senate in 2022 that showed him receiving hundreds of thousands of dollars in annual MitraClip royalties.
Abbott recently received FDA approval for TriClip, a variation of the MitraClip system for the heart’s tricuspid valve.
Endorsed ‘With Trepidation’
Before the FDA said yes to MitraClip in 2013, agency staffers pushed back.
Abbott had originally wanted the device approved for “patients with significant mitral regurgitation,” a relatively broad term. After the FDA objected, the company narrowed its proposal to patients at too-high risk for open-heart surgery.
Even then, in an analysis, the FDA identified “fundamental” flaws in Abbott’s data.
One example: The data compared MitraClip patients with patients who underwent open-heart surgery for valve repair — but the comparison might have been biased by differences in the expertise of doctors treating the two groups, the FDA analysis said. While MitraClip was implanted by a highly select, experienced group of interventional cardiologists, many of the doctors doing the open-heart surgeries had performed only a “very low volume” of such operations.
FDA “approval is not appropriate at this time as major questions of safety and effectiveness, as well as the overall benefit-risk profile for this device, remain unanswered,” the FDA said in a review prepared for a March 2013 meeting of a committee of outside advisers to the agency.
Some committee members expressed misgivings. “If your right shoe goes into horse poop and your left shoe goes into dog poop, it’s still poop,” cardiothoracic surgeon Craig Selzman said, according to a transcript.
The committee voted 5-4 against MitraClip on the question of whether it proved effective. But members voted 8-0 that they considered the device safe and 5-3 that the benefits of the device outweighed its risks.
Selzman voted yes on the last question “with trepidation,” he said at the time.
In October 2013, the FDA approved the MitraClip Clip Delivery System for a narrower group of patients: those with a particular type of mitral regurgitation who were considered a surgery risk.
“The reality is, there is no perfect procedure,” said Jason Rogers, an interventional cardiologist and University of California-Davis professor who is an Abbott consultant. The company referred KFF Health News to Rogers as an authority on MitraClip. He called MitraClip “extremely safe” and said some patients treated with it are “on death’s door to begin with.”
“At least you’re trying to do something for them,” he said.
Conflicting Studies
In 2019, the FDA expanded its approval of MitraClip to a wider set of patients.
The agency based that decision on a clinical trial in the United States and Canada that Abbott not only sponsored but also helped design and manage. It participated in site selection and data analysis, according to a September 2018 New England Journal of Medicine paper reporting the trial results. Some of the authors received consulting fees from Abbott, the paper disclosed.
A separate study in France reached a different conclusion. It found that, for some patients who fit the expanded profile, the device did not significantly reduce deaths or hospitalizations for heart failure over a year.
The French study, which appeared in the New England Journal of Medicine in August 2018, was funded by the government of France and Abbott. As with the North American study, some of the researchers disclosed they had received money from Abbott. However, the write-up in the journal said Abbott played no role in the design of the French trial, the selection of sites, or in data analysis.
Gregg Stone, one of the leaders of the North American study, said there were differences between patients enrolled in the two studies and how they were medicated. In addition, outcomes were better in the North American study in part because doctors in the U.S. and Canada had more MitraClip experience than their counterparts in France, Stone said.
Stone, a clinical trial specialist with a background in interventional cardiology, acknowledged skepticism toward studies sponsored by manufacturers.
“There are some people who say, ‘Oh, well, you know, these results may have been manipulated,’” he said. “But I can guarantee you that’s not the truth.”
‘Nationwide Scheme’
A former Abbott employee alleges in a lawsuit that after MitraClip won approval, the company promoted the device to doctors and hospitals using inducements such as free marketing support, the chance to participate in Abbott clinical trials, and payments for participating in “sham speaker programs.”
The former employee alleges that she was instructed to tell referring physicians that if they observed mitral regurgitation in their patients to “just send it” for a MitraClip procedure because “everything can be clipped.” She also alleges that, using a script, she was told to promote the device to hospital administrators based on financial advantages such as “growth opportunities through profitable procedures, ancillary tests, and referral streams.”
The inducements were part of a “nationwide scheme” of illegal kickbacks that defrauded government health insurance programs including Medicare and Medicaid, the lawsuit claims.
The company denied doing anything illegal and said in a court filing that “to help its groundbreaking therapy reach patients, Abbott needed to educate cardiologists and other healthcare providers.”
Those efforts are “not only routine, they are laudable — as physicians cannot use, or refer a patient to another doctor who can use, a device that they do not understand or in some cases even know about,” the company said in the filing.
Under federal law, the person who filed the suit can receive a share of any money the government recoups from Abbott. The suit was filed by a company associated with a former employee in Abbott’s Structural Heart Division, Lisa Knott. An attorney for the company declined to comment and said Knott had no comment.
Reports to the FDA
As doctors started using MitraClip, the FDA began receiving reports about malfunctions and cases in which the product might have caused or contributed to a death or an injury.
According to some reports, clips detached from valve flaps. Flaps became damaged. Procedures were aborted. Mitral leakage worsened. Doctors struggled to control the device. Clips became “entangled in chordae” — cord-like structures also known as heartstrings that connect the valve flaps to the heart muscle. Patients treated with MitraClip underwent corrective operations.
As of March 2024, the FDA had received more than 17,000 reports documenting more than 22,000 “events” involving mitral valve repair devices, FDA data shows. All but about 200 of those reports mention one iteration of MitraClip or another, a KFF Health News review of FDA data found.
Almost all the reports came from Abbott. The FDA requires manufacturers to submit reports when they learn of mishaps potentially related to their devices.
The reports are not proof that devices caused problems, and the same event might be reported multiple times. Other events may go unreported.
Despite the reports’ limitations, the FDA provides an analysis of them for the public on its website.
MitraClip’s risks weren’t a surprise.
Like the rapid-fire fine print in television ads for prescription drugs, the original product label for the device listed more than 60 types of potential complications.
Indeed, during clinical research on the device, about 6% of patients implanted with MitraClip died within 30 days, according to the label. Almost 1 in 4 — 23.6% – were dead within a year.
The FDA spokesperson, Harrison, pointed to a study originally published in 2021 in The Annals of Thoracic Surgery, based on a central registry of mitral valve procedures, that found lower rates of death after MitraClip went on the market.
“These data confirmed that the MitraClip device remains safe and effective in the real-world setting,” Harrison said.
But the study’s authors, several of whom disclosed financial or other connections to Abbott, said data was missing for more than a quarter of patients one year after the procedure.
A major measure of success would be the proportion of MitraClip patients who are alive “with an acceptable quality of life” a year after undergoing the procedure, the study said. Because such information was available for fewer than half of the living patients, “we have omitted those outcomes from this report,” the authors wrote.
If you’ve had an experience with MitraClip or another medical device and would like to tell KFF Health News about it, click here to share your story with us.
KFF Health News audience engagement producer Tarena Lofton contributed to this report.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: