Childhood Vaccination Rates, a Rare Health Bright Spot in Struggling States, Are Slipping
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Jen Fisher can do only so much to keep her son safe from the types of infections that children can encounter at school. The rest, she said, is up to other students and parents in their hometown of Franklin, Tennessee.
Fisher’s son Raleigh, 12, lives with a congenital heart condition, which has left him with a weakened immune system. For his protection, Raleigh has received all the recommended vaccines for a child his age. But even with his vaccinations, a virus that might only sideline another child could sicken him and land him in the emergency room, Fisher said.
“We want everyone to be vaccinated so that illnesses like measles and things that have basically been eradicated don’t come back,” Fisher said. “Those can certainly have a very adverse effect on Raleigh.”
For much of Raleigh’s life, Fisher could take comfort in the high childhood vaccination rate in Tennessee — a public health bright spot in a conservative state with poor health outcomes and one of the shortest life expectancies in the nation.
Mississippi and West Virginia, two similarly conservative states with poor health outcomes and short life expectancies, also have some of the highest vaccination rates for kindergartners in the nation — a seeming contradiction that stems from the fact that childhood vaccination requirements don’t always align with states’ other characteristics, said James Colgrove, a Columbia University professor who studies factors that influence public health.
“The kinds of policies that states have don’t map neatly on to ‘red’ versus ‘blue’ or one region or another,” Colgrove said.
Advocates, doctors, public health officials, and researchers worry such public health bright spots in some states are fading: Many states have recently reported an increase in people opting out of vaccines for their kids as Americans’ views shift.
During the 2023-24 school year, the percentage of kindergartners exempted from one or more vaccinations rose to 3.3%, the highest ever reported, with increases in 40 states and Washington, D.C., according to Centers for Disease Control and Prevention data. Tennessee and Mississippi were among those with increases. Nearly all exemptions nationally were for nonmedical reasons.
Vaccine proponents worry anti-vaccine messaging could accelerate a growing “health freedom” movement that has been pushed by leaders in states such as Florida. Momentum against vaccines is likely to continue to grow with the election of Donald Trump as president and his proposed nomination of anti-vaccine activist Robert F. Kennedy Jr. as secretary of the Department of Health and Human Services.
Pediatricians in states with high exemption rates, such as Florida and Georgia, say they’re concerned by what they see — declining immunization levels for kindergartners, which could lead to a resurgence in vaccine-preventable diseases such as measles. The Florida Department of Health reported nonmedical exemption rates as high as 50% for children in some areas.
“The religious exemption is huge,” said Brandon Chatani, a pediatric infectious disease doctor in Orlando. “That has allowed for an easy way for these kids to enter schools without vaccines.”
In many states, it’s easier to get a religious exemption than a medical one, which often requires signoff from a doctor.
Over the past decade, California, Connecticut, Maine, and New York have removed religious and philosophical exemptions from school vaccination requirements. West Virginia has not had them.
Idaho, Alaska, and Utah had the highest exemption rates for the 2023-24 school year, according to the CDC. Those states allow parents or legal guardians to exempt their children for religious reasons by submitting a notarized form or a signed statement.
Florida and Georgia, with some of the lowest reported minimum vaccination rates for kindergartners, allow parents to exempt their children by submitting a form with the child’s school or day care.
Both states have reported declines in uptake of the measles, mumps, and rubella vaccine, which is one of the most common childhood shots. In Georgia, MMR coverage for kindergartners dropped to 88.4% in the 2023-24 school year from 93.1% in 2019-20, according to the CDC. Florida dropped to 88.1% from 93.5% during the same period.
Andi Shane, a pediatric infectious disease specialist in Atlanta, traces Georgia’s declining rates to families who lack access to a pediatrician. State policies on exemptions are also key, she said.
“There’s lots of data to support the fact that when personal belief exemptions are not permitted, that vaccination rates are higher,” she said.
In December, Georgia public health officials put out an advisory saying the state had recorded significantly more whooping cough cases than in the prior year. According to CDC data, Georgia reported 280 cases in 2024 compared with 96 the year before.
Until 2023, Mississippi was one of the few states that allowed parents to opt out of vaccinating their kids only for medical reasons — and only with the approval of a doctor. That gave it among the highest vaccination rates in the nation as of the 2023-24 school year.
“It’s one of the few things Mississippi has done well,” said Anita Henderson, a pediatrician who has practiced in the southern part of the state for nearly 30 years. In terms of health, she said, childhood vaccination rates were the state’s one “shining star.”
But that changed in April 2023 when a federal judge ordered state officials to start allowing religious exemptions. The ruling has emboldened many families, Henderson said.
“We are seeing more and more skepticism, more and more vaccine hesitancy, and a lack of confidence because of this ruling,” she said.
State officials have granted more than 5,000 religious exemptions since the court order allowing them, according to the state health department. Daniel Edney, the state health officer, said most of the requests have come from “more affluent” residents in “pockets” of the state.
“Most people listen to the expert opinions of their pediatricians and family medicine doctors to stay on the vaccine schedule, because it’s what is best to protect their children,” he said.
West Virginia’s vaccine law — which hasn’t allowed nonmedical exemptions — also could soon change, Matthew Christiansen said in December before he resigned as the state’s health officer.
A bill that would have broadened exemptions made it through the legislature last year but was vetoed by outgoing Republican Gov. Jim Justice. The new governor, Republican Pat Morrisey, has been a vocal critic of vaccine mandates. And just a day after being inaugurated, he issued an executive order to propose provisions by Feb. 1 that could allow religious and conscientious exemptions.
“I want to send a message that if you have a religious belief, then we’re going to have an exception,” he said at a Jan. 14 press conference. “We’re not going to be the outlier.”
People asserting their personal freedoms to decline vaccines for their kids can ultimately curtail the ability of others to live full lives, Christiansen said. “Kids getting measles and mumps and polio and being paralyzed for their whole life is an impediment on personal freedom and autonomy for those kids,” he said.
Since the covid pandemic, anti-vaccine sentiment has been growing in Tennessee. One organization, Stand for Health Freedom, drafted a letter for constituents to send to their state lawmakers calling for the resignation of the medical director of Tennessee’s Vaccine-Preventable Diseases and Immunization Program. The group said she demonstrated a “lack of respect for the informed consent rights” of the people.
“They feel emboldened by the idea that this presidential administration seems to feel very strongly that a lot of these issues should be taken back to the states,” said Emily Delikat, director of Tennessee Families for Vaccines, a pro-vaccine group.
Ultimately, like many effective public health interventions, vaccines are a victim of their own success, said Henderson, the Mississippi pediatrician. Most people haven’t seen outbreaks of measles or polio, so they forget how dangerous the diseases are, she said.
“It may unfortunately take a resurgence of those diseases to raise awareness to the fact that these are dangerous, these are deadly, these are preventable,” she said. “I hope it doesn’t come to that.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can you drink your fruit and vegetables? How does juice compare to the whole food?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you struggle to eat your fruits and vegetables? You are not alone. Less than 5% of Australians eat the recommended serves of fresh produce each day (with 44% eating enough fruit but only 6% eating the recommended vegetables).
Adults should aim to eat at least five serves of vegetables (or roughly 375 grams) and two serves of fruit (about 300 grams) each day. Fruits and vegetables help keep us healthy because they have lots of nutrients (vitamins, minerals and fibre) and health-promoting bioactive compounds (substances not technically essential but which have health benefits) without having many calories.
So, if you are having trouble eating the rainbow, you might be wondering – is it OK to drink your fruits and vegetables instead in a juice or smoothie? Like everything in nutrition, the answer is all about context.
Darina Belonogova/Pexels It might help overcome barriers
Common reasons for not eating enough fruits and vegetables are preferences, habits, perishability, cost, availability, time and poor cooking skills. Drinking your fruits and vegetables in juices or smoothies can help overcome some of these barriers.
Juicing or blending can help disguise tastes you don’t like, like bitterness in vegetables. And it can blitz imperfections such as bruises or soft spots. Preparation doesn’t take much skill or time, particularly if you just have to pour store-bought juice from the bottle. Treating for food safety and shipping time does change the make up of juices slightly, but unsweetened juices still remain significant sources of nutrients and beneficial bioactives.
Juicing can extend shelf life and reduce the cost of nutrients. In fact, when researchers looked at the density of nutrients relative to the costs of common foods, fruit juice was the top performer.
So, drinking my fruits and veggies counts as a serve, right?
How juice is positioned in healthy eating recommendations is a bit confusing. The Australian Dietary Guidelines include 100% fruit juice with fruit but vegetable juice isn’t mentioned. This is likely because vegetable juices weren’t as common in 2013 when the guidelines were last revised.
The guidelines also warn against having juice too often or in too high amounts. This appears to be based on the logic that juice is similar, but not quite as good as, whole fruit. Juice has lower levels of fibre compared to fruits, with fibre important for gut health, heart health and promoting feelings of fullness. Juice and smoothies also release the sugar from the fruit’s other structures, making them “free”. The World Health Organization recommends we limit free sugars for good health.
But fruit and vegetables are more than just the sum of their parts. When we take a “reductionist” approach to nutrition, foods and drinks are judged based on assumptions made about limited features such as sugar content or specific vitamins.
But these features might not have the impact we logically assume because of the complexity of foods and people. When humans eat varied and complex diets, we don’t necessarily need to be concerned that some foods are lower in fibre than others. Juice can retain the nutrients and bioactive compounds of fruit and vegetables and even add more because parts of the fruit we don’t normally eat, like the skin, can be included.
Juicing or blending might mean you eat different parts of the fruit or vegetable. flyingv3/Shutterstock So, it is healthy then?
A recent umbrella review of meta-analyses (a type of research that combines data from multiple studies of multiple outcomes into one paper looked at the relationship between 100% juice and a range of health outcomes.
Most of the evidence showed juice had a neutral impact on health (meaning no impact) or a positive one. Pure 100% juice was linked to improved heart health and inflammatory markers and wasn’t clearly linked to weight gain, multiple cancer types or metabolic markers (such as blood sugar levels).
Some health risks linked to drinking juice were reported: death from heart disease, prostate cancer and diabetes risk. But the risks were all reported in observational studies, where researchers look at data from groups of people collected over time. These are not controlled and do not record consumption in the moment. So other drinks people think of as 100% fruit juice (such as sugar-sweetened juices or cordials) might accidentally be counted as 100% fruit juice. These types of studies are not good at showing the direct causes of illness or death.
What about my teeth?
The common belief juice damages teeth might not stack up. Studies that show juice damages teeth often lump 100% juice in with sweetened drinks. Or they use model systems like fake mouths that don’t match how people drinks juice in real life. Some use extreme scenarios like sipping on large volumes of drink frequently over long periods of time.
Juice is acidic and does contain sugars, but it is possible proper oral hygiene, including rinsing, cleaning and using straws can mitigate these risks.
Again, reducing juice to its acid level misses the rest of the story, including the nutrients and bioactives contained in juice that are beneficial to oral health.
Juice might be more convenient and could replace less healthy drinks. PintoArt/Shutterstock So, what should I do?
Comparing whole fruit (a food) to juice (a drink) can be problematic. They serve different culinary purposes, so aren’t really interchangeable.
The Australian Guide to Healthy Eating recommends water as the preferred beverage but this assumes you are getting all your essential nutrients from eating.
Where juice fits in your diet depends on what you are eating and what other drinks it is replacing. Juice might replace water in the context of a “perfect” diet. Or juice might replace alcohol or sugary soft drinks and make the relative benefits look very different.
On balance
Whether you want to eat your fruits and vegetables or drink them comes down to what works for you, how it fits into the context of your diet and your life.
Smoothies and juices aren’t a silver bullet, and there is no evidence they work as a “cleanse” or detox. But, with society’s low levels of fruit and vegetable eating, having the option to access nutrients and bioactives in a cheap, easy and tasty way shouldn’t be discouraged either.
Emma Beckett, Adjunct Senior Lecturer, Nutrition, Dietetics & Food Innovation – School of Health Sciences, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Don’t Do *This* If You’re Over 50 (And Want Better Sleep)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Breus, sleep specialist, explains:
Don’t make these mistakes
Dr. Breus recommends avoiding…
- Misusing magnesium: magnesium is a helpful sleep aid but must be carefully monitored. Recommended doses are 250mg for women and 300–350 mg for men, with slight adjustments for hot climates or active lifestyles. Overdosing can cause stomach issues, diarrhea, and dehydration, disrupting sleep. He recommends starting with magnesium glycinate for fewer stomach issues, and later mix with magnesium citrate. Always check supplements to avoid excessive magnesium intake.
- Misusing melatonin: melatonin production declines after age 55–60, making low-dose supplementation (0.5–1 mg) beneficial. He recommends, however, avoiding high doses (3–10mg), and he recommends to take it 90 minutes before bedtime. Melatonin interacts with some medications (including some meds for blood pressure or depression), so consult a pharmacist before use to avoid risks like serotonin syndrome.
- Going to bed too early: going to bed too early disrupts circadian rhythms and reduces sleep drive, causing earlier waking. Now, being an “early bird” is a generally healthy thing, but if you’re already getting up at 5am, say, you probably want your schedule to not continue to creep further forwards until you become nocturnal. Set a consistent wake-up time and count 7.5 hours backward (plus a set time to fall asleep, e.g. 20 minutes, but you’ll know what it is for you) to determine bedtime.
- Excessive caffeine consumption: from the heading, it may seem like a no-brainer, but older adults metabolize caffeine 33% slower on average, prolonging its effects. Dr. Breus recommends to reduce intake with “caffeine fading,” switching to half-caffeinated coffee for a while and then considering transitioning to decaf. He also suggests enjoying increasingly lower-caffeine teas, like black tea in the morning, matcha in the afternoon, and herbal tea at night to reduce caffeine’s impact on sleep.
- Falling foul of serotonin: avoid taking 5-HTP supplements with SSRI antidepressants like Prozac or Zoloft due to the risk of serotonin syndrome.
- Consider checking for physical problems: if you regularly wake up tired and/or groggy (despite having ostensibly had enough sleep, and there not being a pharmaceutical explanation for your grogginess), consider screening for sleep apnea. Home sleep tests are a convenient way to identify and treat this common but often undiagnosed condition.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How to Fall Asleep Faster: CBT-Insomnia Treatment
Take care!
Share This Post
-
Shredded Wheat vs Organic Crunch – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Shredded Wheat to Organic Crunch, we picked the Shredded Wheat.
Why?
In this battle of the cereals, it comes down to the ingredients:
- The Shredded Wheat cereal has two ingredients: wheat (shredded), and BHT. The latter is a phenolic compound and antioxidant.
- The Organic Crunch cereal has lots of ingredients, of which the first two are wheat flour, and sugar.
This means that, per serving…
- The Shredded Wheat cereal has 7g fiber and 0g sugar
- The Organic Crunch cereal has 3g fiber and 12g sugar
Quite a difference! Sometimes, the “Organic Crunch” of a product comes from crunchy sugar.
You can check them out side-by-side here:
Shredded Wheat | Organic Crunch
Want to know more?
There’s a popular view that the only way to get fiber is to eat things that look (and potentially taste) like cardboard. Not so! There are delicious options:
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Enjoy!
Share This Post
Related Posts
-
What’s the difference between physical and chemical sunscreens? And which one should you choose?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sun exposure can accelerate ageing, cause skin burns, erythema (a skin reaction), skin cancer, melasmas (or sun spots) and other forms of hyperpigmentation – all triggered by solar ultraviolet radiation.
Approximately 80% of skin cancer cases in people engaged in outdoor activities are preventable by decreasing sun exposure. This can be done in lots of ways including wearing protective clothing or sunscreens.
But not all sunscreens work in the same way. You might have heard of “physical” and “chemical” sunscreens. What’s the difference and which one is right for you?
How sunscreens are classified
Sunscreens are grouped by their use of active inorganic and organic ultraviolet (UV) filters. Chemical sunscreens use organic filters such as cinnamates (chemically related to cinnamon oil) and benzophenones. Physical sunscreens (sometimes called mineral sunscreens) use inorganic filters such as titanium and zinc oxide.
These filters prevent the effects of UV radiation on the skin.
Organic UV filters are known as chemical filters because the molecules in them change to stop UV radiation reaching the skin. Inorganic UV filters are known as physical filters, because they work through physical means, such as blocking, scattering and reflection of UV radiation to prevent skin damage.
Nano versus micro
The effectiveness of the filters in physical sunscreen depends on factors including the size of the particle, how it’s mixed into the cream or lotion, the amount used and the refraction index (the speed light travels through a substance) of each filter.
When the particle size in physical sunscreens is large, it causes the light to be scattered and reflected more. That means physical sunscreens can be more obvious on the skin, which can reduce their cosmetic appeal.
Nanoparticulate forms of physical sunscreens (with tiny particles smaller than 100 nanometers) can improve the cosmetic appearance of creams on the skin and UV protection, because the particles in this size range absorb more radiation than they reflect. These are sometimes labelled as “invisible” zinc or mineral formulations and are considered safe.
So how do chemical sunscreens work?
Chemical UV filters work by absorbing high-energy UV rays. This leads to the filter molecules interacting with sunlight and changing chemically.
When molecules return to their ground (or lower energy) state, they release energy as heat, distributed all over the skin. This may lead to uncomfortable reactions for people with skin sensitivity.
Generally, UV filters are meant to stay on the epidermis (the first skin layer) surface to protect it from UV radiation. When they enter into the dermis (the connective tissue layer) and bloodstream, this can lead to skin sensitivity and increase the risk of toxicity. The safety profile of chemical UV filters may depend on whether their small molecular size allows them to penetrate the skin.
Chemical sunscreens, compared to physical ones, cause more adverse reactions in the skin because of chemical changes in their molecules. In addition, some chemical filters, such as dibenzoylmethane tend to break down after UV exposure. These degraded products can no longer protect the skin against UV and, if they penetrate the skin, can cause cell damage.
Due to their stability – that is, how well they retain product integrity and effectiveness when exposed to sunlight – physical sunscreens may be more suitable for children and people with skin allergies.
Although sunscreen filter ingredients can rarely cause true allergic dermatitis, patients with photodermatoses (where the skin reacts to light) and eczema have higher risk and should take care and seek advice.
What to look for
The best way to check if you’ll have a reaction to a physical or chemical sunscreen is to patch test it on a small area of skin.
And the best sunscreen to choose is one that provides broad-spectrum protection, is water and sweat-resistant, has a high sun protection factor (SPF), is easy to apply and has a low allergy risk.
Health authorities recommend sunscreen to prevent sun damage and cancer. Chemical sunscreens have the potential to penetrate the skin and may cause irritation for some people. Physical sunscreens are considered safe and effective and nanoparticulate formulations can increase their appeal and ease of use.
Yousuf Mohammed, Dermatology researcher, The University of Queensland and Khanh Phan, Postdoctoral research associate, Frazer Institute, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
No, beetroot isn’t vegetable Viagra. But here’s what else it can do
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beetroot has been in the news for all the wrong reasons. Supply issues in recent months have seen a shortage of tinned beetroot on Australian supermarket shelves. At one point, a tin was reportedly selling on eBay for more than A$65.
But as supplies increase, we turn our attention to beetroot’s apparent health benefits.
Is beetroot really vegetable Viagra, as UK TV doctor Michael Mosley suggests? What about beetroot’s other apparent health benefits – from reducing your blood pressure to improving your daily workout? Here’s what the science says.
What’s so special about beetroot?
Beetroot – alongside foods such as berries, nuts and leafy greens – is a “superfood”. It contains above-average levels per gram of certain vitamins and minerals.
Beetroot is particularly rich in vitamin B and C, minerals, fibre and antioxidants.
Most cooking methods don’t significantly alter its antioxidant levels. Pressure cooking does, however, lower levels of carotenoid (a type of antioxidant) compared to raw beetroot.
Processing into capsules, powders, chips or juice may affect beetroot’s ability to act as an antioxidant. However, this can vary between products, including between different brands of beetroot juice.
Is beetroot really vegetable Viagra?
The Romans are said to have used beetroot and its juice as an aphrodisiac.
But there’s limited scientific evidence to say beetroot improves your sex life. This does not mean it doesn’t. Rather, the vast number of scientific studies looking at the effect of beetroot have not measured libido or other aspects of sexual health.
How could it work?
When we eat beetroot, chemical reactions involving bacteria and enzymes transform the nitrate in beetroot into nitrite, then to nitric oxide. Nitric oxide helps dilate (widen) blood vessels, potentially improving circulation.
The richest sources of dietary nitric oxide that have been tested in clinical studies are beetroot, rocket and spinach.
Nitric oxide is also thought to support testosterone in its role in controlling blood flow before and during sex in men.
Beetroot’s ability to improve blood flow can benefit the circulatory system of the heart and blood vessels. This may positively impact sexual function, theoretically in men and women.
Therefore, it is reasonable to suggest there could be a modest link between beetroot and preparedness for sex, but don’t expect it to transform your sex life.
What else could it do?
Beetroot has received increasing attention over recent years due to its antioxidant and anti-tumour effect in humans.
Clinical trials have not verified all beetroot’s active ingredients and their effects. However, beetroot may be a potentially helpful treatment for various health issues related to oxidative stress and inflammation, such as cancer and diabetes. The idea is that you can take beetroot supplements or eat extra beetroot alongside your regular medicines (rather than replace them).
There is evidence beetroot juice can help lower systolic blood pressure (the first number in your blood pressure reading) by 2.73-4.81 mmHg (millimetres of mercury, the standard unit of measuring blood pressure) in people with high blood pressure. Some researchers say this reduction is comparable to the effects seen with certain medications and dietary interventions.
Other research finds even people without high blood pressure (but at risk of it) could benefit.
Beetroot may also improve athletic performance. Some studies show small benefits for endurance athletes (who run, swim or cycle long distances). These studies looked at various forms of the food, such as beetroot juice as well as beetroot-based supplements.
How to get more beetroot in your diet
There is scientific evidence to support positive impacts of consuming beetroot in whole, juice and supplement forms. So even if you can’t get hold of tinned beetroot, there are plenty of other ways you can get more beetroot into your diet. You can try:
- raw beetroot – grate raw beetroot and add it to salads or coleslaw, or slice beetroot to use as a crunchy topping for sandwiches or wraps
- cooked beetroot – roast beetroot with olive oil, salt and pepper for a flavour packed side dish. Alternatively, steam beetroot and serve it as a standalone dish or mixed into other dishes
- beetroot juice – make fresh beetroot juice using a juicer. You can combine it with other fruits and vegetables for added flavour. You can also blend raw or cooked beetroot with water and strain to make a juice
- smoothies – add beetroot to your favourite smoothie. It pairs well with fruits such as berries, apples and oranges
- soups – use beetroot in soups for both flavour and colour. Borscht is a classic beetroot soup, but you can also experiment with other recipes
- pickled beetroot – make pickled beetroot at home, or buy it from the supermarket. This can be a tasty addition to salads or sandwiches
- beetroot hummus – blend cooked beetroot into your homemade hummus for a vibrant and nutritious dip. You can also buy beetroot hummus from the supermarket
- grilled beetroot – slice beetroot and grill it for a smoky flavour
- beetroot chips – slice raw beetroot thinly, toss the slices with olive oil and your favourite seasonings, then bake or dehydrate them to make crispy beetroot chips
- cakes and baked goods – add grated beetroot to muffins, cakes, or brownies for a moist and colourful twist.
You can add beetroot to baked goods. Ekaterina Khoroshilova/Shutterstock Are there any downsides?
Compared to the large number of studies on the beneficial effects of beetroot, there is very little evidence of negative side effects.
If you eat large amounts of beetroot, your urine may turn red or purple (called beeturia). But this is generally harmless.
There have been reports in some countries of beetroot-based dietary supplements contaminated with harmful substances, yet we have not seen this reported in Australia.
What’s the take-home message?
Beetroot may give some modest boost to sex for men and women, likely by helping your circulation. But it’s unlikely to transform your sex life or act as vegetable Viagra. We know there are many contributing factors to sexual wellbeing. Diet is only one.
For individually tailored support talk to your GP or an accredited practising dietitian.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
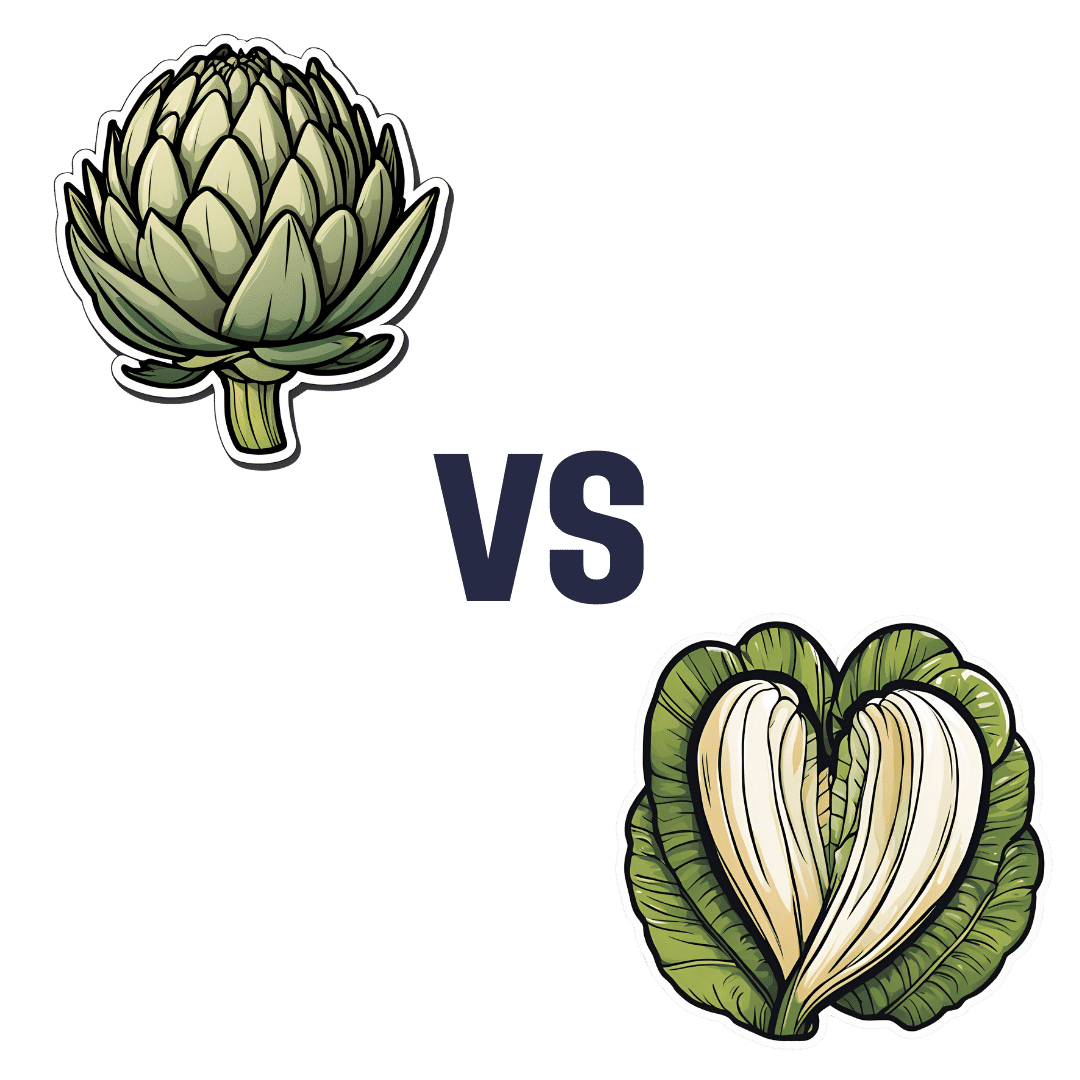
Artichoke vs Heart of Palm– Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing artichoke to heart of palm, we picked the artichoke.
Why?
If you were thinking “isn’t heart of palm full of saturated fat?” then no… Palm oil is, but heart of palm itself has 0.62g/100g fat, of which, 0.13g saturated fat. So, negligible.
As for the rest of the macros, artichoke has more protein, carbs, and fiber, thus being the “more food per food” option. Technically heart of palm has the lower glycemic index, but they are both low-GI foods, so it’s really not a factor here.
Vitamins are where artichoke shines; artichoke has more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, K, and choline, while heart of palm is not higher in any vitamins.
The minerals situation is more balanced: artichoke has more copper, magnesium, phosphorus, and potassium, while heart of palm has more iron, manganese, selenium, and zinc.
Adding up the categories, the winner of this “vegetables with a heart” face-off is clearly artichoke.
Fun fact: in French, “to have the heart of an artichoke” (avoir le coeur d’un artichaut) means to fall in love easily. Perfect vegetable for a romantic dinner, perhaps (especially with all those generous portions of B-vitamins)!
Want to learn more?
You might like to read:
Artichoke vs Cabbage – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: