State Regulators Know Health Insurance Directories Are Full of Wrong Information. They’re Doing Little to Fix It.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: America’s Mental Barrier:How Insurers Interfere With Mental Health Care
- Extensive Errors: Many states have sought to make insurers clean up their health plans’ provider directories over the past decade. But the errors are still widespread.
- Paltry Penalties: Most state insurance agencies haven’t issued a fine for provider directory errors since 2019. When companies have been penalized, the fines have been small and sporadic.
- Ghostbusters: Experts said that stricter regulations and stronger fines are needed to protect insurance customers from these errors, which are at the heart of so-called ghost networks.
These highlights were written by the reporters and editors who worked on this story.
To uncover the truth about a pernicious insurance industry practice, staffers with the New York state attorney general’s office decided to tell a series of lies.
So, over the course of 2022 and 2023, they dialed hundreds of mental health providers in the directories of more than a dozen insurance plans. Some staffers pretended to call on behalf of a depressed relative. Others posed as parents asking about their struggling teenager.
They wanted to know two key things about the supposedly in-network providers: Do you accept insurance? And are you accepting new patients?
The more the staffers called, the more they realized that the providers listed either no longer accepted insurance or had stopped seeing new patients. That is, if they heard back from the providers at all.
In a report published last December, the office described rampant evidence of these “ghost networks,” where health plans list providers who supposedly accept that insurance but who are not actually available to patients. The report found that 86% of the listed mental health providers who staffers had called were “unreachable, not in-network, or not accepting new patients.” Even though insurers are required to publish accurate directories, New York Attorney General Letitia James’ office didn’t find evidence that the state’s own insurance regulators had fined any insurers for their errors.
Shortly after taking office in 2021, Gov. Kathy Hochul vowed to combat provider directory misinformation, so there seemed to be a clear path to confronting ghost networks.
Yet nearly a year after the publication of James’ report, nothing has changed. Regulators can’t point to a single penalty levied for ghost networks. And while a spokesperson for New York state’s Department of Financial Services has said that “nation-leading consumer protections” are in the works, provider directories in the state are still rife with errors.
A similar pattern of errors and lax enforcement is happening in other states as well.
In Arizona, regulators called hundreds of mental health providers listed in the networks of the state’s most popular individual health plans. They couldn’t schedule visits with nearly 2 out of every 5 providers they called. None of those companies have been fined for their errors.
In Massachusetts, the state attorney general investigated alleged efforts by insurers to restrict their customers’ mental health benefits. The insurers agreed to audit their mental health provider listings but were largely allowed to police themselves. Insurance regulators have not fined the companies for their errors.
In California, regulators received hundreds of complaints about provider listings after one of the nation’s first ghost network regulations took effect in 2016. But under the new law, they have actually scaled back on fining insurers. Since 2016, just one plan was fined — a $7,500 penalty — for posting inaccurate listings for mental health providers.
ProPublica reached out to every state insurance commission to see what they have done to curb rampant directory errors. As part of the country’s complex patchwork of regulations, these agencies oversee plans that employers purchase from an insurer and that individuals buy on exchanges. (Federal agencies typically oversee plans that employers self-fund or that are funded by Medicare.)
Spokespeople for the state agencies told ProPublica that their “many actions” resulted in “significant accountability.” But ProPublica found that the actual actions taken so far do not match the regulators’ rhetoric.
“One of the primary reasons insurance commissions exist is to hold companies accountable for what they are advertising in their contracts,” said Dr. Robert Trestman, a leading American Psychiatric Association expert who has testified about ghost networks to the U.S. Senate Committee on Finance. “They’re not doing their job. If they were, we would not have an ongoing problem.”
Most states haven’t fined a single company for publishing directory errors since 2019. When they do, the penalties have been small and sporadic. In an average year, fewer than a dozen fines are issued by insurance regulators for directory errors, according to information obtained by ProPublica from almost every one of those agencies. All those fines together represent a fraction of 1% of the billions of dollars in profits made by the industry’s largest companies. Health insurance experts told ProPublica that the companies treat the fines as a “cost of doing business.”
Insurers acknowledge that errors happen. Providers move. They retire. Their open appointments get booked by other patients. The industry’s top trade group, AHIP, has told lawmakers that companies contact providers to verify that their listings are accurate. The trade group also has stated that errors could be corrected faster if the providers did a better job updating their listings.
But providers have told us that’s bogus. Even when they formally drop out of a network, they’re not always removed from the insurer’s lists.
The harms from ghost networks are real. ProPublica reported on how Ravi Coutinho, a 36-year-old entrepreneur from Arizona, had struggled for months to access the mental health and addiction treatment that was covered by his health plan. After nearly two dozen calls to the insurer and multiple hospitalizations, he couldn’t find a therapist. Last spring, he died, likely due to complications from excessive drinking.
Health insurance experts said that, unless agencies can crack down and issue bigger fines, insurers will keep selling error-ridden plans.
“You can have all the strong laws on the books,” said David Lloyd, chief policy officer with the mental health advocacy group Inseparable. “But if they’re not being enforced, then it’s kind of all for nothing.”
The problem with ghost networks isn’t one of awareness. States, federal agencies, researchers and advocates have documented them time and again for years. But regulators have resisted penalizing insurers for not fixing them.
Two years ago, the Arizona Department of Insurance and Financial Institutions began to probe the directories used by five large insurers for plans that they sold on the individual market. Regulators wanted to find out if they could schedule an appointment with mental health providers listed as accepting new patients, so their staff called 580 providers in those companies’ directories.
Thirty-seven percent of the calls did not lead to an appointment getting scheduled.
Even though this secret-shopper survey found errors at a lower rate than what had been found in New York, health insurance experts who reviewed Arizona’s published findings said that the results were still concerning.
Ghost network regulations are intended to keep provider listings as close to error-free as possible. While the experts don’t expect any insurer to have a perfect directory, they said that double-digit error rates can be harmful to customers.
Arizona’s regulators seemed to agree. In a January 2023 report, they wrote that a patient could be clinging to the “last few threads of hope, which could erode if they receive no response from a provider (or cannot easily make an appointment).”
Secret-shopper surveys are considered one of the best ways to unmask errors. But states have limited funding, which restricts how often they can conduct that sort of investigation. Michigan, for its part, mostly searches for inaccuracies as part of an annual review of a health plan. Nevada investigates errors primarily if someone files a complaint. Christine Khaikin, a senior health policy attorney for the nonprofit advocacy group Legal Action Center, said fewer surveys means higher odds that errors go undetected.
Some regulators, upon learning that insurers may not be following the law, still take a hands-off approach with their enforcement. Oregon’s Department of Consumer and Business Services, for instance, conducts spot checks of provider networks to see if those listings are accurate. If they find errors, insurers are asked to fix the problem. The department hasn’t issued a fine for directory errors since 2019. A spokesperson said the agency doesn’t keep track of how frequently it finds network directory errors.
Dave Jones, a former insurance commissioner in California, said some commissioners fear that stricter enforcement could drive companies out of their states, leaving their constituents with fewer plans to choose from.
Even so, staffers at the Arizona Department of Insurance and Financial Institutions wrote in the report that there “needs to be accountability from insurers” for the errors in their directories. That never happened, and the agency concealed the identities of the companies in the report. A department spokesperson declined to provide the insurers’ names to ProPublica and did not answer questions about the report.
Since January 2023, Arizonans have submitted dozens of complaints to the department that were related to provider networks. The spokesperson would not say how many were found to be substantiated, but the department was able to get insurers to address some of the problems, documents obtained through an open records request show.
According to the department’s online database of enforcement actions, not a single one of those companies has been fined.
Sometimes, when state insurance regulators fail to act, attorneys general or federal regulators intervene in their stead. But even then, the extra enforcers haven’t addressed the underlying problem.
For years, the Massachusetts Division of Insurance didn’t fine any company for ghost networks, so the state attorney general’s office began to investigate whether insurers had deceived consumers by publishing inaccurate directories. Among the errors identified: One plan had providers listed as accepting new patients but no actual appointments were available for months; another listed a single provider more than 10 times at different offices.
In February 2020, Maura Healey, who was then the Massachusetts attorney general, announced settlements with some of the state’s largest health plans. No insurer admitted wrongdoing. The companies, which together collect billions in premiums each year, paid a total of $910,000. They promised to remove providers who left their networks within 30 days of learning about that decision. Healey declared that the settlements would lead to “unprecedented changes to help ensure patients don’t have to struggle to find behavioral health services.”
But experts who reviewed the settlements for ProPublica identified a critical shortcoming. While the insurers had promised to audit directories multiple times a year, the companies did not have to report those findings to the attorney general’s office. Spokespeople for Healey and the attorney general’s office declined to answer questions about the experts’ assessments of the settlements.
After the settlements were finalized, Healey became the governor of Massachusetts and has been responsible for overseeing the state’s insurance division since she took office in January 2023. Her administration’s regulators haven’t brought any fines over ghost networks.
Healey’s spokesperson declined to answer questions and referred ProPublica to responses from the state’s insurance division. A division spokesperson said the state has taken steps to strengthen its provider directory regulations and streamline how information about in-network providers gets collected. Starting next year, the spokesperson said that the division “will consider penalties” against any insurer whose “provider directory is found to be materially noncompliant.”
States that don’t have ghost network laws have seen federal regulators step in to monitor directory errors.
In late 2020, Congress passed the No Surprises Act, which aimed to cut down on the prevalence of surprise medical bills from providers outside of a patient’s insurance network. Since then, the Centers for Medicare and Medicaid Services, which oversees the two large public health insurance programs, has reached out to every state to see which ones could handle enforcement of the federal ghost network regulations.
At least 15 states responded that they lacked the ability to enforce the new regulation. So CMS is now tasked with watching out for errors in directories used by millions of insurance customers in those states.
Julie Brookhart, a spokesperson for CMS, told ProPublica that the agency takes enforcement of the directory error regulations “very seriously.” She said CMS has received a “small number” of provider directory complaints, which the agency is in the process of investigating. If it finds a violation, Brookhart said regulators “will take appropriate enforcement action.”
But since the requirement went into effect in January 2022, CMS hasn’t fined any insurer for errors. Brookhart said that CMS intends to develop further guidelines with other federal agencies. Until that happens, Brookhart said that insurers are expected to make “good-faith” attempts to follow the federal provider directory rules.
Last year, five California lawmakers proposed a bill that sought to get rid of ghost networks around the state. If it passed, AB 236 would limit the number of errors allowed in a directory — creating a cap of 5% of all providers listed — and raise penalties for violations. California would become home to one of the nation’s toughest ghost network regulations.
The state had already passed one of America’s first such regulations in 2015, requiring insurers to post directories online and correct inaccuracies on a weekly basis.
Since the law went into effect in 2016, insurance customers have filed hundreds of complaints with the California Department of Managed Health Care, which oversees health plans for nearly 30 million enrollees statewide.
Lawyers also have uncovered extensive evidence of directory errors. When San Diego’s city attorney, Mara Elliott, sued several insurers over publishing inaccurate directories in 2021, she based the claims on directory error data collected by the companies themselves. Citing that data, the lawsuits noted that error rates for the insurers’ psychiatrist listings were between 26% and 83% in 2018 and 2019. The insurers denied the accusations and convinced a judge to dismiss the suits on technical grounds. A panel of California appeals court judges recently reversed those decisions; the cases are pending.
The companies have continued to send that data to the DMHC each year — but the state has not used it to examine ghost networks. California is among the states that typically waits for a complaint to be filed before it investigates errors.
“The industry doesn’t take the regulatory penalties seriously because they’re so low,” Elliott told ProPublica. “It’s probably worth it to take the risk and see if they get caught.”
California’s limited enforcement has resulted in limited fines. Over the past eight years, the DMHC has issued just $82,500 in fines for directory errors involving providers of any kind. That’s less than one-fifth of the fines issued in the two years before the regulation went into effect.
A spokesperson for the DMHC said its regulators continue “to hold health plans accountable” for violating ghost network regulations. Since 2018, the DMHC has discovered scores of problems with provider directories and pushed health plans to correct the errors. The spokesperson said that the department’s oversight has also helped some customers get reimbursed for out-of-network costs incurred due to directory errors.
“A lower fine total does not equate to a scaling back on enforcement,” the spokesperson said.
Dr. Joaquin Arambula, one of the state Assembly members who co-sponsored AB 236, disagreed. He told ProPublica that California’s current ghost network regulation is “not effectively being enforced.” After clearing the state Assembly this past winter, his bill, along with several others that address mental health issues, was suddenly tabled this summer. The roadblock came from a surprising source: the administration of the state’s Democratic governor.
Officials with the DMHC, whose director was appointed by Gov. Gavin Newsom, estimated that more than $15 million in extra funding would be needed to carry out the bill’s requirements over the next five years. State lawmakers accused officials of inflating the costs. The DMHC’s spokesperson said that the estimate was accurate and based on the department’s “real experience” overseeing health plans.
Arambula and his co-sponsors hope that their colleagues will reconsider the measure during next year’s session. Sitting before state lawmakers in Sacramento this year, a therapist named Sarah Soroken told the story of a patient who had called 50 mental health providers in her insurer’s directory. None of them could see her. Only after the patient attempted suicide did she get the care she’d sought.
“We would be negligent,” Soroken told the lawmakers, “if we didn’t do everything in our power to ensure patients get the health care they need.”
Paige Pfleger of WPLN/Nashville Public Radio contributed reporting.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Case of the Armadillo: Is It Spreading Leprosy in Florida?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
GAINESVILLE, Fla. — In an open-air barn at the edge of the University of Florida, veterinarian Juan Campos Krauer examines a dead armadillo’s footpads and ears for signs of infection.
Its claws are curled tight and covered in blood. Campos Krauer thinks it was struck in the head while crossing a nearby road.
He then runs a scalpel down its underside. He removes all the important organs: heart, liver, kidneys. Once the specimens are bottled up, they’re destined for an ultra-cold freezer in his lab at the college.
Campos Krauer plans to test the armadillo for leprosy, an ancient illness also known as Hansen’s disease that can lead to nerve damage and disfigurement in humans. He and other scientists are trying to solve a medical mystery: why Central Florida has become a hot spot for the age-old bacteria that cause it.
Leprosy remains rare in the United States. But Florida, which often reports the most cases of any state, has seen an uptick in patients. The epicenter is east of Orlando. Brevard County reported a staggering 13% of the nation’s 159 leprosy cases in 2020, according to a Tampa Bay Times analysis of state and federal data.
Many questions about the phenomenon remain unanswered. But leprosy experts believe armadillos play a role in spreading the illness to people. To better understand who’s at risk and to prevent infections, about 10 scientists teamed up last year to investigate. The group includes researchers from the University of Florida, Colorado State University, and Emory University in Atlanta.
“How this transmission is happening, we really don’t know,” said Ramanuj Lahiri, chief of the laboratory research branch for the National Hansen’s Disease Program, which studies the bacteria involved and cares for leprosy patients across the country.
‘Nothing Was Adding Up’
Leprosy is believed to be the oldest human infection in history. It probably has been sickening people for at least 100,000 years. The disease is highly stigmatized — in the Bible, it was described as a punishment for sin. In more modern times, patients were isolated in “colonies” around the world, including in Hawaii and Louisiana.
In mild cases, the slow-growing bacteria cause a few lesions. If left untreated, they can paralyze the hands and feet.
But it’s actually difficult to fall ill with leprosy, as the infection isn’t very contagious. Antibiotics can cure the ailment in a year or two. They’re available for free through the federal government and the World Health Organization, which launched a campaign in the 1990s to eliminate leprosy as a public health problem.
In 2000, reported U.S. cases dropped to their lowest point in decades with 77 infections. But they later increased, averaging about 180 per year from 2011 to 2020, according to data from the National Hansen’s Disease Program.
During that time, a curious trend emerged in Florida.
In the first decade of the 21st century, the state logged 67 cases. Miami-Dade County noted 20 infections — the most of any Florida county. The vast majority of its cases were acquired outside the U.S., according to a Times analysis of Florida Department of Health data.
But over the next 10 years, recorded cases in the state more than doubled to 176 as Brevard County took center stage.
The county, whose population is about a fifth the size of Miami-Dade’s, logged 85 infections during that time — by far the most of any county in the state and nearly half of all Florida cases. In the previous decade, Brevard noted just five cases.
Remarkably, at least a quarter of Brevard’s infections were acquired within the state, not while the individuals were abroad. India, Brazil, and Indonesia diagnose more leprosy cases than anywhere, reporting over 135,000 infections combined in 2022 alone. People were getting sick even though they hadn’t traveled to such areas or been in close contact with existing leprosy patients, said Barry Inman, a former epidemiologist at the Brevard health department who investigated the cases and retired in 2021.
“Nothing was adding up,” Inman said.
A few patients recalled touching armadillos, which are known to carry the bacteria. But most didn’t, he said. Many spent a lot of time outdoors, including lawn workers and avid gardeners. The cases were usually mild.
It was difficult to nail down where people got the illness, he added. Because the bacteria grow so slowly, it can take anywhere from nine months to 20 years for symptoms to begin.
Amoeba or Insect Culprits?
Heightened awareness of leprosy could play a role in Brevard’s groundswell of cases.
Doctors must report leprosy to the health department. Yet Inman said many in the county didn’t know that, so he tried to educate them after noticing cases in the late 2000s.
But that’s not the sole factor at play, Inman said.
“I don’t think there’s any doubt in my mind that something new is going on,” he said.
Other parts of Central Florida have also recorded more infections. From 2011 to 2020, Polk County logged 12 cases, tripling its numbers compared with the previous 10 years. Volusia County noted 10 cases. It reported none the prior decade.
Scientists are honing in on armadillos. They suspect the burrowing critters may indirectly cause infections through soil contamination.
Armadillos, which are protected by hard shells, serve as good hosts for the bacteria, which don’t like heat and can thrive in the animals whose body temperatures range from a cool 86-95 degrees.
Colonists probably brought the disease to the New World hundreds of years ago, and somehow armadillos became infected, said Lahiri, the National Hansen’s Disease Program scientist. The nocturnal mammals can develop lesions from the illness just as humans can. More than 1 million armadillos occupy Florida, estimated Campos Krauer, an assistant professor in the University of Florida’s Department of Large Animal Clinical Sciences.
How many carry leprosy is unclear. A study published in 2015 of more than 600 armadillos in Alabama, Florida, Georgia, and Mississippi found that about 16% showed evidence of infection. Public health experts believe leprosy was previously confined to armadillos west of the Mississippi River, then spread east.
Handling the critters is a known hazard. Lab research shows that single-cell amoebas, which live in soil, can also carry the bacteria.
Armadillos love to dig up and eat earthworms, frustrating homeowners whose yards they damage. The animals may shed the bacteria while hunting for food, passing it to amoebas, which could later infect people.
Leprosy experts also wonder if insects help spread the disease. Blood-sucking ticks might be a culprit, lab research shows.
“Some people who are infected have little to no exposure to the armadillo,” said Norman Beatty, an assistant professor of medicine at the University of Florida. “There is likely another source of transmission in the environment.”
Campos Krauer, who’s been searching Gainesville streets for armadillo roadkill, wants to gather infected animals and let them decompose in a fenced-off area, allowing the remains to soak into a tray of soil while flies lay eggs. He hopes to test the dirt and larvae to see if they pick up the bacteria.
Adding to the intrigue is a leprosy strain found only in Florida, according to scientists.
In the 2015 study, researchers discovered that seven armadillos from the Merritt Island National Wildlife Refuge, which is mostly in Brevard but crosses into Volusia, carried a previously unseen version of the pathogen.
Ten patients in the region were stricken with it, too. At the genetic level, the strain is similar to another type found in U.S. armadillos, said Charlotte Avanzi, a Colorado State University researcher who specializes in leprosy.
It’s unknown if the strain causes more severe disease, Lahiri said.
Reducing Risk
The public should not panic about leprosy, nor should people race to euthanize armadillos, researchers warn.
Scientists estimate that over 95% of the global human population has a natural ability to ward off the disease. They believe months of exposure to respiratory droplets is needed for person-to-person transmission to occur.
But when infections do happen, they can be devastating.
“If we better understand it,” Campos Krauer said, “the better we can learn to live with it and reduce the risk.”
The new research may also provide insight for other Southern states. Armadillos, which don’t hibernate, have been moving north, Campos Krauer said, reaching areas like Indiana and Virginia. They could go farther due to climate change.
People concerned about leprosy can take simple precautions, medical experts say. Those working in dirt should wear gloves and wash their hands afterward. Raising garden beds or surrounding them with a fence may limit the chances of soil contamination. If digging up an armadillo burrow, consider wearing a face mask, Campos Krauer said.
Don’t play with or eat the animals, added John Spencer, a scientist at Colorado State University who studies leprosy transmission in Brazil. They’re legal to hunt year-round in Florida without a license.
Campos Krauer’s team has so far examined 16 dead armadillos found on Gainesville area roads, more than 100 miles from the state’s leprosy epicenter, trying to get a preliminary idea of how many carry the bacteria.
None has tested positive yet.
This article was produced through a partnership between KFF Health News and the Tampa Bay Times.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Surgery is the default treatment for ACL injuries in Australia. But it’s not the only way
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
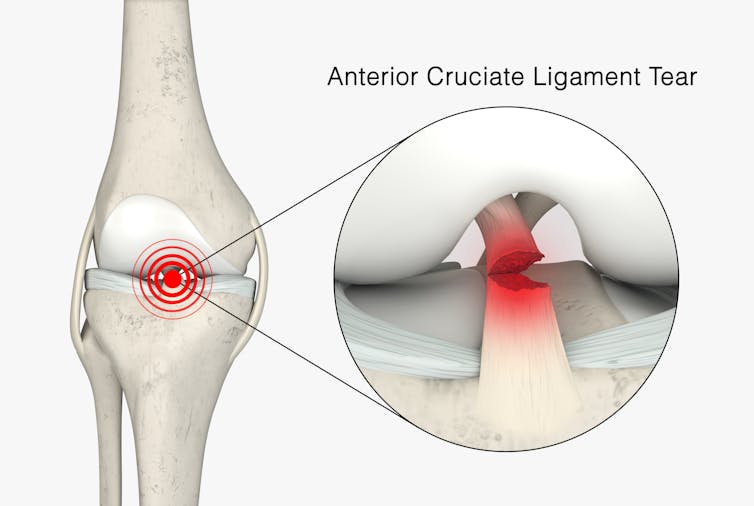
The anterior cruciate ligament (ACL) is an important ligament in the knee. It runs from the thigh bone (femur) to the shin bone (tibia) and helps stabilise the knee joint.
Injuries to the ACL, often called a “tear” or a “rupture”, are common in sport. While a ruptured ACL has just sidelined another Matildas star, people who play sport recreationally are also at risk of this injury.
For decades, surgical repair of an ACL injury, called a reconstruction, has been the primary treatment in Australia. In fact, Australia has among the highest rates of ACL surgery in the world. Reports indicate 90% of people who rupture their ACL go under the knife.
Although surgery is common – around one million are performed worldwide each year – and seems to be the default treatment for ACL injuries in Australia, it may not be required for everyone.
PeopleImages.com – Yuri A/Shutterstock What does the research say?
We know ACL ruptures can be treated using reconstructive surgery, but research continues to suggest they can also be treated with rehabilitation alone for many people.
Almost 15 years ago a randomised clinical trial published in the New England Journal of Medicine compared early surgery to rehabilitation with the option of delayed surgery in young active adults with an ACL injury. Over half of people in the rehabilitation group did not end up having surgery. After five years, knee function did not differ between treatment groups.
The findings of this initial trial have been supported by more research since. A review of three trials published in 2022 found delaying surgery and trialling rehabilitation leads to similar outcomes to early surgery.
A 2023 study followed up patients who received rehabilitation without surgery. It showed one in three had evidence of ACL healing on an MRI after two years. There was also evidence of improved knee-related quality of life in those with signs of ACL healing compared to those whose ACL did not show signs of healing.
Experts used to think an ACL tear couldn’t heal without surgery – now there’s evidence it can. SKYKIDKID/Shutterstock Regardless of treatment choice the rehabilitation process following ACL rupture is lengthy. It usually involves a minimum of nine months of progressive rehabilitation performed a few days per week. The length of time for rehabilitation may be slightly shorter in those not undergoing surgery, but more research is needed in this area.
Rehabilitation starts with a physiotherapist overseeing simple exercises right through to resistance exercises and dynamic movements such as jumping, hopping and agility drills.
A person can start rehabilitation with the option of having surgery later if the knee remains unstable. A common sign of instability is the knee giving way when changing direction while running or playing sports.
To rehab and wait, or to go straight under the knife?
There are a number of reasons patients and clinicians may opt for early surgical reconstruction.
For elite athletes, a key consideration is returning to sport as soon as possible. As surgery is a well established method, athletes (such as Matilda Sam Kerr) often opt for early surgical reconstruction as this gives them a more predictable timeline for recovery.
At the same time, there are risks to consider when rushing back to sport after ACL reconstruction. Re-injury of the ACL is very common. For every month return to sport is delayed until nine months after ACL reconstruction, the rate of knee re-injury is reduced by 51%.
For people who opt to try rehabilitation, the option of having surgery later is still there. PeopleImages.com – Yuri A/Shutterstock Historically, another reason for having early surgical reconstruction was to reduce the risk of future knee osteoarthritis, which increases following an ACL injury. But a review showed ACL reconstruction doesn’t reduce the risk of knee osteoarthritis in the long term compared with non-surgical treatment.
That said, there’s a need for more high-quality, long-term studies to give us a better understanding of how knee osteoarthritis risk is influenced by different treatments.
Rehab may not be the only non-surgical option
Last year, a study looking at 80 people fitted with a specialised knee brace for 12 weeks found 90% had evidence of ACL healing on their follow-up MRI.
People with more ACL healing on the three-month MRI reported better outcomes at 12 months, including higher rates of returning to their pre-injury level of sport and better knee function. Although promising, we now need comparative research to evaluate whether this method can achieve similar results to surgery.
What to do if you rupture your ACL
First, it’s important to seek a comprehensive medical assessment from either a sports physiotherapist, sports physician or orthopaedic surgeon. ACL injuries can also have associated injuries to surrounding ligaments and cartilage which may influence treatment decisions.
In terms of treatment, discuss with your clinician the pros and cons of management options and whether surgery is necessary. Often, patients don’t know not having surgery is an option.
Surgery appears to be necessary for some people to achieve a stable knee. But it may not be necessary in every case, so many patients may wish to try rehabilitation in the first instance where appropriate.
As always, prevention is key. Research has shown more than half of ACL injuries can be prevented by incorporating prevention strategies. This involves performing specific exercises to strengthen muscles in the legs, and improve movement control and landing technique.
Anthony Nasser, Senior Lecturer in Physiotherapy, University of Technology Sydney; Joshua Pate, Senior Lecturer in Physiotherapy, University of Technology Sydney, and Peter Stubbs, Senior Lecturer in Physiotherapy, University of Technology Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Aspirin vs Cancer Metastasis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aspirin is a bit of a mixed bag.
In the category of things in its favor, it’s a modest analgesic with few side effects from occasional use, so it’s a good option if you have a headache, for example.
Unless you’re already on blood thinners or having a bleeding disorder, in which case, aspirin is not the thing to reach for.
About aspirin and heart disease
This is actually a complicated one, and we covered it at length in a dedicated main feature. If you want a one-line summary, it’s “chronic low-dose aspirin use can lower overall CVD risk, but does not reduce CVD mortality or all-cause mortality, and you may pay for it with gastrointestinal bleeding, and increased risk of ulcers“.
For a more nuanced explanation, see: Aspirin, CVD Risk, & Potential Counter-Risks
On the other hand, if you are having a heart attack and are waiting for the ambulance that you already called, and have aspirin to hand that you don’t have to go looking for, then it can be good to take a dose then.
For more on that, see: How To Survive A Heart Attack When You’re Alone
There are more problems
In the case of chronic use of low-dose aspirin, not only does it increase the risks of bleeding, especially gastrointestinal bleeding, and ulcers, but also it increases the risk of anemia. Given that anemia also gives the symptom “dizziness”, this is also a significant threat for increasing the incidence of falls in the older population, too, which can of course lead to serious complications and ultimately death.
For the science about this, see: Low-Dose Aspirin & Anemia
Now, about aspirin and cancer metastasis
This one’s a point in aspirin’s favor.
Cancer is, in and of itself, obviously a big problem. In terms of when it’s most likely to kill someone, that is usually when the cancer becomes metastatic, that is to say, it has spread.
So, while preventing cancer and, failing that, killing cancer are very important goals, there is a third axis to cancer care, which is preventing metastasis in someone who has cancer.
And that’s what aspirin does. How, you ask?
Scientists found this one out by accident!
They were doing genetic research in mice, to find genes that had an effect on metastasis. In the process, they found a certain gene that instructs the creation of a certain protein, and mice that lacked that gene (and thus its associated protein) had less metastasis.
The protein in question suppresses T-cells, which are programmed to recognize and kill metastatic cancer cells (amongst having other great jobs; they are an important part of the immune system in general, and one that declines with aging; most people in their 60s or older are producing very few T-cells).
About that, see: Focusing On Health In Our Sixties
Tracing the cell signaling, the researchers found that the protein is activated when T-cells are exposed to thromboxane A2 (or TXA2 to its friends).
And TXA2? That’s produced by platelets, and aspirin works by inhibiting TXA2 production, effectively making platelets (and thus the blood as a whole) less sticky.
So, that’s quite a few steps in the process, but ultimately:
- Aspirin inhibits TXA2 production
- Lower TXA2 levels mean ARHGEF1 (that’s the protein) isn’t activated
- ARHGEF1 not being activated means T-cells are free to do their thing
- T-cells are now free to kill metastatic cancer cells
You can read the paper here:
Aspirin prevents metastasis by limiting platelet TXA2 suppression of T cell immunity
Take care!
Share This Post
Related Posts
-
7 Healthy Gut Habits For Women Over 40 – by Lara West
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With regard to the titular 7 healthy gut habits for women over 40, a chapter is devoted to each one of those habits, and she goes into quite some detail in each category, more than you might expect.
As for the 7 things, we’ll not keep them a mystery; they are:
- Intermittent fasting
- Prebiotics & probiotics
- Mindful eating
- Understanding ingredients
- Movement
- Sleep
- Stress management
Of course, all of these things are good regardless of one’s age or gender, but West is writing with women over 40 in mind, and as such, she will focus on things that are especially relevant to those of us who are indeed women over 40.
You may be wondering: what if I’m a long way over 40, and menopause is a distant memory? In that case, 90% of this will still be relevant to you; the only parts that won’t be, are those that pertain specifically to the menopausal transitional phase itself, rather than the post-menopause state.
You may also be wondering: what if I’m a man, and menopause is just not in the cards for me? In that case, maybe about 70% of this will still be relevant to you, because of the broad applicability of most of the advice. That said, if it’s just for yourself, you’d probably do better with a book of which 100% is relevant to you, rather than this one.
The style is conversational pop-science, with personal anecdotes mixed in with references to science. It’s definitely on the light/easy-reading end of books that we’ve reviewed on the topic.
Bottom line: if you’re a woman over 40 who would like to improve your gut health, this book was written for you.
Click here to check out 7 Healthy Gut Habits For Women Over 40, and rediscover vitality!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Walnuts vs Cashews – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing walnuts to cashews, we picked the walnuts.
Why?
It was close! In terms of macros, walnuts have about 2x the fiber, while cashews have slightly more protein. In the specific category of fats, walnuts have more fat. Looking further into it: walnuts’ fats are mostly polyunsaturated, while cashews’ fats are mostly monounsaturated, both of which are considered healthy.
Notwithstanding being both high in calories, neither nut is associated with weight gain—largely because of their low glycemic indices (of which, walnuts enjoy the slightly lower GI, but both are low-GI foods)
When it comes to vitamins, walnuts have more of vitamins A, B2, B3 B6, B9, and C, while cashews have more of vitamins B1, B5, E, and K. Because of the variation in their respective margins of difference, this is at best a moderate victory for walnuts, though.
In the category of minerals, cashews get their day, as walnuts have more calcium and manganese, while cashews have more copper, iron, magnesium, phosphorus, potassium, selenium, and zinc.
In short: unless you’re allergic, we recommend enjoying both of these nuts (and others) for a full range of benefits. However, if you’re going to pick one, walnuts win the day.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Radiant Rebellion – by Karen Walrond
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In health terms, we are often about fighting aging here. But to be more specific, what we’re fighting in those cases is not truly aging itself, so much as age-related decline.
Karen Walrond makes a case that we’ve made from the very start of 10almonds (but she wrote a whole book about it), that there’s merit in looking at what we can and can’t control about aging, doing what we reasonably can, and embracing what we can’t.
And yes, embracing, not merely accepting. This is not a downer of a book; it’s a call to revolution. It asks us to be proud of our grey hairs, to see our smile-lines around our eyes as the sign of a lived-in body, and even to embrace some of the unavoidable “actual decline” things as part of the journey of life. Maybe we’re not as strong as we used to be and now need a grippety-doodah to open jars; not everyone gets to live long enough to experience that! How lucky we are.
Perhaps most importantly, she bids us be the change we want to see in the world, and inspire others with our choices and actions, and shake off ageist biases for good.
Bottom line: if you want to foster a better attitude to aging not only for yourself, but also those around you, then this is a top-tier book for that.
Click here to check out Radiant Rebellion, and reclaim aging!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: