How light can shift your mood and mental health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is the next article in our ‘Light and health’ series, where we look at how light affects our physical and mental health in sometimes surprising ways. Read other articles in the series.
It’s spring and you’ve probably noticed a change in when the Sun rises and sets. But have you also noticed a change in your mood?
We’ve known for a while that light plays a role in our wellbeing. Many of us tend to feel more positive when spring returns.
But for others, big changes in light, such as at the start of spring, can be tough. And for many, bright light at night can be a problem. Here’s what’s going on.

An ancient rhythm of light and mood
In an earlier article in our series, we learned that light shining on the back of the eye sends “timing signals” to the brain and the master clock of the circadian system. This clock coordinates our daily (circadian) rhythms.
“Clock genes” also regulate circadian rhythms. These genes control the timing of when many other genes turn on and off during the 24-hour, light-dark cycle.
But how is this all linked with our mood and mental health?
Circadian rhythms can be disrupted. This can happen if there are problems with how the body clock develops or functions, or if someone is routinely exposed to bright light at night.
When circadian disruption happens, it increases the risk of certain mental disorders. These include bipolar disorder and atypical depression (a type of depression when someone is extra sleepy and has problems with their energy and metabolism).
Light on the brain
Light may also affect circuits in the brain that control mood, as animal studies show.
There’s evidence this happens in humans. A brain-imaging study showed exposure to bright light in the daytime while inside the scanner changed the activity of a brain region involved in mood and alertness.
Another brain-imaging study found a link between daily exposure to sunlight and how the neurotransmitter (or chemical messenger) serotonin binds to receptors in the brain. We see alterations in serotonin binding in several mental disorders, including depression.

What happens when the seasons change?
Light can also affect mood and mental health as the seasons change. During autumn and winter, symptoms such as low mood and fatigue can develop. But often, once spring and summer come round, these symptoms go away. This is called “seasonality” or, when severe, “seasonal affective disorder”.
What is less well known is that for other people, the change to spring and summer (when there is more light) can also come with a change in mood and mental health. Some people experience increases in energy and the drive to be active. This is positive for some but can be seriously destabilising for others. This too is an example of seasonality.
Most people aren’t very seasonal. But for those who are, seasonality has a genetic component. Relatives of people with seasonal affective disorder are more likely to also experience seasonality.
Seasonality is also more common in conditions such as bipolar disorder. For many people with such conditions, the shift into shorter day-lengths during winter can trigger a depressive episode.
Counterintuitively, the longer day-lengths in spring and summer can also destabilise people with bipolar disorder into an “activated” state where energy and activity are in overdrive, and symptoms are harder to manage. So, seasonality can be serious.
Alexis Hutcheon, who experiences seasonality and helped write this article, told us:
[…] the season change is like preparing for battle – I never know what’s coming, and I rarely come out unscathed. I’ve experienced both hypomanic and depressive episodes triggered by the season change, but regardless of whether I’m on the ‘up’ or the ‘down’, the one constant is that I can’t sleep. To manage, I try to stick to a strict routine, tweak medication, maximise my exposure to light, and always stay tuned in to those subtle shifts in mood. It’s a time of heightened awareness and trying to stay one step ahead.
So what’s going on in the brain?
One explanation for what’s going on in the brain when mental health fluctuates with the change in seasons relates to the neurotransmitters serotonin and dopamine.
Serotonin helps regulate mood and is the target of many antidepressants. There is some evidence of seasonal changes in serotonin levels, potentially being lower in winter.
Dopamine is a neurotransmitter involved in reward, motivation and movement, and is also a target of some antidepressants. Levels of dopamine may also change with the seasons.
But the neuroscience of seasonality is a developing area and more research is needed to know what’s going on in the brain.
How about bright light at night?
We know exposure to bright light at night (for instance, if someone is up all night) can disturb someone’s circadian rhythms.
This type of circadian rhythm disturbance is associated with higher rates of symptoms including self-harm, depressive and anxiety symptoms, and lower wellbeing. It is also associated with higher rates of mental disorders, such as major depression, bipolar disorder, psychotic disorders and post-traumatic stress disorder (or PTSD).
Why is this? Bright light at night confuses and destabilises the body clock. It disrupts the rhythmic regulation of mood, cognition, appetite, metabolism and many other mental processes.
But people differ hugely in their sensitivity to light. While still a hypothesis, people who are most sensitive to light may be the most vulnerable to body clock disturbances caused by bright light at night, which then leads to a higher risk of mental health problems.

Where to from here?
Learning about light will help people better manage their mental health conditions.
By encouraging people to better align their lives to the light-dark cycle (to stabilise their body clock) we may also help prevent conditions such as depression and bipolar disorder emerging in the first place.
Healthy light behaviours – avoiding light at night and seeking light during the day – are good for everyone. But they might be especially helpful for people at risk of mental health problems. These include people with a family history of mental health problems or people who are night owls (late sleepers and late risers), who are more at risk of body clock disturbances.
Alexis Hutcheon has lived experience of a mental health condition and helped write this article.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Jacob Crouse, Research Fellow in Youth Mental Health, Brain and Mind Centre, University of Sydney; Emiliana Tonini, Postdoctoral Research Fellow, Brain and Mind Centre, University of Sydney, and Ian Hickie, Co-Director, Health and Policy, Brain and Mind Centre, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dates vs Prunes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to prunes, we picked the prunes.
Why?
First let’s note: we’re listing the second fruit here as “prunes” rather than “plums”, since prunes are dehydrated plums, and it makes more sense to compare the dried fruit to dates which are invariably dried too. Otherwise, the water weight of plums would unfairly throw out the nutrient proportions per 100g (indeed, upon looking up numbers, dates would overwhelmingly beat plums easily in the category of pretty much every nutrient).
So let’s look at the fairer comparison:
In terms of macros, dates have a little more protein, carbohydrate, and fiber. This is because while both are dried, prunes are usually sold with more water remaining than dates; indeed, per 100g prunes still have 30g water weight to dates’ 20g water weight. This makes everything close, but we are going to call this category a nominal win for dates. Mind you, hydration is still good, but please do not rely on dried fruit for your hydration!
When it comes to vitamins, dates have more of vitamins B5 and B9, while prunes have more of vitamins A, B2, B3, B6, C, E, K, and choline. A clear win for prunes here.
In the category of minerals, it’s a similar story: dates have more iron, magnesium, and selenium, while prunes have more calcium, copper, manganese, phosphorus, potassium, and zinc. Another win for prunes.
In short, enjoy either or both, but prunes win on overall nutritional density!
Want to learn more?
You might like to read:
From Apples to Bees, and High-Fructose Cs: Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Share This Post
-
Three Daily Servings of Beans?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Not crazy about the Dr.s food advice. Beans 3X a day?❞
For reference, this is in response to our recent article on the topic of 12 things to aim to get a certain amount of each day:
So, there are a couple of things to look at here:
Firstly, don’t worry, it’s a guideline and an aim. If you don’t hit it on a given day, there is always tomorrow. It’s just good to know what one is aiming for, because without knowing that, achieving it will be a lot less likely!
Secondly, the beans/legumes/pulses category says three servings, but the example serving sizes are quite small, e.g. ½ cup cooked beans, or ¼ cup hummus. And also as you notice, dips/pastes/sauces made from beans count too. So given the portion sizes, you could easily get two servings in by breakfast (and two servings of whole grains, too) if you enjoy frijoles refritos, for example. Many of the recipes we share on this site have “stealth” beans/legumes/pulses in this fashion
Take care!
Share This Post
-
6 Signs Of A Heart Attack… A Month In Advance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many people know the signs of a heart attack when it’s happening, but how about before it’s too late to avoid it?
The signs
- Unusual fatigue: persistent tiredness that doesn’t improve with rest
- Shortness of breath: unexplained breathlessness during light activities or rest, which can be caused by fluid buildup in the lungs (because the heart isn’t circulating blood as well as it should)
- Chest discomfort: pain, pressure, tightness, or aching in the chest due to reduced blood flow to the heart muscle—often occurring during physical exertion or emotional stress
- Frequent indigestion: means that heartburn could be heart-related! This is about persistently reoccurring discomfort or pain in the upper abdomen
- Sleep disturbances: difficulties falling asleep, staying asleep, or waking up abruptly
- Excessive sweating: unexplained cold sweats or sudden sweating without physical exertion or excessive heat, can be a response to the decreased oxygen levels caused by less efficient blood flow
Note: this is a list of warning signs, not a diagnostic tool. Any or even all of these could be caused by something else. Just, don’t ignore the signs and do get yourself checked out.
For more details on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
Related Posts
-
What is type 1.5 diabetes? It’s a bit like type 1 and a bit like type 2 – but it’s often misdiagnosed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While you’re likely familiar with type 1 and type 2 diabetes, you’ve probably heard less about type 1.5 diabetes.
Also known as latent autoimmune diabetes in adults (LADA), type 1.5 diabetes has features of both type 1 and type 2 diabetes.
More people became aware of this condition after Lance Bass, best known for his role in the iconic American pop band NSYNC, recently revealed he has it.
So, what is type 1.5 diabetes? And how is it diagnosed and treated?
Pixel-Shot/Shutterstock There are several types of diabetes
Diabetes mellitus is a group of conditions that arise when the levels of glucose (sugar) in our blood are higher than normal. There are actually more than ten types of diabetes, but the most common are type 1 and type 2.
Type 1 diabetes is an autoimmune condition where the body’s immune system attacks and destroys the cells in the pancreas that make the hormone insulin. This leads to very little or no insulin production.
Insulin is important for moving glucose from the blood into our cells to be used for energy, which is why people with type 1 diabetes need insulin medication daily. Type 1 diabetes usually appears in children or young adults.
Type 2 diabetes is not an autoimmune condition. Rather, it happens when the body’s cells become resistant to insulin over time, and the pancreas is no longer able to make enough insulin to overcome this resistance. Unlike type 1 diabetes, people with type 2 diabetes still produce some insulin.
Type 2 is more common in adults but is increasingly seen in children and young people. Management can include behavioural changes such as nutrition and physical activity, as well as oral medications and insulin therapy.
People with diabetes may need to regularly monitor their blood sugar levels. Dragana Gordic/Shutterstock How does type 1.5 diabetes differ from types 1 and 2?
Like type 1 diabetes, type 1.5 occurs when the immune system attacks the pancreas cells that make insulin. But people with type 1.5 often don’t need insulin immediately because their condition develops more slowly. Most people with type 1.5 diabetes will need to use insulin within five years of diagnosis, while those with type 1 typically require it from diagnosis.
Type 1.5 diabetes is usually diagnosed in people over 30, likely due to the slow progressing nature of the condition. This is older than the typical age for type 1 diabetes but younger than the usual diagnosis age for type 2.
Type 1.5 diabetes shares genetic and autoimmune risk factors with type 1 diabetes such as specific gene variants. However, evidence has also shown it may be influenced by lifestyle factors such as obesity and physical inactivity which are more commonly associated with type 2 diabetes.
What are the symptoms, and how is it treated?
The symptoms of type 1.5 diabetes are highly variable between people. Some have no symptoms at all. But generally, people may experience the following symptoms:
- increased thirst
- frequent urination
- fatigue
- blurred vision
- unintentional weight loss.
Typically, type 1.5 diabetes is initially treated with oral medications to keep blood glucose levels in normal range. Depending on their glucose control and the medication they are using, people with type 1.5 diabetes may need to monitor their blood glucose levels regularly throughout the day.
When average blood glucose levels increase beyond normal range even with oral medications, treatment may progress to insulin. However, there are no universally accepted management or treatment strategies for type 1.5 diabetes.
Type 1.5 diabetes might be managed with oral medications, at least initially. Dragana Gordic/Shutterstock Type 1.5 diabetes is often misdiagnosed
Lance Bass said he was initially diagnosed with type 2 diabetes, but later learned he actually has type 1.5 diabetes. This is not entirely uncommon. Estimates suggest type 1.5 diabetes is misdiagnosed as type 2 diabetes 5–10% of the time.
There are a few possible reasons for this.
First, accurately diagnosing type 1.5 diabetes, and distinguishing it from other types of diabetes, requires special antibody tests (a type of blood test) to detect autoimmune markers. Not all health-care professionals necessarily order these tests routinely, either due to cost concerns or because they may not consider them.
Second, type 1.5 diabetes is commonly found in adults, so doctors might wrongly assume a person has developed type 2 diabetes, which is more common in this age group (whereas type 1 diabetes usually affects children and young adults).
Third, people with type 1.5 diabetes often initially make enough insulin in the body to manage their blood glucose levels without needing to start insulin medication. This can make their condition appear like type 2 diabetes, where people also produce some insulin.
Finally, because type 1.5 diabetes has symptoms that are similar to type 2 diabetes, it may initially be treated as type 2.
We’re still learning about type 1.5
Compared with type 1 and type 2 diabetes, there has been much less research on how common type 1.5 diabetes is, especially in non-European populations. In 2023, it was estimated type 1.5 diabetes represented 8.9% of all diabetes cases, which is similar to type 1. However, we need more research to get accurate numbers.
Overall, there has been a limited awareness of type 1.5 diabetes and unclear diagnostic criteria which have slowed down our understanding of this condition.
A misdiagnosis can be stressful and confusing. For people with type 1.5 diabetes, being misdiagnosed with type 2 diabetes might mean they don’t get the insulin they need in a timely manner. This can lead to worsening health and a greater likelihood of complications down the road.
Getting the right diagnosis helps people receive the most appropriate treatment, save money, and reduce diabetes distress. If you’re experiencing symptoms you think may indicate diabetes, or feel unsure about a diagnosis you’ve already received, monitor your symptoms and chat with your doctor.
Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University and Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Signs That Are Present When Someone Is Dying
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You’ve probably been there a few times, although given the emotional nature of the thing, it’s likely that you weren’t taking notes. Hospice workers, on the other hand, do take notes, so here are some things you might want to know, and if anything makes the next time even a little easier, that’ll be good:
Last stages
Here are the discussed signs of the “active dying” phase:
- Increasing unconsciousness:
- The person will be mostly unresponsive most of the time.
- Eyes may be open or partially open but not making eye contact.
- Mouth will likely remain open due to muscle relaxation.
- Cessation of food and water intake
- The person will likely not eat or drink for several days.
- This is a natural process and does not cause suffering per se (e.g. thirst, hunger).
- Dryness of mouth, however, can be treated with a little moistening, for comfort.
- Changes in breathing
- Breathing patterns will change and may be irregular.
- This is a natural metabolic response, and is not a sign of distress.
- Terminal secretions (“death rattle”) may occur:
- A gurgling sound caused by saliva buildup due to loss of swallowing reflex.
- Not painful or distressing for the person.
- Can be managed by repositioning or using medication to dry secretions.
- Skin color changes / mottling:
- First appears on fingers and toes (purple or gray discoloration).
- May spread to knees, nose, or other extremities.
- Temperature fluctuations:
- The body loses its ability to regulate temperature.
- Person may feel hot but be cold (or vice versa).
- Fevers are common—cooling measures and/or Tylenol can help.
A person in discomfort may appear restless, have a furrowed brow, or show physical agitation. If on the other hand they appear peaceful and unresponsive, they are almost certainly not in distress. At such times, it’s best to focus on just keeping them clean and comfortable.
For more on all of these, see:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Managing Mortality: When Planning Is a Matter of Life and Death
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Increasing unconsciousness:
-
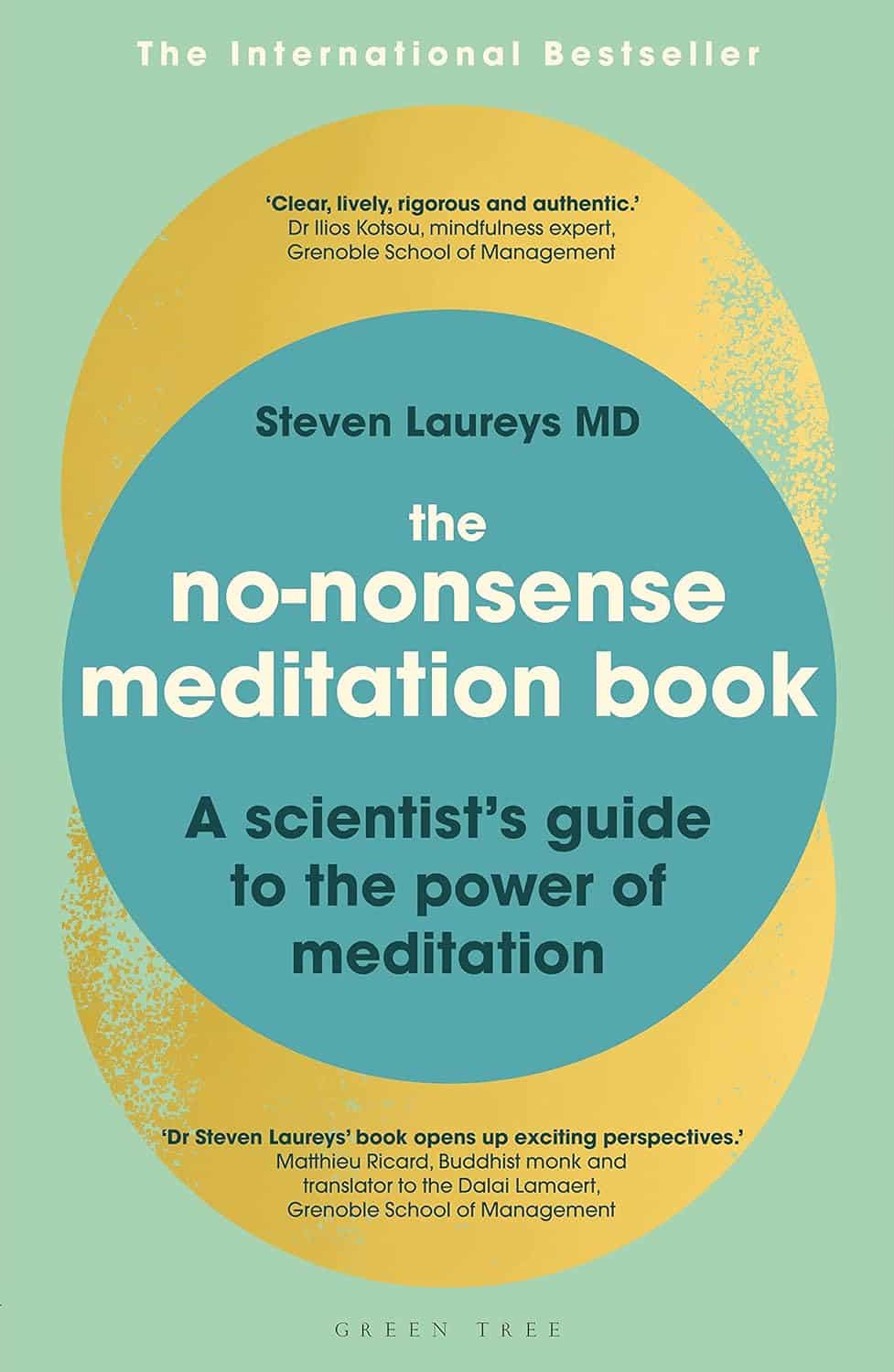
The No-Nonsense Meditation Book – by Dr. Steven Laureys
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about meditation before, and when we review books, we try to pick ones that have something that make them stand out from the others. So, what stands out in this case?
The author is a medical doctor and neurologist, with decades of experience focusing on neuronal plasticity and multimodel neural imaging. So, a little beyond “think happy thoughts”-style woo.
The style of the book is pop-science in tone, but with a lot of hard clinical science underpinning it and referenced throughout, as one would expect of a scientist of Dr. Laurey’s stature (with hundreds of peer-reviewed papers in top-level journals).
You may be wondering: is this a “how-to” book or a “why-to” book or a “what-happens” book? It’s all three.
The “how-to” is also, as the title suggests, no-nonsense. We are talking maximum results for minimum mystery here.
Bottom line: if you’d like to be able to take up a meditative practice and know exactly what it’s doing to your brain (quietening these parts, stimulating and physically growing those parts, etc) then this is the book for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: