Debunking the vitamin D fad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Throughout the pandemic, many unproven miracle COVID-19 “cures” emerged, and vitamin D claims have been one of the most persistent. This is not new for the vitamin. It’s been touted in recent decades as a way to “boost” the immune system, improve overall health, prevent a host of diseases, and allegedly even substitute for vaccines.
But as with many internet-popular health “remedies,” the reality is far less flashy and far more nuanced.
What is vitamin D, and why is it important?
Vitamin D is a nutrient that helps the body absorb calcium, which is essential for bone health. In the sunlight, your skin naturally produces vitamin D that is then stored in fat cells until it is used.
The skin pigment melanin absorbs the UV rays necessary for vitamin D production, meaning that more highly pigmented or darker skin produces less vitamin D than lighter skin with the same amount of sun exposure. Thus, people with darker skin are at higher risk of vitamin D deficiency.
Most of our vitamin D comes from the sun. An additional 10 percent to 20 percent of our vitamin D comes from foods like fatty fish (such as salmon), eggs, and mushrooms. Vitamin D supplements are another source of the nutrient for people who are unable to get enough from sun exposure and diet.
Vitamin D deficiency is real, but there’s no epidemic
Some people who promote vitamin D supplements claim that vitamin D deficiency is an epidemic causing widespread health issues. There is little evidence to support this claim. A 2022 analysis of 2001-2018 data found that 2.6 percent of people in the U.S. had severe vitamin D deficiency.
Severe vitamin D deficiency can cause serious health issues, such as muscle weakness, bone loss in adults, and rickets (weak bones) in children. Some people are at higher risk for the deficiency, including individuals with certain disorders that prevent the body from absorbing or processing vitamin D or those with a family history of vitamin D deficiency.
Black Americans have the highest rates of severe vitamin D deficiency at nearly 12 percent. Severe vitamin D deficiency is also slightly higher in the U.S. during the winter when people get less sun exposure. Rates of moderate vitamin D deficiency are higher at 22 percent overall and are highest among Black Americans (49 percent) and Mexican Americans (35 percent).
Although severe vitamin D deficiency exists in the U.S., it is far from common. Most tellingly, conditions that are directly linked to vitamin D deficiency are not widespread. There is no epidemic of rickets, for example, or bone loss in adults.
There’s little evidence that vitamin D supplements improve overall health
Vitamin D supplements have clear, proven positive effects for people with vitamin D deficiency. Other health benefits of vitamin D supplements are less certain.
There is some evidence that the supplement may reduce the risk of fracture in adults with osteoporosis, a condition that causes weak, fragile bones. However, the benefit appears to be limited to people who have low vitamin D levels. In adults with normal vitamin D levels, supplements have no effect on fracture risk.
The largest randomized controlled trial of vitamin D, called VITAL, investigated the effects of vitamin D supplementation in people without an existing deficiency. The study found that vitamin D supplements had no effects on the risk of cancer, diabetes, or cardiovascular disease, including heart attack and stroke. The study concluded that more research is necessary to determine who may benefit from vitamin D supplements.
Independent analyses found that vitamin D supplementation may be associated with a long-term decrease in cancer mortality, but results are mixed and also require more investigation.
A 2021 analysis of past vitamin D trials found no overall health benefits from vitamin D supplements in people with normal vitamin D levels. Most large-scale studies have found no link between vitamin D supplements and lower all-cause mortality (deaths from any cause), except in older adults and those with vitamin D deficiency.
Vitamin D provides modest protection against respiratory infections
Vitamin D is important for immune function, but this is often misconstrued as vitamin D “boosting” the immune system.
Some people falsely believe that taking vitamin D supplements will keep them healthy and prevent infections like the flu or COVID-19. In reality, clinical trials and large-scale studies of vitamin D have found only minimal protective effects against respiratory infections.
A 2021 analysis of 46 trials found that 61.3 percent of participants who took daily vitamin D supplements got respiratory infections during the study periods—compared to 62.3 percent of people who did not take the supplements. A 2024 meta-analysis of 43 trials found no overall protective effect against respiratory infections, but it detected a slight decrease in risk among people who took specific doses daily.
In young children, there is some evidence that vitamin D supplementation may reduce the length of respiratory infections. However, it does not affect the number or severity of infections that children have.
Despite claims that taking vitamin D can protect against COVID-19, two clinical trials found that taking daily vitamin D supplements did not reduce the risk or severity of COVID-19 infections, even at high doses.
Context is key when considering vitamin D’s benefits
None of these studies contradict the well-established evidence that people with vitamin D deficiency benefit from vitamin D supplements. But it’s important to remember that many of the most popular health claims about vitamin D’s benefits are based on research in people with vitamin D deficiency.
Research in vitamin D-deficient populations is important, but it tells us little about how vitamin D will affect people with normal or close to normal vitamin D levels. A closer look at vitamin D research in people without low levels reveals little evidence to support the idea that the general population benefits from taking vitamin D supplements.
For more information, or to learn about your vitamin D levels, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pelvic Floor Exercises (Not Kegels!) To Prevent Urinary Incontinence
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a common threat, and if you think it couldn’t happen to you, then well, just wait. Happily, Dr. Christine Pieton, PT, DPT, a sport & women’s health physical therapist, has advice:
On the ball!
Or rather, we’re going to be doing ball-squeezing here, if you’ll pardon the expression. You will need a soccer-ball sized ball to squeeze.
Ball-squeeze breathing: lie on your back, ball between your knees, and inhale deeply, expanding your torso. Exhale, pressing your knees into the ball, engaging your abdominal muscles from lower to upper. Try to keep your spine long and avoid your pelvis tucking under during the exhalation.
Ball-squeeze bridge: lie on your back, ball between your knees, inhale to prepare, and then exhale, pressing up into a bridge, maintaining a firm pressure on the ball. Inhale as you lower yourself back down.
Ball-squeeze side plank: lie on your side this time, ball between your knees, supporting forearm under your shoulder, as in the video thumbnail. Inhale to prepare, and then exhale, lifting your hip a few inches off the mat. Inhale as you lower yourself back down.
Ball-squeeze bear plank: get on your hands and knees, ball between your thighs. Lengthen your spine, inhale to prepare, and exhale as you bring your knees just a little off the floor. Inhale as you lower yourself back down.
For more details and tips on each of these, plus a visual demonstration, plus an optional part 2 video with more exercises that aren’t ball-squeezes this time, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Psst… A Word To The Wise About UTIs
Take care!
Share This Post
-
AI: The Doctor That Never Tires?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
AI: The Doctor That Never Tires?
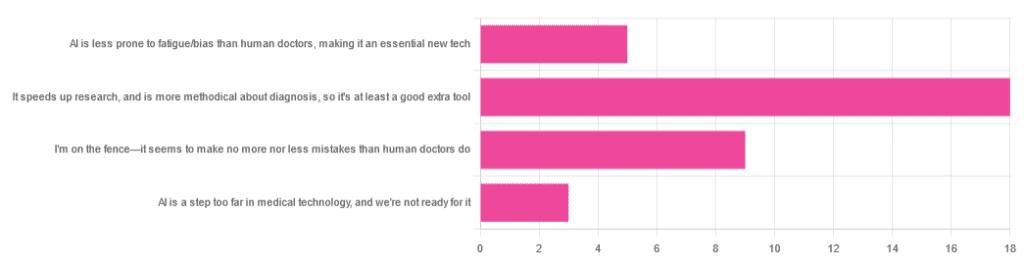
We asked you for your opinion on the use of Artificial Intelligence (AI) in healthcare, and got the above-depicted, below-described set of results:
- A little over half of respondents to the poll voted for “It speeds up research, and is more methodical about diagnosis, so it’s at least a good extra tool”
- A quarter of respondents voted for “I’m on the fence—it seems to make no more nor less mistakes than human doctors do”
- A little under a fifth of respondents voted for “AI is less prone to fatigue/bias than human doctors, making it an essential new tech”
- Three respondents voted for “AI is a step too far in medical technology, and we’re not ready for it”
Writer’s note: I’m a professional writer (you’d never have guessed, right?) and, apparently, I really did write “no more nor less mistakes”, despite the correct grammar being “no more nor fewer mistakes”. Now, I know this, and in fact, people getting less/fewer wrong is a pet hate of mine. Nevertheless, I erred.
Yet, now that I’m writing this out in my usual software, and not directly into the poll-generation software, my (AI!) grammar/style-checker is highlighting the error for me.
Now, an AI could not do my job. ChatGPT would try, and fail miserably. But can technology help me do mine better? Absolutely!
And still, I dismiss a lot of the AI’s suggestions, because I know my field and can make informed choices. I don’t follow it blindly, and I think that’s key.
AI is less prone to fatigue/bias than human doctors, making it an essential new tech: True or False?
True—with one caveat.
First, a quick anecdote from a subscriber who selected this option in the poll:
❝As long as it receives the same data inputs as my doctor (ie my entire medical history), I can see it providing a much more personalised service than my human doctor who is always forgetting what I have told him. I’m also concerned that my doctor may be depressed – not an ailment that ought to affect AI! I recently asked my newly qualified doctor goddaughter whether she would prefer to be treated by a human or AI doctor. No contest, she said – she’d go with AI. Her argument was that human doctors leap to conclusions, rather than properly weighing all the evidence – meaning AI, as long as it receives the same inputs, will be much more reliable❞
Now, an anecdote is not data, so what does the science say?
Well… It says the same:
❝Of 6695 responding physicians in active practice, 6586 provided information on the areas of interest: 3574 (54.3%) reported symptoms of burnout, 2163 (32.8%) reported excessive fatigue, and 427 (6.5%) reported recent suicidal ideation, with 255 of 6563 (3.9%) reporting a poor or failing patient safety grade in their primary work area and 691 of 6586 (10.5%) reporting a major medical error in the prior 3 months. Physicians reporting errors were more likely to have symptoms of burnout (77.6% vs 51.5%; P<.001), fatigue (46.6% vs 31.2%; P<.001), and recent suicidal ideation (12.7% vs 5.8%; P<.001).❞
See the damning report for yourself: Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors
AI, of course, does not suffer from burnout, fatigue, or suicidal ideation.
So, what was the caveat?
The caveat is about bias. Humans are biased, and that goes for medical practitioners just the same. AI’s machine learning is based on source data, and the source data comes from humans, who are biased.
See: Bias and Discrimination in AI: A Cross-Disciplinary Perspective
So, AI can perpetuate human biases and doesn’t have a special extra strength in this regard.
The lack of burnout, fatigue, and suicidal ideation, however, make a big difference.
AI speeds up research, and is more methodical about diagnosis: True or False?
True! AI is getting more and more efficient at this, and as has been pointed out, doesn’t make errors due to fatigue, and often comes to accurate conclusions near-instantaneously. To give just one example:
❝Deep learning algorithms achieved better diagnostic performance than a panel of 11 pathologists participating in a simulation exercise designed to mimic routine pathology workflow; algorithm performance was comparable with an expert pathologist interpreting whole-slide images without time constraints. The area under the curve was 0.994 (best algorithm) vs 0.884 (best pathologist).❞
About that “getting more and more efficient at this”; it’s in the nature of machine learning that every new piece of data improves the neural net being used. So long as it is getting fed new data, which it can process at rate far exceeding humans’ abilities, it will always be constantly improving.
AI makes no more nor
lessfewer mistakes than humans do: True or False?False! AI makes fewer, now. This study is from 2021, and it’s only improved since then:
❝Professionals only came to the same conclusions [as each other] approximately 75 per cent of the time. More importantly, machine learning produced fewer decision-making errors than did all the professionals❞
See: AI can make better clinical decisions than humans: study
All that said, we’re not quite at Star Trek levels of “AI can do a human’s job entirely” just yet:
BMJ | Artificial intelligence versus clinicians: pros and cons
To summarize: medical AI is a powerful tool that:
- Makes healthcare more accessible
- Speeds up diagnosis
- Reduces human error
…and yet, for now at least, still requires human oversights, checks and balances.
Essentially: it’s not really about humans vs machines at all. It’s about humans and machines giving each other information, and catching any mistakes made by the other. That way, humans can make more informed decisions, and still keep a “hand on the wheel”.
Share This Post
-
Foods For Managing Hypothyroidism (incl. Hashimoto’s)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Foods for Managing Hypothyroidism
For any unfamiliar, hypothyroidism is the condition of having an underactive thyroid gland. The thyroid gland lives at the base of the front of your neck, and, as the name suggests, it makes and stores thyroid hormones. Those are important for many systems in the body, and a shortage typically causes fatigue, weight gain, and other symptoms.
What causes it?
This makes a difference in some cases to how it can be treated/managed. Causes include:
- Hashimoto’s thyroiditis, an autoimmune condition
- Severe inflammation (end result is similar to the above, but more treatable)
- Dietary deficiencies, especially iodine deficiency
- Secondary endocrine issues, e.g. pituitary gland didn’t make enough TSH for the thyroid gland to do its thing
- Some medications (ask your pharmacist)
We can’t do a lot about those last two by leveraging diet alone, but we can make a big difference to the others.
What to eat (and what to avoid)
There is nuance here, which we’ll go into a bit, but let’s start by giving the
one-linetwo-line summary that tends to be the dietary advice for most things:- Eat a nutrient-dense whole-foods diet (shocking, we know)
- Avoid sugar, alcohol, flour, processed foods (ditto)
What’s the deal with meat and dairy?
- Meat: avoid red and processed meats; poultry and fish are fine or even good (unless fried; don’t do that)
- Dairy: limit/avoid milk; but unsweetened yogurt and cheese are fine or even good
What’s the deal with plants?
First, get plenty of fiber, because that’s important to ease almost any inflammation-related condition, and for general good health for most people (an exception is if you have Crohn’s Disease, for example).
If you have Hashimoto’s, then gluten (as found in wheat, barley, and rye) may be an issue, but the jury is still out, science-wise. Here’s an example study for “avoid gluten” and “don’t worry about gluten”, respectively:
- The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Women with Hashimoto’s Thyroiditis
- Doubtful Justification of the Gluten-Free Diet in the Course of Hashimoto’s Disease
So, you might want to skip it, to be on the safe side, but that’s up to you (and the advice of your nutritionist/doctor, as applicable).
A word on goitrogens…
Goitrogens are found in cruciferous vegetables and soy, both of which are very healthy foods for most people, but need some extra awareness in the case of hypothyroidism. This means there’s no need to abstain completely, but:
- Keep serving sizes small, for example a 100g serving only
- Cook goitrogenic foods before eating them, to greatly reduce goitrogenic activity
For more details, reading even just the abstract (intro summary) of this paper will help you get healthy cruciferous veg content without having a goitrogenic effect.
(as for soy, consider just skipping that if you suffer from hypothyroidism)
What nutrients to focus on getting?
- Top tier nutrients: iodine, selenium, zinc
- Also important: vitamin B12, vitamin D, magnesium, iron
Enjoy!
Share This Post
Related Posts
-
The Longevity Project – by Dr. Howard Friedman & Dr. Leslie Martin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most books on the topic of longevity focus on such things as diet and exercise, and indeed, those are of course important things. But what of psychological and sociological factors?
Dr. Friedman and Dr. Martin look at a landmark longitudinal study, following a large group of subjects from childhood into old age. Looking at many lifestyle factors and life events, they crunched the numbers to see what things really made the biggest impact on healthy longevity.
A strength of the book is that this study had a huge amount of data—a limitation of the book is that it often avoids giving that concrete data, preferring to say “many”, “a majority”, “a large minority”, “some”, and so forth.
However, the conclusions from the data seem clear, and include many observations such as:
- conscientiousness is a characteristic that not only promotes healthy long life, but also can be acquired as time goes by (some “carefree” children became “conscientious” adults)
- resilience is a characteristic that promotes healthy long life—but tends to only be “unlocked” by adversity
- men tend to live longer if married—women, not so much
- religion and spirituality are not big factors in healthy longevity—but social connections (that may or may not come with such) do make a big difference
Bottom line: if you’d like to know which of your decisions are affecting your healthy longevity (beyond the obvious diet, exercise, etc), this is a great book for collating that information and presenting, in essence, a guideline for a long healthy life.
Click here to check out The Longevity Project and see how it applies to your life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Useful Is Peppermint, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Peppermint For Digestion & Against Nausea
Peppermint is often enjoyed to aid digestion, and sometimes as a remedy for nausea, but what does the science say about these uses?
Peppermint and digestion
In short: it works! (but beware)
Most studies on peppermint and digestion, that have been conducted with humans, have been with regard to IBS, but its efficacy seems quite broad:
❝Peppermint oil is a natural product which affects physiology throughout the gastrointestinal tract, has been used successfully for several clinical disorders, and appears to have a good safety profile.❞
However, and this is important: if your digestive problem is GERD, then you may want to skip it:
❝The univariate logistic regression analysis showed the following risk factors: eating 1–2 meals per day (OR = 3.50, 95% CI: 1.75–6.98), everyday consumption of peppermint tea (OR = 2.00, 95% CI: 1.14–3.50), and eating one, big meal in the evening instead of dinner and supper (OR = 1.80, 95% CI: 1.05–3.11).
The multivariate analysis confirmed that frequent peppermint tea consumption was a risk factor (OR = 2.00, 95% CI: 1.08–3.70).❞
~ Dr. Jarosz & Dr. Taraszewska
Source: Risk factors for gastroesophageal reflux disease: the role of diet
Peppermint and nausea
Peppermint is also sometimes recommended as a nausea remedy. Does it work?
The answer is: maybe
The thing with nausea is it is a symptom with a lot of possible causes, so effectiveness of remedies may vary. But for example:
- Aromatherapy for treatment of postoperative nausea and vomiting ← no better than placebo
- The Effect of Combined Inhalation Aromatherapy with Lemon and Peppermint on Nausea and Vomiting of Pregnancy: A Double-Blind, Randomized Clinical Trial ← initially no better than placebo, then performed better on subsequent days
- The Effects of Peppermint Oil on Nausea, Vomiting and Retching in Cancer Patients Undergoing Chemotherapy: An Open Label Quasi-Randomized Controlled Pilot Study ← significant benefit immediately
Summary
Peppermint is useful against wide variety of gastrointestinal disorders, including IBS, but very definitely excluding GERD (in the case of GERD, it may make things worse)
Peppermint may help with nausea, depending on the cause.
Where can I get some?
Peppermint tea, and peppermint oil, you can probably find in your local supermarket (as well as fresh mint leaves, perhaps).
For the “heavy guns” that is peppermint essential oil, here’s an example product on Amazon for your convenience
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eat Move Sleep – by Tom Rath
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle of this book, “how small choices lead to big changes“, is very much the idea that a lot of what we do here at 10almonds is about.
And the title itself, “Eat Move Sleep”? Well, that’s 3/5 of The Usual Five Things™ that we promote here (the other two being: reduce or eliminate alcohol, and don’t smoke). So, naturally this book got our attention.
One of the key ideas that Rath presents is that every action we take leads to a net gain or loss in health. The question then is: what are the biggest point-swingers? In other words, what are the places in our life where the smallest changes can make the biggest difference?
Rath looks at what parts of diet make the biggest difference to our health, and the findings there alone probably make reading the book worthwhile.
When it comes to movement, he actually flips this! For Rath, it’s less about how much exercise you get, and more about minimizing how long we spend not moving… And especially, minimizing how long we spend sitting. So, lots of little tweaks for that.
In the category of sleep: a key idea is that quality is as important as quantity, and there’s an aspect of bringing together as a synergistic routine. To finish off a productive day with good rest, and power up ready for the next morning.
In short: tying these items together—and focusing on the smallest choices that lead to the biggest changes—makes for quite a manifesto that we could describe as “Atomic Habits, for health specifically”.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: