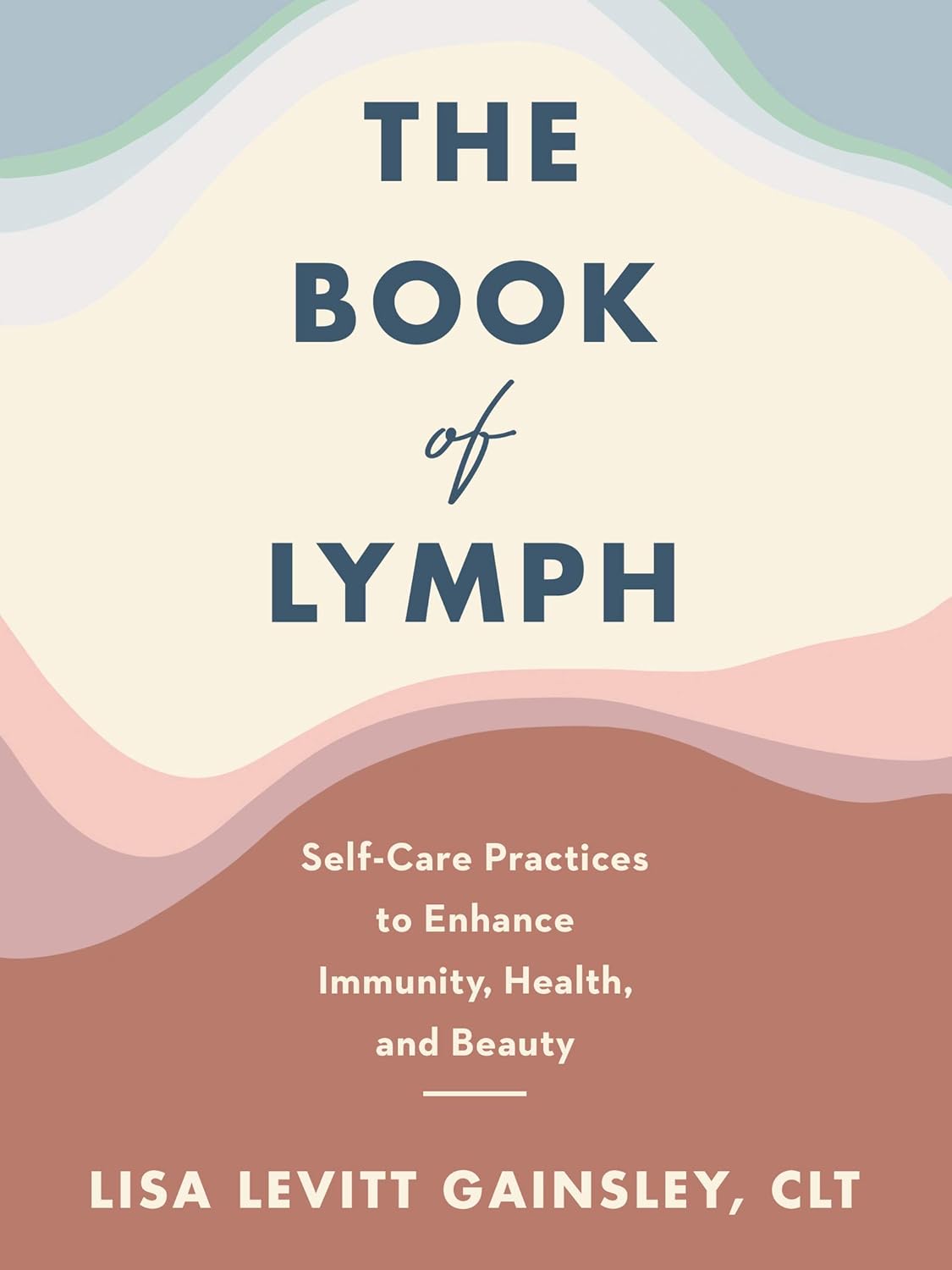
The Book of Lymph – by Lisa Levitt Gainsely
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book starts with an overview of what lymph is and why it matters, before getting into the main meat of the book, which is lymphatic massage techniques to improve lymphatic flow/drainage throughout different parts of the body, and in the context of an assortment of common maladies that may merit particular attention.
There’s an element of aesthetic medicine here, and improving beauty, but there’s also a whole section devoted to such things as breast care and the like (bearing in mind, the lymphatic system is one of our main defenses against cancer). There’s also a lot about managing lymph in the context of chronic health conditions.
The style is light pop-science; the science is explained clearly throughout, but without academic citations every few lines as some books might have. The author is, after all, a practitioner (CLT) and/but not an academic.
Bottom line: if you’d like to improve your lymphatic health, whether for beauty or health maintenance or recovery, this book will walk you through it.
Click here to check out The Book of Lymph, and give yours some love!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fitness In Our Fifties
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: What’s a worthwhile fitness goal for people in their 50s?
A: At 10almonds, we think that goals are great but habits are better.
If your goal is to run a marathon, that’s a fine goal, and can be very motivating, but then after the marathon, then what? You’ll look back on it as a great achievement, but what will it do for your future health?
PS, yes, marathon-running in one’s middle age is a fine and good activity for most people. Maybe skip it if you have osteoporosis or some other relevant problem (check with your doctor), but…
Marathons in Mid- and Later-Life ← we wrote about the science of it here
PS, we also explored some science that may be applicable to your other question, on the same page as that about marathons!
The thing about habits vs goals is that habits give ongoing cumulative (often even: compounding) benefits:
How To Really Pick Up (And Keep!) Those Habits
If you pressingly want advice on goals though, our advice is this:
Make it your goal to be prepared for the health challenges of later life. It may seem gloomy to say that old age is coming for us all if something else doesn’t get us first, but the fact is, old age does not have to come with age-related decline, and the very least, we can increase our healthspan (so we’re hitting 90 with most of the good health we enjoyed in our 70s, for example, or hitting 80 with most of the good health we enjoyed in our 60s).
If that goal seems a little wishy-washy, here are some very specific and practical ideas to get you started:
Train For The Event Of Your Life!
As for the limits and/or extents of how much we can do in that regard? Here are what two aging experts have to say:
And here’s what we at 10almonds had to say:
Age & Aging: What Can (And Can’t) We Do About It?
Take care!
Share This Post
-
Ageless Athletes – by Dr. Jim Madden
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is an approach to strength and fitness training specifically for the 50+ crowd, and/but even more specifically for the 50+ crowd who do not wish to settle for mediocrity. In short, it’s for those who not only wish to stay healthy and have good mobility, but also who wish to be and remain athletic.
It does not assume extant athleticism, but nor does it assume complete inexperience. It provides a fairly ground-upwards entry to a training program that then quickly proceeds to competitive levels of athleticism.
The author himself details his own journey from being in his 30s, overweight and unfit, to being in his 50s and very athletic, with before and after photos. Granted, those are 20 years in between, but all the same, it’s a good sign when someone gets stronger and fitter with age, rather than declining.
The style of the book is quite casual, and/but after the introductory background and pep talk, is quite pragmatic and drops the additional fluff. In particular, older readers may enjoy the “Old Workhorse” protocol, as a tailored measured progression system.
In terms of expected equipment by the way, some is bodyweight and some is with weights; kettlebells in particular feature strongly, since this is about functional strength and not bodybuilding.
In the category of criticism, he does refer to his other books and generally assumes the reader is reading all his work, so it may not be for everyone as a standalone book.
Bottom line: if you’re 50+ and are wondering how to gain/maintain a high level athleticism, this book can definitely help with that.
Click here to check out Ageless Athlete, and go from strength to strength!
Share This Post
-
The Comfort Book – by Matt Haig
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book “is what it says on the tin”. Matt Haig, bestselling author of “Reasons to Stay Alive” (amongst other works) is here with “a hug in a book”.
The format of the book is an “open it at any page and you’ll find something of value” book. Its small chapters are sometimes a few pages long, but often just a page. Sometimes just a line. Always deep.
All of us, who live long enough, will ponder our mortality sometimes. The feelings we may have might vary on a range from “afraid of dying” to “despairing of living”… but Haig’s single biggest message is that life is full of wonder; each moment precious.
- That hope is an incredible (and renewable!) resource.
- That we are more than a bad week, or month, or year, or decade.
- That when things are taken from us, the things that remain have more value.
Bottom line: you might cry (this reviewer did!), but it’ll make your life the richer for it, and remind you—if ever you need it—the value of your amazing life.
Share This Post
Related Posts
-
The Many Faces Of Cosmetic Surgery
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cosmetic Surgery: What’s The Truth?
In Tuesday’s newsletter, we asked you your opinion on elective cosmetic surgeries, and got the above-depicted, below-described, set of responses:
- About 48% said “Everyone should be able to get what they want, assuming informed consent”
- About 28% said “It can ease discomfort to bring features more in line with normalcy”
- 15% said “They should be available in the case of extreme disfigurement only”
- 10% said “No elective cosmetic surgery should ever be performed; needless danger”
Well, there was a clear gradient of responses there! Not so polarizing as we might have expected, but still enough dissent for discussion
So what does the science say?
The risks of cosmetic surgery outweigh the benefits: True or False?
False, subjectively (but this is important).
You may be wondering: how is science subjective?
And the answer is: the science is not subjective, but people’s cost:worth calculations are. What’s worth it to one person absolutely may not be worth it to another. Which means: for those for whom it wouldn’t be worth it, they are usually the people who will not choose the elective surgery.
Let’s look at some numbers (specifically, regret rates for various surgeries, elective/cosmetic or otherwise):
- Regret rate for elective cosmetic surgery in general: 20%
- Regret rate for knee replacement (i.e., not cosmetic): 17.1%
- Regret rate for hip replacement (i.e., not cosmetic): 4.8%
- Regret rate for gender-affirming surgeries (for transgender patients): 1%
So we can see, elective surgeries have an 80–99% satisfaction rate, depending on what they are. In comparison, the two joint replacements we mentioned have a 82.9–95.2% satisfaction rate. Not too dissimilar, taken in aggregate!
In other words: if a person has studied the risks and benefits of a surgery and decides to go ahead, they’re probably going to be happy with the results, and for them, the benefits will have outweighed the risks.
Sources for the above numbers, by the way:
- What is the regret rate for plastic surgery?
- Decision regret after primary hip and knee replacement surgery
- A systematic review of patient regret after surgery—a common phenomenon in many specialties but rare within gender-affirmation surgery
But it’s just a vanity; therapy is what’s needed instead: True or False?
False, generally. True, sometimes. Whatever the reasons for why someone feels the way they do about their appearance—whether their face got burned in a fire or they just have triple-J cups that they’d like reduced, it’s generally something they’ve already done a lot of thinking about. Nevertheless, it does also sometimes happen that it’s a case of someone hoping it’ll be the magical solution, when in reality something else is also needed.
How to know the difference? One factor is whether the surgery is “type change” or “restorative”, and both have their pros and cons.
- In “type change” (e.g. rhinoplasty), more psychological adjustment is needed, but when it’s all over, the person has a new nose and, statistically speaking, is usually happy with it.
- In “restorative” (e.g. facelift), less psychological adjustment is needed (as it’s just a return to a previous state), so a person will usually be happy quickly, but ultimately it is merely “kicking the can down the road” if the underlying problem is “fear of aging”, for example. In such a case, likely talking therapy would be beneficial—whether in place of, or alongside, cosmetic surgery.
Here’s an interesting paper on that; the sample sizes are small, but the discussion about the ideas at hand is a worthwhile read:
Does cosmetic surgery improve psychosocial wellbeing?
Some people will never be happy no matter how many surgeries they get: True or False?
True! We’re going to refer to the above paper again for this one. In particular, here’s what it said about one group for whom surgeries will not usually be helpful:
❝There is a particular subgroup of people who appear to respond poorly to cosmetic procedures. These are people with the psychiatric disorder known as “body dysmorphic disorder” (BDD). BDD is characterised by a preoccupation with an objectively absent or minimal deformity that causes clinically significant distress or impairment in social, occupational, or other areas of functioning.
For several reasons, it is important to recognise BDD in cosmetic surgery settings:
Firstly, it appears that cosmetic procedures are rarely beneficial for these people. Most patients with BDD who have had a cosmetic procedure report that it was unsatisfactory and did not diminish concerns about their appearance.
Secondly, BDD is a treatable disorder. Serotonin-reuptake inhibitors and cognitive behaviour therapy have been shown to be effective in about two-thirds of patients with BDD❞
~ Dr. David Castle et al. (lightly edited for brevity)
Which is a big difference compared to, for example, someone having triple-J breasts that need reducing, or the wrong genitals for their gender, or a face whose features are distinct outliers.
Whether that’s a reason people with BDD shouldn’t be able to get it is an ethical question rather than a scientific one, so we’ll not try to address that with science.
After all, many people (in general) will try to fix their woes with a haircut, a tattoo, or even a new sportscar, and those might sometimes be bad decisions, but they are still the person’s decision to make.
And even so, there can be protectionist laws/regulations that may provide a speed-bump, for example:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Mistakes To Sabotage Your Ozempic Progress
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ozempic has a good reputation for getting reliable results, but there are ways to mess it up:
It’s not just inject-and-go
We’ll not keep the 10 ways a secret; they are:
- Increasing the dose too quickly: avoid cranking doses up too high too quickly, to prevent severe nausea, appetite suppression, and muscle loss. It’s worth being aware that high doses without proper management can lead to metabolic health disasters.
- Pushing through side effects: severe nausea or vomiting means you probably have an unhelpfully high dose; consult your prescribing doctor—it’s easy to feel “more is better; I don’t want to have less!”, but there really is a sweet spot, and if you’re not in it, then adjustments are needed in order to find it.
- Eating nutritionally scant food: reducing the quantity of unhealthy food isn’t enough—please prioritize nutrient-rich foods instead. Remember, “it’s not the calories in your food; it’s the food in your calories”.
- Consuming fried food and refined carbs: their general metabolic woes aside, fried foods and ultra-refined carbs can exacerbate nausea and other side effects, so it really is best to skip them. The good news is that Ozempic will help overcome those cravings more easily.
- Neglecting muscle protection: especially women, especially middle-aged or older, are at higher risk of osteoporosis and should maintain muscle mass (strong muscles and strong bones go together, by necessity). So, eat protein and do resistance training!
- Assuming it’s a monotherapy: GLP-1 drugs work best as part of a holistic protocol, including proper nutrition, strength training, and hormone therapy if appropriate.
- Not addressing metabolic health first: GLP-1 drugs are less effective in people with poor baseline metabolic health, so there’s a bit of a catch-22 here, but it’s important to be aware of. Fortunately, Ozempic and adopting a healthy lifestyle will each make the other work better.
- Neglecting comprehensive treatment plans: in other words, going through the motions of a holistic protocol and then expecting Ozempic to do all the work.
- Upping doses to overcome plateaus: plateaus often signal other issues (e.g. lack of protein, no strength training), so do address these before increasing dosage.
- Lack of collaboration with doctors: the human body is complex, and what’s going on metabolically is complex too, so there’s a lot a layperson can easily miss. For that matter, there’s a lot that doctors can easily miss too, but more heads are better than one.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
5 Ways To Naturally Boost The Ozempic Effect
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Best Foods For Collagen Production
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Andrea Suarez gives us the low-down on collagen synthesis and maintenance. Collagen is the most abundant protein in our body, and it can be fairly described as “the stuff that holds us together”. It’s particularly important for joints and bones too, though many people’s focus on it is for the skin. Whatever your priorities, collagen levels are something it pays to be mindful of, as they usually drop quite sharply after a certain age. What certain age? Well, that depends a lot on you, and your diet and lifestyle. But it can start to decline from the age of 30 with often noticeable drop-offs in one’s mid-40s and again in one’s mid-60s.
Showing us what we’re made of
There’s a lot more to having good collagen levels than just how much collagen we consume (which for vegetarians/vegans, will be “none”, unless using the “except if for medical reasons” exemption, which is probably a little tenuous in the case of collagen but nevertheless it’s a possibility; this exemption is usually one that people use for, say, a nasal spray vaccine that contains gelatine, or a medicinal tablet that contains lactose, etc).
Rather, having good collagen levels is also a matter of what we eat that allows us to synthesize our own collagen (which includes: its ingredients, and various “helper” nutrients), as well as what dietary adjustments we make to avoid our extant collagen getting broken down, degraded, and generally lost.
Here’s what Dr. Suarez recommends:
Protein-rich foods (but watch out)
- Protein is essential for collagen production.
- Sources: fish, soy, lean meats (but not red meats, which—counterintuitively—degrade collagen), eggs, lentils.
- Egg whites are high in lysine, vital for collagen synthesis.
- Bone broth is a natural source of collagen.
Omega-3 fatty acids
- Omega-3s are anti-inflammatory and protect skin collagen.
- Sources: walnuts, chia seeds, flax seeds, fatty fish (e.g. mackerel, sardines).
Leafy greens
- Leafy dark green vegetables (e.g. kale, spinach) are rich in vitamins C and B9.
- Vitamin C is crucial for collagen synthesis and acts as an antioxidant.
- Vitamin B9 supports skin cell division and DNA repair.
Red fruits & vegetables
- Red fruits/vegetables (e.g. tomatoes, red bell peppers) contain lycopene, an antioxidant that protects collagen from UV damage (so, that aspect is mostly relevant for skin, but antioxidants are good things to have in all of the body in any case).
Orange-colored vegetables
- Carrots and sweet potatoes are rich in vitamin A, which helps in collagen repair and synthesis.
- Vitamin A is best from food, not supplements, to avoid potential toxicity.
Fruits rich in vitamin C
- Citrus fruits, kiwi, and berries are loaded with vitamin C and antioxidants, essential for collagen synthesis and skin health.
Soy
- Soy products (e.g. tofu, soybeans) contain isoflavones, which reduce inflammation and inhibit enzymes that degrade collagen.
- Soy is associated with lower risks of chronic diseases.
Garlic
- Garlic contains sulfur, taurine, and lipoic acid, important for collagen production and repair.
What to avoid:
- Reduce foods high in advanced glycation end products (AGEs), which damage collagen and promote inflammation.
- AGEs are found in fried, roasted, or grilled fatty proteinous foods (e.g. meat, including synthetic meat, and yes, including grass-fed nicely marketed meat—although processed meat such as bacon and sausages are even worse than steaks etc).
- Switch to cooking methods like boiling or steaming to reduce AGE levels.
- Processed foods, sugary pastries, and red meats contribute to collagen degradation.
General diet tips:
- Incorporate more plant-based, antioxidant-rich foods.
- Opt for slow cooking to reduce AGEs.
- Since sustainability is key, choose foods you enjoy for a collagen-boosting diet that you won’t seem like a chore a month later.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
We Are Such Stuff As Fish Are Made Of ← our main feature research review about collagen
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: