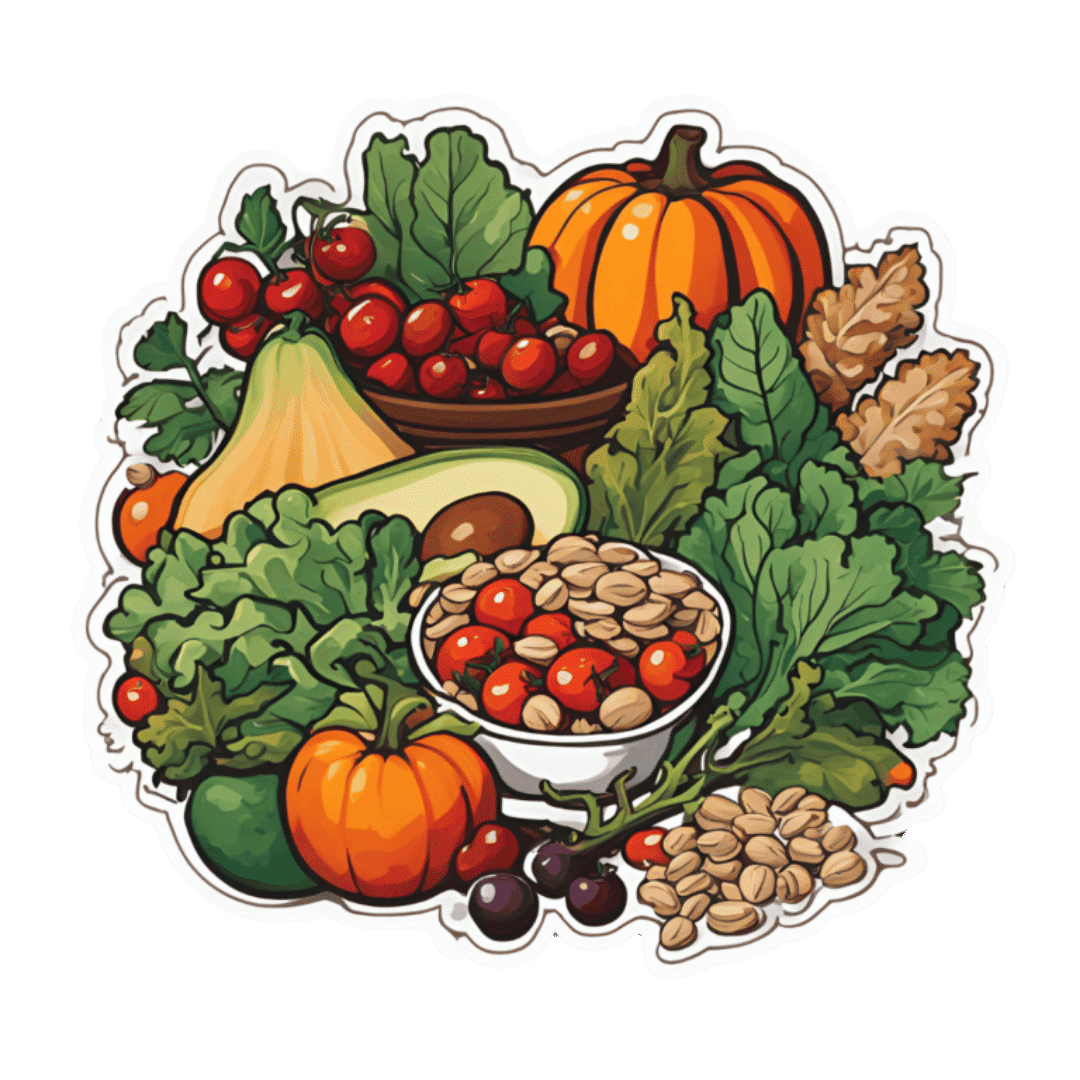
12 Foods That Fight Depression & Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Food impacts mental health, and while it won’t magically cure mental illness, dietary changes can do a lot to improve mood. Here’s how:
Nutraceuticals
We’ll not keep the 12 nutraceutical foods a mystery; here’s what they are and a few words on how they work (in many cases, we could write whole articles about them; in some cases, we already have! You can find many of them by using the search function in the top-right of each page).
- Walnuts are rich in omega-3s for brain health; arguably the best nut for depression relief.
- Fermented foods because probiotics in foods like yogurt and sauerkraut support the gut-brain connection as well as serotonin production there, enhancing mood.
- Cherry tomatoes are rich in lycopene, which helps combat both depression and mood swings.
- Leafy greens reduce brain inflammation linked to depression.
- Apples and other fruit are high in fiber and antioxidants that stabilize blood sugar and mood, reducing brain inflammation.
- Beans are high in B vitamins, crucial for neurotransmitter production and mood regulation (without also being high in brain-harmful things, as red meat is).
- Berries are super-high antioxidants and cortisol-lowering anthocyanidins, promoting calmness and reducing stress.
- Oats contain the healthiest kind of fiber, β-glucan, and additionally help stabilize blood sugar and mood; they’re also rich in selenium, which boosts mood.
- Mushrooms help regulate blood sugar and act as prebiotics, supporting serotonin production in the gut.
- Avocados are famously rich in healthy fats, including omega-3s and oleic acid, which support brain health and combat depression.
- Dark chocolate contains antioxidants, magnesium, and gut-healthy prebiotics that indirectly reduce mental stress and improve brain function. Also a famous comfort food for many, of course, and that factor’s not to be overlooked either.
- Pumpkin seeds are rich in tryptophan, which boosts serotonin production. As a bonus, they also help some kinds of antidepressant to work better—check with your doctor or pharmacist to be sure in your case, though.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The 6 Pillars Of Nutritional Psychiatry
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is childhood dementia? And how could new research help?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Childhood” and “dementia” are two words we wish we didn’t have to use together. But sadly, around 1,400 Australian children and young people live with currently untreatable childhood dementia.
Broadly speaking, childhood dementia is caused by any one of more than 100 rare genetic disorders. Although the causes differ from dementia acquired later in life, the progressive nature of the illness is the same.
Half of infants and children diagnosed with childhood dementia will not reach their tenth birthday, and most will die before turning 18.
Yet this devastating condition has lacked awareness, and importantly, the research attention needed to work towards treatments and a cure.
More about the causes
Most types of childhood dementia are caused by mutations (or mistakes) in our DNA. These mistakes lead to a range of rare genetic disorders, which in turn cause childhood dementia.
Two-thirds of childhood dementia disorders are caused by “inborn errors of metabolism”. This means the metabolic pathways involved in the breakdown of carbohydrates, lipids, fatty acids and proteins in the body fail.
As a result, nerve pathways fail to function, neurons (nerve cells that send messages around the body) die, and progressive cognitive decline occurs.
Childhood dementia is linked to rare genetic disorders. maxim ibragimov/Shutterstock What happens to children with childhood dementia?
Most children initially appear unaffected. But after a period of apparently normal development, children with childhood dementia progressively lose all previously acquired skills and abilities, such as talking, walking, learning, remembering and reasoning.
Childhood dementia also leads to significant changes in behaviour, such as aggression and hyperactivity. Severe sleep disturbance is common and vision and hearing can also be affected. Many children have seizures.
The age when symptoms start can vary, depending partly on the particular genetic disorder causing the dementia, but the average is around two years old. The symptoms are caused by significant, progressive brain damage.
Are there any treatments available?
Childhood dementia treatments currently under evaluation or approved are for a very limited number of disorders, and are only available in some parts of the world. These include gene replacement, gene-modified cell therapy and protein or enzyme replacement therapy. Enzyme replacement therapy is available in Australia for one form of childhood dementia. These therapies attempt to “fix” the problems causing the disease, and have shown promising results.
Other experimental therapies include ones that target faulty protein production or reduce inflammation in the brain.
Research attention is lacking
Death rates for Australian children with cancer nearly halved between 1997 and 2017 thanks to research that has enabled the development of multiple treatments. But over recent decades, nothing has changed for children with dementia.
In 2017–2023, research for childhood cancer received over four times more funding per patient compared to funding for childhood dementia. This is despite childhood dementia causing a similar number of deaths each year as childhood cancer.
The success for childhood cancer sufferers in recent decades demonstrates how adequately funding medical research can lead to improvements in patient outcomes.
Dementia is not just a disease of older people. Miljan Zivkovic/Shutterstock Another bottleneck for childhood dementia patients in Australia is the lack of access to clinical trials. An analysis published in March this year showed that in December 2023, only two clinical trials were recruiting patients with childhood dementia in Australia.
Worldwide however, 54 trials were recruiting, meaning Australian patients and their families are left watching patients in other parts of the world receive potentially lifesaving treatments, with no recourse themselves.
That said, we’ve seen a slowing in the establishment of clinical trials for childhood dementia across the world in recent years.
In addition, we know from consultation with families that current care and support systems are not meeting the needs of children with dementia and their families.
New research
Recently, we were awarded new funding for our research on childhood dementia. This will help us continue and expand studies that seek to develop lifesaving treatments.
More broadly, we need to see increased funding in Australia and around the world for research to develop and translate treatments for the broad spectrum of childhood dementia conditions.
Dr Kristina Elvidge, head of research at the Childhood Dementia Initiative, and Megan Maack, director and CEO, contributed to this article.
Kim Hemsley, Head, Childhood Dementia Research Group, Flinders Health and Medical Research Institute, College of Medicine and Public Health, Flinders University; Nicholas Smith, Head, Paediatric Neurodegenerative Diseases Research Group, University of Adelaide, and Siti Mubarokah, Research Associate, Childhood Dementia Research Group, Flinders Health and Medical Research Institute, College of Medicine and Public Health, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Tiramisu Crunch Bites
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s coffee, it’s creamy, it’s nutty, it’s chocolatey, what’s not to love? It has all the well-loved flavors of tiramisu, but this recipe is a simple one, and it’s essentially stuffed dates in a way you’ve never had them before. They’re delectable, decadent, and decidedly good for your health. These things are little nutrient-bombs that’ll keep you reaching for more.
You will need
- Coffee (we will discuss this)
- 150g (5.5oz) mascarpone (if vegan or lactose-intolerant, can be substituted with vegan varieties, or at a pinch, pressed silken tofu)
- 500g (1lb) dates (Medjool are ideal)
- Twice as many almonds as you have dates
- 50g (2oz) dark chocolate (the darkest, bitterest, you can find)
- Edible flower petals if you can source them (some shops sell dried rose petals for this purpose)
Method
(we suggest you read everything at least once before doing anything)
1) Take the mascarpone and whisk (or blend) it with the coffee. What kind of coffee, you ask? Many will use instant coffee (1tbsp granules mixed with enough boiling water to dissolve it), and that is actually healthiest (counterintuitive but true) but if you care for flavor over health, and have the means to make espresso, make it ristretto (so, stop it halfway through filling up an espresso cup), let it cool, and use that. Absolute bonus for flavor (not for health): if you have the means to make Turkish coffee, use an equivalent amount of that (again, cooled).
You will now have coffee-flavoured mascarpone. It’s great for your gut and full of antioxidant polyphenols. Set it aside for the moment.
2) Take the dark chocolate and melt it. Please don’t microwave it or try to do it in a pan directly over the hob; instead, you will need to use a Bain-Marie. If you don’t have one made-for-purpose, you can place a metal or heatproof glass bowl in a saucepan, with something to stop it from touching the floor of the pan. Then boil water in the pan (without letting the water get into the bowl), and melt the chocolate in the bowl—this will allow you to melt it evenly without burning the chocolate.
You will now have melted dark chocolate. It has its own set of polyphenols, and is great for everything from the brain to the gut microbiome.
3) Cut the dates lengthways on one side and remove the stone. Stuff them carefully with the coffee-flavored mascarpone (you can use a teaspoon, or use a piping kit if you have one). Add a couple of almonds to each one. Place them all on a big plate, and drizzle the melted chocolate over them. Add the petals if you have them.
The dates and almonds deliver extra vitamins and minerals in abundance (not to mention, lots of fiber), and also are an amazing combination even just by themselves. With the mascarpone and chocolate added, this winning on new levels. We’re not done yet, though…
4) Chill them in the fridge for about 30 minutes.
Serve!
Learn more
For those interested in some of the science of what we have going on today:
- Make The Heart-Healthiest Coffee ← this is about cafestol content and why instant is heart-healthiest (alas)
- The Bitter Truth About Coffee (Or Is It) ← this is about the health benefits (and some risks, but mostly benefits) of coffee
- Why You Should Diversify Your Nuts ← almonds are a top-tier choice, but other nuts are good too! This recipe could work well with hazelnuts, for example (we wouldn’t call it “tiramisu crunch bites” in that case, though, since the flavor profile would change)
- Which Sugars Are Healthier, And Which Are Just The Same? ← for any worrying “aren’t dates sugary, though?”
Enjoy!
Share This Post
-
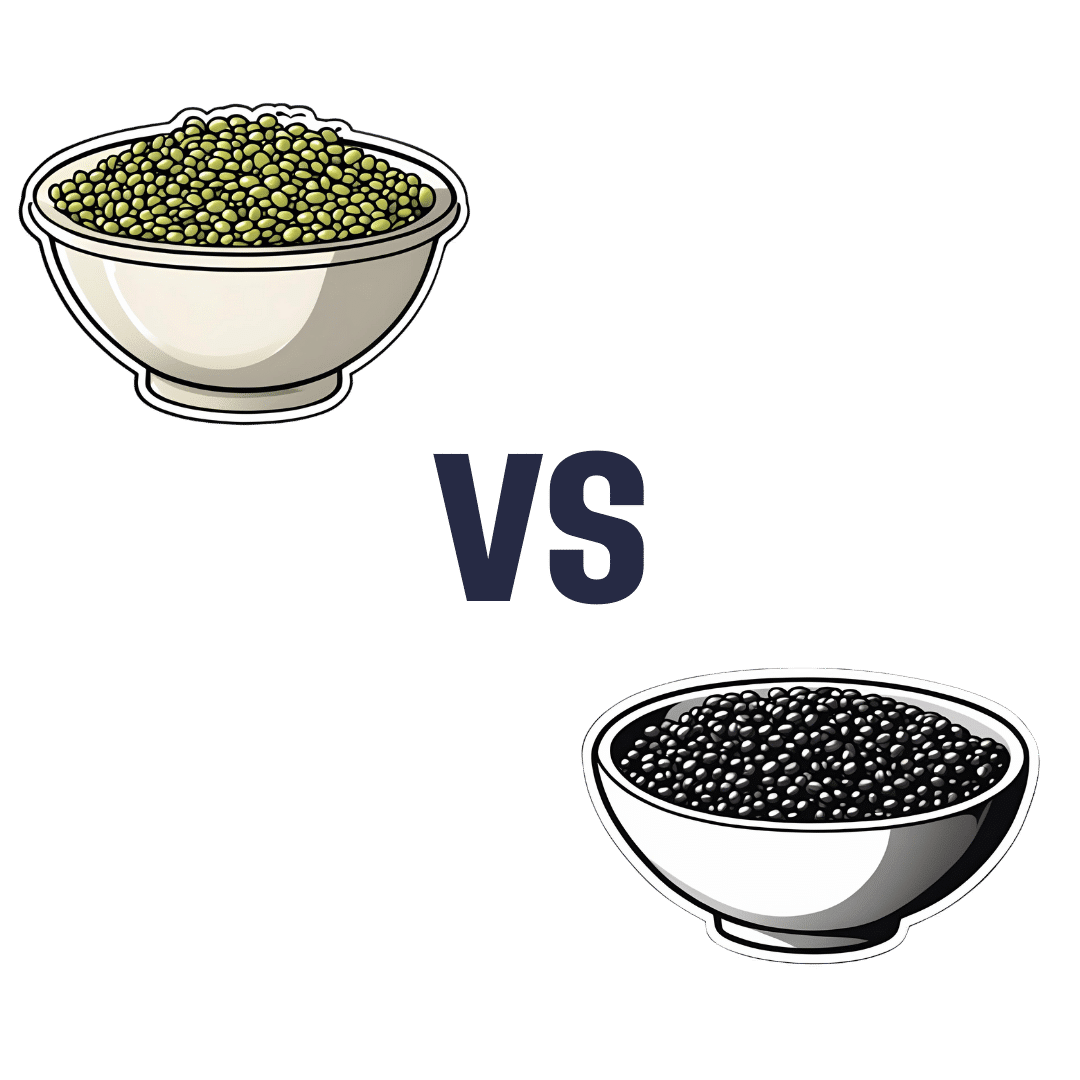
Mung Beans vs Black Gram – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mung beans to black gram, we picked the black gram.
Why?
Both are great, and it was close!
In terms of macros, the main difference is that mung beans have slightly more fiber, while black gram has slightly more protein. So, it comes down to which we prioritize out of those two, and we’re going to call it fiber and thus hand the win in this category to mung beans—but it’s very close in either case.
In the category of vitamins, mung beans have more of vitamins B1, B6, and B9, while black gram has more of vitamins A, B2, B3, and B5. They’re equal on vitamins C, E, K, and choline. So, a marginal victory by the numbers for black gram here.
When it comes to minerals, mung beans have more copper and potassium, while black gram has more calcium, iron, magnesium, manganese, and phosphorus. They’re equal on selenium and zinc. Another win for black gram.
Adding up the sections makes for an overall win for black gram, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
Related Posts
-
How To Know When You’re Healing Emotionally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The healing process can be humbling but rewarding, leading to deep fulfillment and inner peace. Discomfort in healing can be part of growth and self-integration. Because of that, progress sometimes looks and/or feels like progress… And sometimes it doesn’t. Here’s how to recognize it, though:
Small but important parts of a bigger process
Nine signs indicating you are healing:
- Allowing emotions: you acknowledge and process both negative and positive emotions instead of suppressing them.
- Improved boundaries: you improve at expressing and maintaining boundaries, overcoming fear of rejection, guilt, and shame.
- Acceptance of past: you accept difficult past experiences and their impact, reducing their hold over you.
- Less reactivity: you become less reactive and more thoughtful in responses, practicing emotional self-regulation.
- Non-linear healing: you understand that healing involves ups and downs and isn’t a straightforward journey.
- Stepping out of your comfort zone: you start taking brave steps that previously induced fear or anxiety.
- Handling disappointments: you accept setbacks and respond to them healthily, without losing motivation.
- Inner peace: you develop a sense of wholeness, and forgiveness for yourself and others, reducing self-sabotage.
- Welcoming support: you become more open to seeking and accepting help, moving beyond pride and shame.
In short: healing (especially the very first part: accepting that something needs healing) can be uncomfortable but lead to much better places in life. It’s okay if healing is slow; everyone’s journey is different, and doing your best is enough.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Why You Can’t Just “Get Over” Trauma
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Language Fluency Beats General Intelligence & Memory For Longevity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
And no, it doesn’t have to be a second language, although that helps a lot:
An Underrated Tool Against Alzheimer’s ← you don’t even have to learn the second language to a high level, to benefit
Rather, what we’re talking about today is your first language fluency. So, for most of our readers, English. For the study participants it was German, because this was a German research team using data from the German population.
The Berlin Aging Study
Previous research has linked intelligence to longevity, but intelligence comprises multiple traits. So, what’s most important? Memory? General intelligence? Nope. Language fluency!
Let’s clarify something before we continue: “fluency” does not, in linguistics, mean what most people use it to mean. It’s not about the size of one’s overall knowledge of the language (e.g. vocabulary size), but rather, it is about one’s ability to speak and/or write fluently—literally, fluently means “flowingly”, i.e. without undue hesitation or difficulty.
The study used data from the Berlin Aging Study, which tracked 516 people aged 70–105 from 1989 onwards.
Researchers assessed four cognitive abilities, with two kinds of tests for each of:
- Verbal fluency (detailed description below)
- Perceptual speed (pattern-recognition speed)
- Verbal knowledge (vocabulary size)
- Episodic memory (personal memory recall)
General intelligence, meanwhile, was assessed as “the average of those 8 scores”.
The two tests for the cognitive ability of “verbal fluency” were:
Categories
Participants had to name as many different animals as possible within 90 seconds. Their answers were subsequently rated for correctness by two independent research assistants, to assure that noticed or unnoticed repetitions, wrong categories, and morphological variants were not coded as correct.
Word beginnings
Participants were asked to name as many different real words starting with the letter s as possible within 90 seconds. The named words were rated for correctness by two independent research assistants to avoid considering repetitions, morphological variants, and wrong words as correct.
You can read about these and the other tests for the other cognitive abilities, in the paper itself:
Verbal Fluency Selectively Predicts Survival in Old and Very Old Age ← if you’re looking for the test descriptions, scroll to “Method” and then scroll past the table, and you’ll see the test descriptions
They found that of all these metrics, only the two verbal fluency tests (and none of the other tests) showed a significant link to longevity.
Why this is important
Although the study does not prove causality (it could be that people who are predisposed to live longer for other reasons are more verbally fluent because of some common factor that influences both language fluency and longevity), it seems as good a reason as any to develop and maintain language fluency.
This builds on what was found in “The Nun Study“, that followed a convent of nuns (because they are a very homogenous sample in terms of occupation, location, diet, routine, etc, so a lot of confounding factors were already controlled-for) and made numerous major discoveries about things that impact aging (including the relevance of the APOE4 gene! That was The Nun Study).
When it came to nuns and language…
Based on the autobiographies written by the nuns in their youth upon taking their vows, there were two factors that were later correlated with not getting dementia:
- Longer sentences
- Positive outlook
- “Idea density”
That latter item means the relative linguistic density of ideas and complexity thereof, and the fluency and vivacity with which they were expressed (this was not a wishy-washy assessment; there was a hard-science analysis to determine numbers).
Want to spruce up yours? You might like to check out:
Reading, Better: Reading As A Cognitive Exercise
…for specific, evidence-based ways to tweak your reading to fight cognitive decline.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Want the health benefits of strength training but not keen on the gym? Try ‘exercise snacking’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The science is clear: resistance training is crucial to ageing well. Lifting weights (or doing bodyweight exercises like lunges, squats or push-ups) can help you live independently for longer, make your bones stronger, reduce your risk of diseases such as diabetes, and may even improve your sleep and mental health.
But not everyone loves the gym. Perhaps you feel you’re not a “gym person” and never will be, or you’re too old to start. Being a gym-goer can be expensive and time-consuming, and some people report feeling unwelcome or awkward at the gym.
The good news is you don’t need the gym, or lots of free time, to get the health benefits resistance training can offer.
You can try “exercise snacking” instead.
Pressmaster/Shutterstock What is exercise snacking?
Exercise snacking involves doing multiple shorter bouts (as little as 20 seconds) of exercise throughout the day – often with minimal or no equipment. It’s OK to have several hours of rest between.
You could do simple bodyweight exercises such as:
- chair sit-to-stand (squats)
- lunges
- box step-ups
- calf raises
- push-ups.
Exercise snacking like this can help improve muscle mass, strength and physical function.
It’s OK to hold onto a nearby object for balance, if you need. And doing these exercises regularly will also improve your balance. That, in turn, reduces your risk of falls and fractures.
OK I have done all those, now what?
Great! You can also try using resistance bands or dumbbells to do the previously mentioned five exercises as well as some of the following exercises:
When using resistance bands, make sure you hold them tightly and that they’re securely attached to an immovable object.
Exercise snacking works well when you pair it with an activity you do often throughout the day. Perhaps you could:
- do a few extra squats every time you get up from a bed or chair
- do some lunges during a TV ad break
- chuck in a few half squats while you’re waiting for your kettle to boil
- do a couple of elevated push-ups (where you support your body with your hands on a chair or a bench while doing the push-up) before tucking into lunch
- sneak in a couple of calf raises while you’re brushing your teeth.
Exercise snacking involves doing multiple shorter bouts (as little as 20 seconds) of exercise throughout the day. Cavan-Images/Shutterstock What does the evidence say about exercise snacking?
One study had older adults without a history of resistance training do exercise snacks at home twice per day for four weeks.
Each session involved five simple bodyweight exercises (chair sit-to-stand, seated knee extension, standing knee bends, marching on the spot, and standing calf raises). The participants did each exercise continuously for one minute, with a one-minute break between exercises.
These short and simple exercise sessions, which lasted just nine minutes, were enough to improve a person’s ability to stand up from a chair by 31% after four weeks (compared to a control group who didn’t exercise). Leg power and thigh muscle size improved, too.
Research involving one of us (Jackson Fyfe) has also shown older adults found “exercise snacking” feasible and enjoyable when done at home either once, twice, or three times per day for four weeks.
Exercise snacking may be a more sustainable approach to improve muscle health in those who don’t want to – or can’t – lift heavier weights in a gym.
A little can yield a lot
We know from other research that the more you exercise, the more likely it is you will keep exercising in future.
Very brief resistance training, albeit with heavier weights, may be more enjoyable than traditional approaches where people aim to do many, many sets.
We also know brief-and-frequent exercise sessions can break up periods of sedentary behaviour (which usually means sitting too much). Too much sitting increases your risk of chronic diseases such as diabetes, whereas exercise snacking can help keep your blood sugar levels steady.
Of course, longer-term studies are needed. But the evidence we do have suggests exercise snacking really helps.
Just a few short exercise sessions can do you a world of good. eggeegg/Shutterstock Why does any of this matter?
As you age, you lose strength and mass in the muscles you use to walk, or stand up. Everyday tasks can become a struggle.
All this contributes to disability, hospitalisation, chronic disease, and reliance on community and residential aged care support.
By preserving your muscle mass and strength, you can:
- reduce joint pain
- get on with activities you enjoy
- live independently in your own home
- delay or even eliminate the need for expensive health care or residential aged care.
What if I walk a lot – is that enough?
Walking may maintain some level of lower body muscle mass, but it won’t preserve your upper body muscles.
If you find it difficult to get out of a chair, or can only walk short distances without getting out of breath, resistance training is the best way to regain some of the independence and function you’ve lost.
It’s even more important for women, as muscle mass and strength are typically lower in older women than men. And if you’ve been diagnosed with osteoporosis, which is more common in older women than men, resistance exercise snacking at home can improve your balance, strength, and bone mineral density. All of this reduces the risk of falls and fractures.
You don’t need heavy weights or fancy equipment to benefit from resistance training.
So, will you start exercise snacking today?
Justin Keogh, Associate Dean of Research, Faculty of Health Sciences and Medicine, Bond University and Jackson Fyfe, Senior Lecturer, Strength and Conditioning Sciences, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: