Exercise and Fat Loss (5 Things You Need To Know)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to think “I’ll eat whatever; I can always burn it off later”, and if it’s an odd occasion, then that’s fine; indeed, a fit and healthy body can usually weather small infrequent dietary indiscretions easily. But…
You can’t outrun a bad diet
Exercise can create a calorie deficit, but over time, the body balances this out by adjusting one’s metabolism, leading to a plateau in fat loss—and as you might know, you can’t out-exercise a bad diet. On the contrary, dietary adjustments are crucial for fat loss and body recomposition.
About that calorie deficit in the first place, by the way: extreme calorie deficits through exercise alone can lead to muscle loss, reduced energy, and thus sabotage long-term fat loss because having muscle mass increases one’s base metabolic rate (while having fat does not).
Another thing to bear in mind about exercise is that longer workouts without adequate rests in between can cause burnout, injury, or weight gain due to the body doing its best to conserve energy.
So, a good diet is a necessary condition for both muscle maintenance and fat loss.
Five Key Diet Tips:
- Include foods you love: don’t feel obliged cut out favorite foods that are a little unhealthy; incorporate them in moderation for sustainability.
- Keep adjustments small: avoid making drastic dietary changes all at once; make gradual tweaks to prevent feeling deprived.
- Prioritize protein: focus on including a protein source in every meal to increase satiety and aid in muscle building.
- Avoid low-calorie diets: drastically cutting calories can lead to muscle loss, metabolic adaptation, and overeating.
- Embrace diet evolution: changes may not feel sustainable at first, but adjustments over time help achieve long-term balance. You can always “adjust course” as you go.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Are You A Calorie-Burning Machine?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Ways To Delay Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Colin Rose; he is a Senior Associate of the Royal Society of Medicine. He’s also a main contributor to EduScience, a program funded by the E.U. which is designed to enhance the teaching and learning of science in schools in Europe.
His most recent work has been about aging—and how to delay it. We also reviewed his latest book, here:
Delay Ageing – by Dr. Colin Rose
So, what does he want us to know? The key lies in his compilation of ten ways in which we age on a cellular level, and what we can to do slow each one of those:
Damage to DNA accumulates
While DNA can get damaged without any external stimulus to cause that, there are a lot of modifiable factors that we can do to reduce DNA damage. The list is easy: if it causes cancer, it causes aging.
Thus, check out: Stop Cancer 20 Years Ago
Cells become senescent
Our cells are replaced all the time; some sooner than others, but all of them at some point. The problem occurs when cells are outliving their usefulness. If a cell becomes completely immortal, that is cancer, but happily most don’t. Nevertheless, having senescent (aging) cells in the body means that those senescent cells are what get copied forwards by mitosis, and our DNA becomes like a photocopy of a tattered old photocopy of a tattered old photocopy. Which, needless to say, is not good for our health. So, the best thing to do is to kill them earlier:
Yes, really: Fisetin: The Anti-Aging Assassin
Mitochondria become dysfunctional
Without properly functional mitochondria, no living human cell can do its job properly.
Options: 7 Ways To Boost Mitochondrial Health To Fight Disease
Beneficial genes are switched off, harmful genes are on
It’s easy to think of our genes as being immutable, but epigenetics means that our environment (amongst other factors) can mean that our gene expression changes.
Imagine it this way: your genes are a set of instructions for your body. However, your body will act or not on those instructions, depending on other factors. Hormones often play a big part in this; for example sex hormones tell the body which set of genetic instructions to read (and thus what kind of body to build/rebuild), and cortisol or oxytocin can tell the body which set of contingency plans to activate or suppress (respectively). A milder example is gray hair; genes have the program for it, but many other factors inform the body when, if, and how to do it.
Of more concern when it comes to aging is what goes on with more critical systems, such as the brain, in which the aforementioned DNA damage can cause unhelpful instructions to get interpreted, resulting in epigenetic changes that in turn facilitate age-related degeneration.
As to what can be done, see : Klotho: Unzipping The Genes Of Aging?
Stem cells become exhausted
Stem cells can become different kinds of cells, and thus they’re very useful for maintaining a healthy body. However, they get depleted with age. We can slow down the rate of loss, though; for example, intermittent fasting can help:
Per Dr. Li’s 5 Ways To Beat Cancer (And Other Diseases)
And for more detail, see:
Doctor’s Tip: Regeneration (stem cells) — one of your body’s five defense systems
(complete with lists of foods to eat or avoid for stem cell health)
Cells fail to communicate properly
Cells need to talk to each other constantly, to continue doing their jobs. We are one big organism, after all, and not a haphazard colony of the countless cells that constitute such. However, cell signalling gets worse with age, which in turn precipitates others age-related problems. Fortunately, there are nutrients that can improve cellular communication.
For example: PS, We Love You ← this is about phosphatidylserine, also called “PS”
Telomeres become shorter
These protective caps on our DNA suffer the wear-and-tear so that our DNA doesn’t have to. However, as they get shorter, the DNA can start suffering damage. For this reason, telomere length is considered one of the most “Gold Standard” markers of cellular aging.
Here’s what can be done for that: The Stress Prescription (Against Aging!)
The body fails to sense nutritional intake properly
This is mostly about insulin signalling (though problems can occur in other systems too, but we only have so much room here), so it’s important to take care of that.
See: Turn Back The Clock On Insulin Resistance
Proteins accumulate errors
This is due to DNA damage, of course, but there are specific things that can reduce protein error accumulation; see for example:
A quick fix – preventing protein errors extends lifespan
See also: Rapamycin Can Slow Aging By 20% (But Watch Out)
The microbiome becomes unbalanced
We at 10almonds often mention that gut health affects pretty much every other kind of health, and it’s true for aging as well. So, take care of that microbiome!
Here’s a primer: Gut Health 101
Want to know more about delaying aging beyond the cellular level?
Check out: Age & Aging: What Can (And Can’t) We Do About It?
Take care!
Share This Post
-
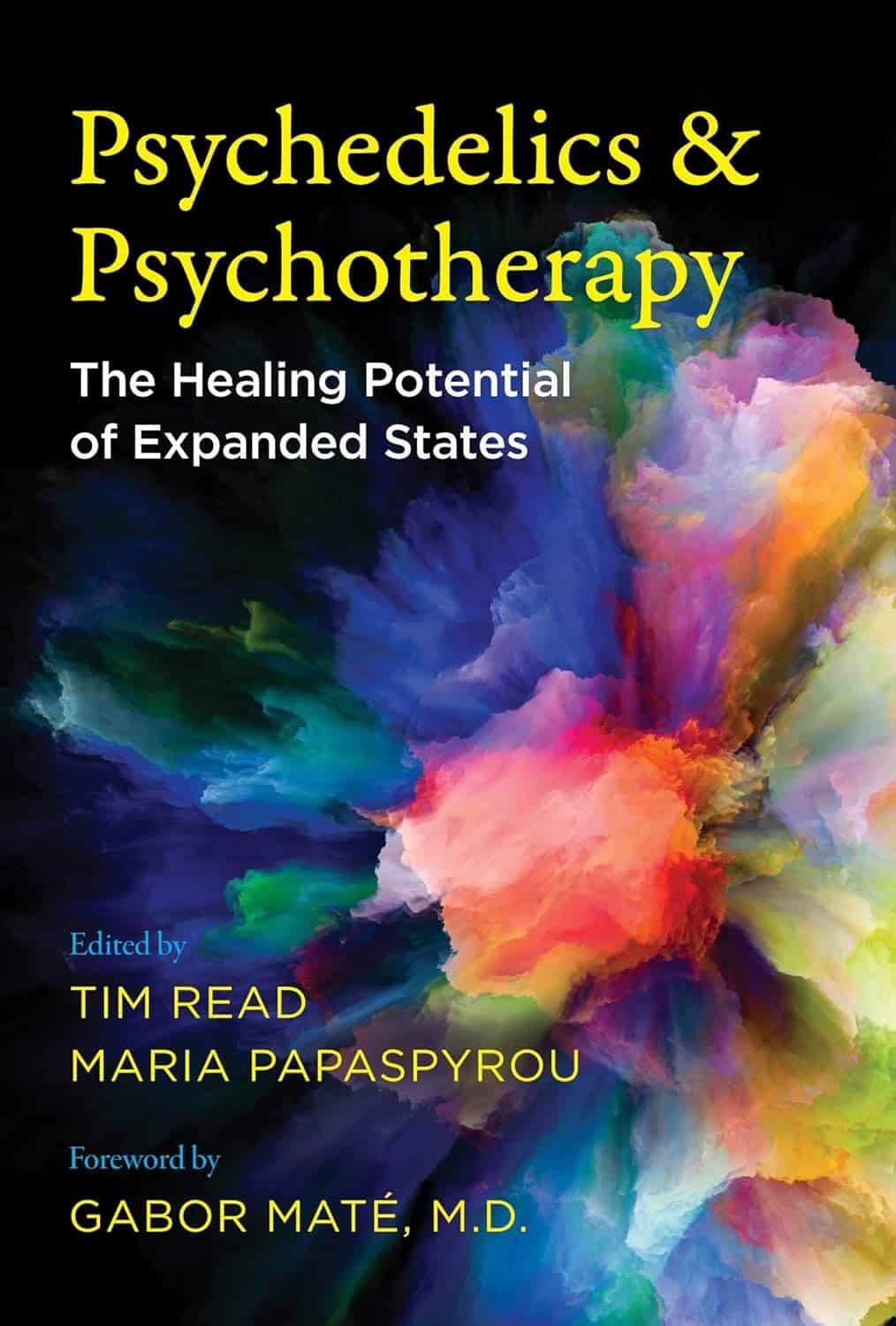
Psychedelics and Psychotherapy – Edited by Dr. Tim Read & Maria Papaspyrou
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A quick note on authorship, first: this book is edited by the psychiatrist and psychotherapist credited above, but after the introductory section, the rest of the chapters are written by experts on the individual topics.As such, the style will vary somewhat, from chapter to chapter.
What this book isn’t: “try drugs and feel better!”
Rather, the book explores the various ways in which assorted drugs can help people to—even if just briefly—shed things they didn’t know they were carrying, or otherwise couldn’t put down, and access parts of themselves they otherwise couldn’t.
We also get to read a lot about the different roles the facilitator can play in guiding the therapeutic process, and what can be expected out of each kind of experience. This varies a lot from one drug to another, so it makes for very worthwhile reading, if that’s something you might consider pursuing. Knowledge makes for much more informed choices!
Bottom line: if you’re curious about the therapeutic potential of psychedelics, and want a reference that’s more personal than dry clinical studies, but still more “safe and removed” than diving in by yourself, this is the book for you.
Click here to check out Psychedelics and Psychotherapy, and expand your understanding!
Share This Post
-
How To Keep Your Mind From Wandering
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether your mind keeps wandering more as you get older, or you’re a young student whose super-active brain is more suited to TikTok than your assigned reading, sustained singular focus can be a challenge for everyone—and yet (alas!) it remains a required skill for so much in life.
Today’s edition of 10Almonds presents a nifty trick to get yourself through those tasks! We’ll also be taking some time to reply to your questions and comments, in our weekly interactive Q&A.
First of all though, we’ve a promise to make good on, so…
How To Stay On The Ball (Or The Tomato?) The Easy Way
For most of us, we face three main problems when it comes to tackling our to-dos:
- Where to start?
- The task seems intimidating in its size
- We get distracted and/or run out of energy
If you’re really not sure where to start, we recommended a powerful tool in last Friday’s newsletter!
For the rest, we love the Pomodoro Technique:
- Set a timer for 25 minutes, and begin your task.
- Keep going until the timer is done! No other tasks, just focus.
- Take a 5-minute break.
- Repeat
This approach has three clear benefits:
- No matter the size of the task, you are only committing to 25 minutes—everything is much less overwhelming when there’s an end in sight!
- Being only 25 minutes means we are much more likely to stay on track; it’s easier to defer other activities if we know that there will be a 5-minute break for that soon.
- Even without other tasks to distract us, it can be difficult to sustain attention for long periods; making it only 25 minutes at a time allows us to approach it with a (relatively!) fresh mind.
Have you heard that a human brain can sustain attention for only about 40 minutes before focus starts to decline rapidly?
While that’s been a popular rationale for school classroom lesson durations (and perhaps coincidentally ties in with Zoom’s 40-minute limit for free meetings), the truth is that focus starts dropping immediately, to the point that one-minute attention tests are considered sufficient to measure the ability to focus.
So a 25-minute Pomodoro is a more than fair compromise!
Why’s it called the “Pomodoro” technique?
And why is the 25-minute timed work period called a Pomodoro?
It’s because back in the 80s, university student Francesco Cirillo was struggling to focus and made a deal with himself to focus just for a short burst at a time—and he used a (now “retro” style) kitchen timer in the shape of a tomato, or “pomodoro”, in Italian.
If you don’t have a penchant for kitsch kitchenware, you can use this free, simple Online Pomodoro Timer!
(no registration/login/download necessary; it’s all right there on the web page)
Share This Post
Related Posts
-
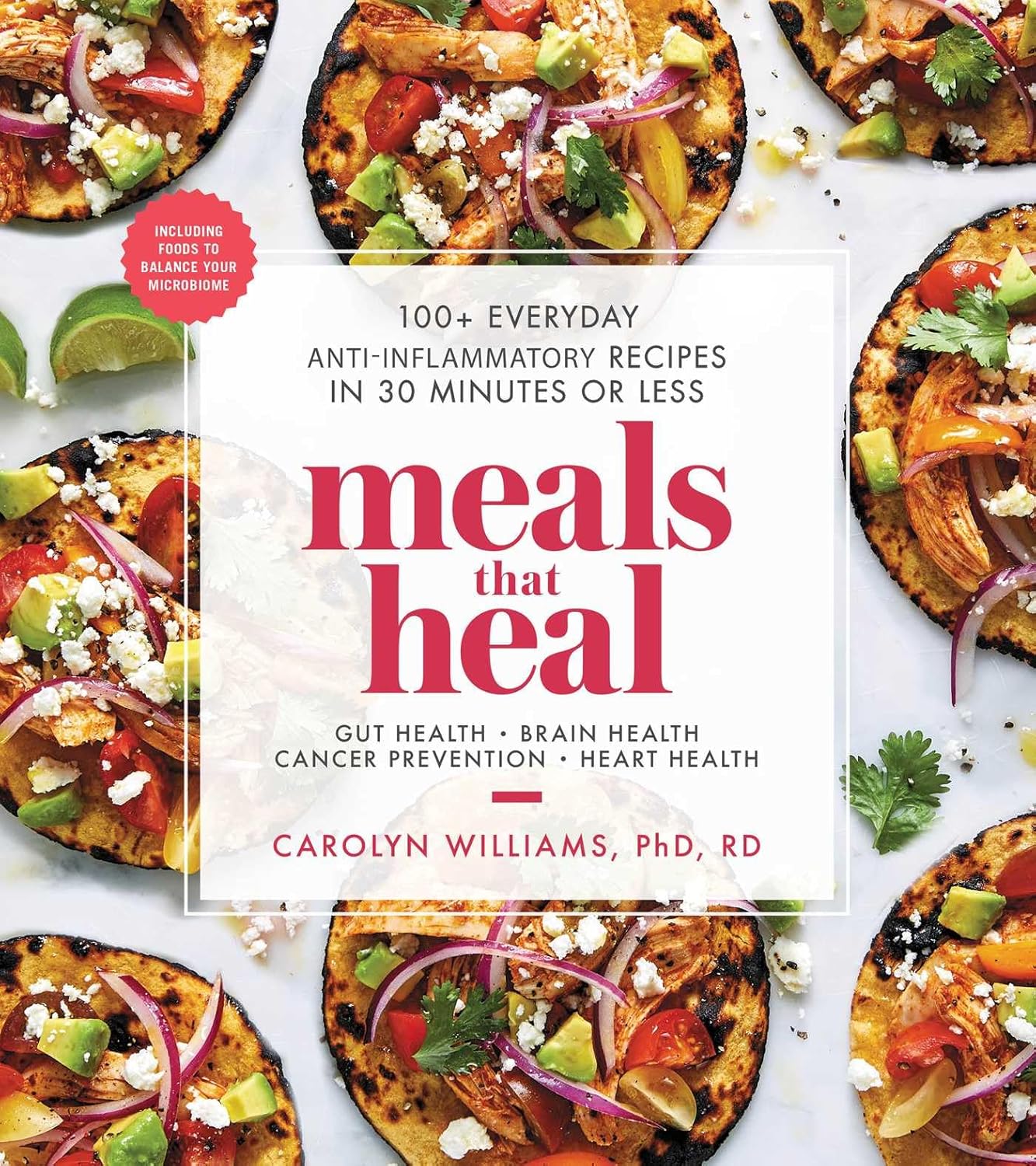
Meals That Heal – by Dr. Carolyn Williams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Inflammation is implicated as a contributory or casual factor in almost all chronic diseases (and still exacerbates the ones in which it’s not directly implicated causally), so if there’s one area of health to focus on with one’s diet, then reducing inflammation is a top candidate.
This book sets about doing exactly that.
You may be wondering whether, per the book’s subtitle, they can really all be done in 30 minutes or under. The answer is: no, not unless you have a team of sous-chefs to do all the prep work for you, and line up everything mise-en-place style for when you start the clock. If you do have that team of sous-chefs working for you, then you can probably do most of them in under 30 minutes. If you don’t have that team, then budget about an hour in total, sometimes less, sometimes more, depending on the recipe.
The recipes themselves are mostly Mediterranean-inspired, though you might want to do a few swaps where the author has oddly recommended using seed oils instead of olive oil, or plant milk in place of where she has used dairy milk in a couple of “recipes” for smoothies. You might also want to be a little more generous with the seasonings, if you’re anything like this reviewer.
Bottom line: if you’re looking for an anti-inflammatory starter cookbook, you could do worse than this. You could probably do better, too, such as starting with The Inflammation Spectrum – by Dr. Will Cole.
Alternatively, click here if you want to check out Meals That Heal, and dive straight in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
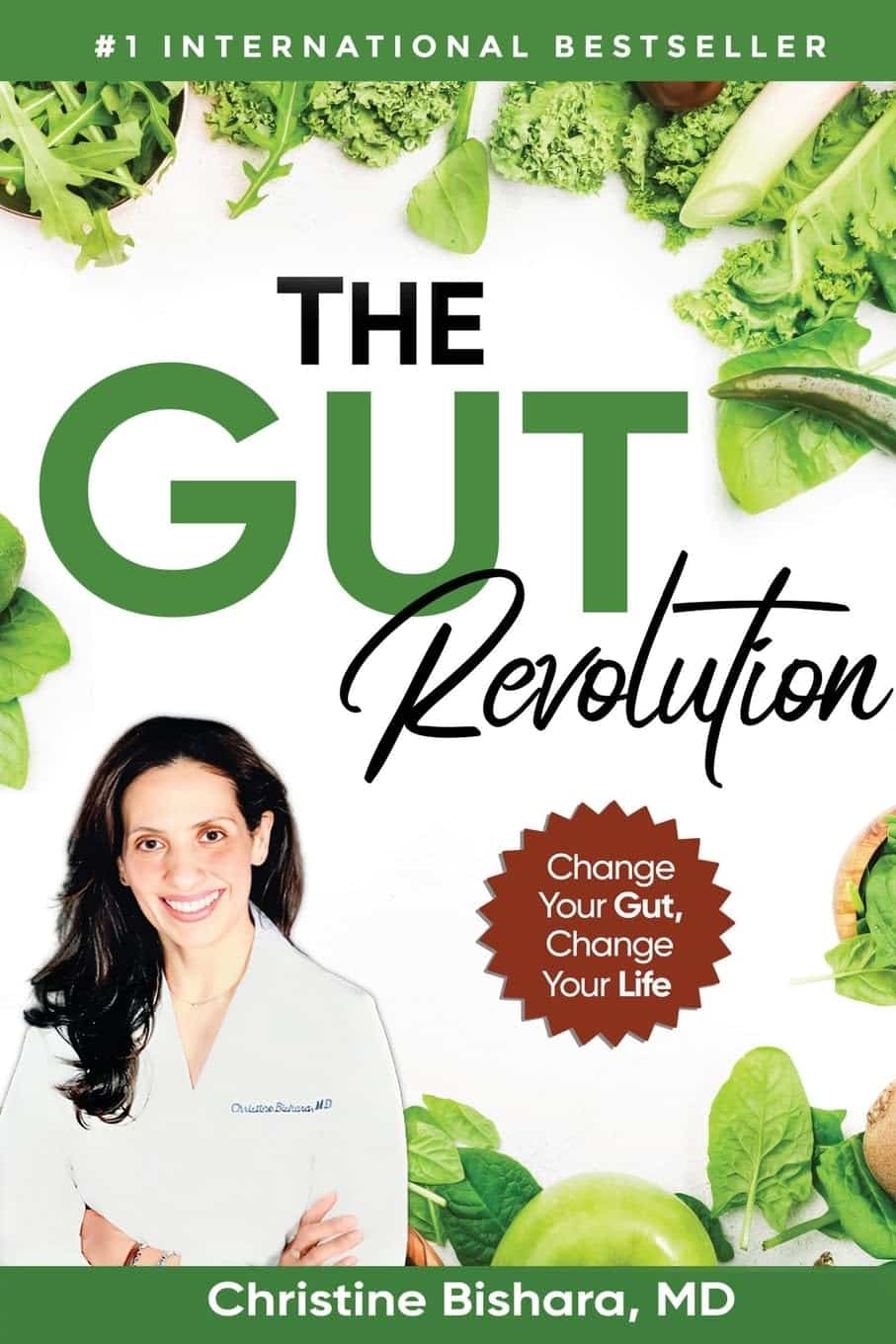
The Gut Revolution – by Dr. Christine Bishara
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be wondering: what sets this apart from other books about gut health?
And one answer is: the author discusses her own published study, with regard to the connection between a deficiency in Bifidobacterium sp., and COVID infection risk/severity. However, this is not an entire book to say “supplement Bifidobacterium sp.”; rather, there are many other things at hand too.
And indeed, supplementing with probiotics will be useless if your gut is not an environment conducive to them thriving. If you take probiotics on an otherwise “Standard American Diet”, then this is approximately the equivalent of paradropping firefighters naked into a raging fire. It will not help. It isn’t the thought that counts.
Instead, Dr. Bishara talks us through what is required for beneficial gut bacteria to thrive, and how to go about making our gut an ideal place for them. In return, they will produce important biochemical metabolites for us, they will improve our immune response, regulate our emotions, help us maintain a healthy weight, heal our skin, and make us smell nice too. In short, they’re a trillions-strong clean-up and maintenance team, if only we treat our workforce well.
Another thing that Dr. Bishara brings of value here that’s not found in a lot of gut health books is the benefits (for gut health) of intermittent fasting, and specifically, a very useful timeline of what happens when, to ensure we do not sabotage our efforts by breaking our fast too early or too late.
The style is easy-reading pop-science, albeit with scientific references throughout for those who want to delve deeper.
Bottom line: this is a gut health book that stands out from the crowd in several ways, and is well worth the investment of reading it!
Click here to check out Gut Revolution, and help yours to help you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Actually Get Abs (10 Annoying Tips That Work!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cori Lefkowitz, of “Strong At Any Age”, advises…
The method
It may not be fun, but here’s what she finds works:
- Be boring: stick to a simple, repetitive diet to track progress easily, and make hitting macros simpler.
- Cut back on protein bars: processed protein bars are calorie-dense but not filling (due to their small volume), so limit them, especially when trying to get lean.
- Stop daily fluctuations: she advises to be precise with macros and calories daily, not just weekly, to see consistent results.
- Focus on fiber: aim for 25–30g of fiber daily to improve gut health, reduce cravings, and maintain health while cutting fat.
- Get 30–40g of protein per meal: ensure each meal has enough protein to fuel muscle growth and support overall body function.
- Prioritize carbs around workouts: eat carbs before and after training to fuel performance, aid muscle repair, and maintain lean mass.
- Take diet breaks: incorporate 1–2 week maintenance phases to prevent metabolic adaptation, maintain muscle, and thus stay consistent in the long-term.
- Be careful with fat burners & preworkout: these can harm sleep, recovery, and long-term fat loss; opt for natural dietary energy sources instead.
- Don’t set-and-forget: regularly assess and adjust your diet and macros as your body and lifestyle change.
- “Suck it up, buttercup”: fat loss requires persistence, discipline, and pushing through tough moments when you feel like quitting.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Is A Visible Six-Pack Obtainable Regardless Of Genetic Predisposition?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: