The Vagus Nerve’s Power for Weight Loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Arun Dhir is a university lecturer, a gastrointestinal surgeon, an author, and a yoga and meditation instructor, and he has this to say:
Gut feelings
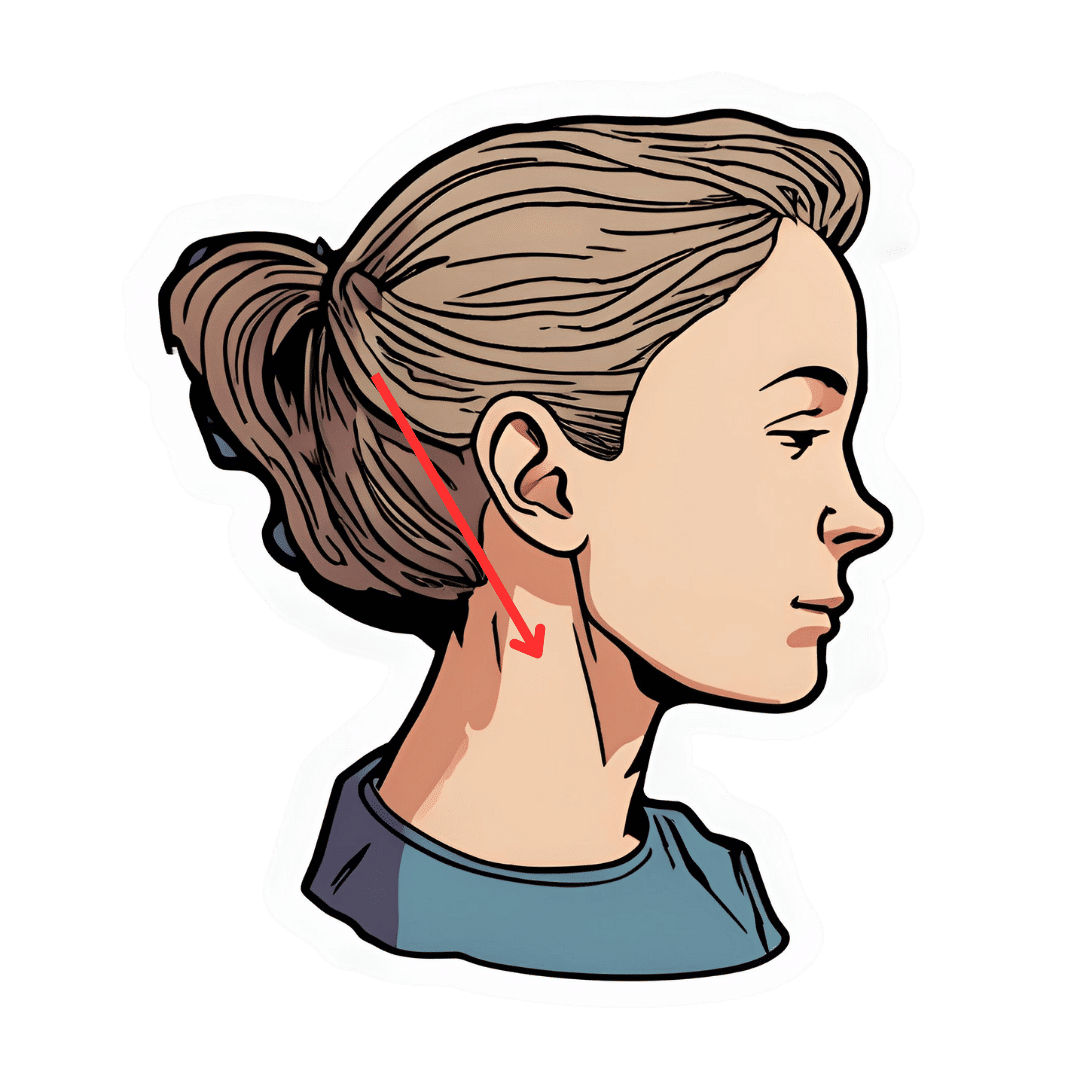
The vagus nerve is the 10th cranial nerve, also known as “vagus” (“the wanderer”), because it travels from the brain to many other body parts, including the ears, throat, heart, respiratory system, gut, pancreas, liver, and reproductive system. It’s no surprise then, that it plays a key role in brain-gut communication and metabolism regulation.
The vagus nerve is part of the parasympathetic nervous system, responsible for rest, digestion, and counteracting the stress response. Most signals through the vagus nerve travel from the gut to the brain, though there is communication in both directions.
You may be beginning to see how this works and its implications for weight management: the vagus nerve senses metabolites from the liver, pancreas, and small intestine, and regulates insulin production by stimulating beta cells in the pancreas, which is important for avoiding/managing insulin resistance and metabolic syndrome in general.
Dr. Dhir cites a study in which vagus nerve stimulation (originally used for treating epilepsy and depression) was shown to cause unintentional weight loss (6-11%) in patients, revealing a link to weight management. Of course, that is quite a specific sample, so more research is needed to say for sure, but because the principle is very sound and the mechanism of action is clear, it’s not being viewed as a controversial conclusion.
As for how get these benefits, here are seven ways:
- Cold water on the face: submerge your face in cold water in the morning while holding water in your mouth, or cover your face with a cold wet washcloth (while holding your breath please; no need to waterboard yourself!), which activates the “mammalian dive response” in which your body activates the parasympathetic nervous system in order to remain calm and thus survive for longer underwater
- Alternate hot and cold showers: switch between hot and cold water during showers for 10-second intervals; this creates eustress and activates the process of hormesis, improving your overall stress management and reducing any chronic stress response you may otherwise have going on
- Humming and gargling: the vibrations in the throat stimulate the nearby vagus nerve
- Deep breathing (pranayama): yoga breathing exercises, especially combined with somatic exercises such as the sun salutation, can stimulate the vagus nerve
- Intermittent fasting: helps recalibrate the metabolism and indirectly improves vagus nerve function
- Massage and acupressure: stimulates lymphatic channels and the vagus nerve
- Long walks in nature (“forest bathing”): helps trigger relaxation in general
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Vagus Nerve (And How You Can Make Use Of It)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Death by Sitting – by Carolyne Thompson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be wondering: is this a lot of words to say “sit down less”?
And the answer is: there’s a lot more in here than that. Of course, yes, “sit down less” is an important take-away, but there’s a lot about the specific problems caused by sitting in chairs, the health risks are that are increased and how, and the early warning signs to watch out for.
After these chapters of woe, most of the book is given over to solutions; about taking standing and walking breaks, tying movement to productivity, why exercise alone is not enough to offset the damage of sitting, relearning ergonomic posture in the context of mitigating the harm, psychological shifts to break the habit of sitting, redefining social norms around sitting and socializing, rewiring one’s body and retraining better movements as well as postures to always immediately move out of if one finds oneself in, and much much more.
The style is light and easy to read, while still including scientific research as appropriate along with practical, actionable advice.
Bottom line: if you’d like to do better for your body than slowly killing it for however many hours a day, then this book has a wealth of advice far beyond the obvious (but important!) “sit less”.
Share This Post
-
Starfruit vs Soursop – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing starfruit to soursop, we picked the soursop.
Why?
First, by starfruit, we also mean carambola, which is a different name for the same fruit, and by soursop we also mean graviola/guyabano/guanábana, which are different namers for the same fruit. Now, as for their health qualities:
In terms of macros, the soursop has more carbs and fiber, the ratio of which also give it the lower glycemic index. So, a win for soursop here.
When it comes to vitamins, starfruit has more of vitamins A, B5, C, and E, while soursop has more of vitamins B1, B2, B3, B6, B7, B9, and K. Another win for soursop.
In the category of minerals, starfruit has slightly more copper, manganese, and zinc, while soursop has much more calcium, iron, magnesium, phosphorus, and potassium. One more win for soursop!
Adding up the sections makes for a clear and overwhelming win for soursop, but let’s address to quick safety considerations while we’re here:
- Soursop extract has been claimed to be an effective cancer treatment. It isn’t. There is no evidence for this at all; just one unscrupulous company that spread the claims.
- Soursop contains annonacin, a neurotoxin. That sounds scary, but much like with apple seeds and cyanide, the quantities you’d have to consume to suffer ill effects are absurd. Remember how capsaicin (as found in hot peppers) is also a neurotoxin, too and has many health benefits. Humans have a long and happy tradition of enjoying things that are toxic at high doses, but in small doses are neutral or even beneficial. Pretty much all things we can consume (including oxygen, and water) are toxic at sufficient doses.
In short, both of these fruits are fine and good, neither will treat cancer, but both will help to keep you in good health. As for nutritional density, the soursop wins in every category.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← soursop has no special cancer treatment properties, but actual evidence shows these fruits are beneficial (being good as a preventative, and also definitely a worthy adjunct to—but not a replacement for—mainstream anticancer therapies if you have cancer).
Take care!
Share This Post
-
Protein Immune Support Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to get enough protein from a salad, without adding meat? Cashews and chickpeas have you more than covered! Along with the leafy greens and an impressive array of minor ingredients full of healthy phytochemicals, this one’s good for your muscles, bones, skin, immune health, and more.
You will need
- 1½ cups raw cashews (if allergic, omit; the chickpeas and coconut will still carry the dish for protein and healthy fats)
- 2 cans (2x 14oz) chickpeas, drained
- 1½ lbs baby spinach leaves
- 2 large onions, finely chopped
- 3 oz goji berries
- ½ bulb garlic, finely chopped
- 2 tbsp dessicated coconut
- 1 tbsp dried cumin
- 1 tbsp nutritional yeast
- 2 tsp chili flakes
- 1 tsp black pepper, coarse ground
- ½ tsp MSG, or 1 tsp low-sodium salt
- Extra virgin olive oil, for cooking
Method
(we suggest you read everything at least once before doing anything)
1) Heat a little oil in a pan; add the onions and cook for about 3 minutes.
2) Add the garlic and cook for a further 2 minutes.
3) Add the spinach, and cook until it wilts.
4) Add the remaining ingredients except the coconut, and cook for another three minutes.
5) Heat another pan (dry); add the coconut and toast for 1–2 minutes, until lightly golden. Add it to the main pan.
6) Serve hot as a main, or an attention-grabbing side:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Cashew Nuts vs Coconut – Which is Healthier?
- What Matters Most For Your Heart?
- Beyond Supplements: The Real Immune-Boosters!
- Goji Berries: Which Benefits Do They Really Have?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
Related Posts
-
Seven and a Half Lessons About the Brain – by Dr. Lisa Feldman Barrett
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about neurology before, and we always try to review books that bring something new/different. So, what makes this one stand out?
Dr. Lisa Feldman Barrett, one of the world’s foremost neuroscientists, starts with an overview of how our unusual brain (definitely our species’ defining characteristic) came to be, and then devotes the rest of the book to mostly practical information.
She explains, in clear terms and without undue jargon, how the brain goes about such things as making constant predictions and useful assumptions about our environment, and reports these things to us as facts—which process is usually useful, and sometimes counterproductive.
We learn about how the apparently mystical trait of empathy works, in real flesh-and-blood terms, and why some kinds of empathy are more metabolically costly than others, and what that means for us all.
Unlike many such books, this one also looks at what is going on in the case of “different minds” that operate very dissimilarly to our own, and how this neurodiversity is important for our species.
Critically, she also looks at what else makes our brains stand out, the symphony of “5 Cs” that aren’t often found to the same extent all in the same species: creativity, communication, copying, cooperation, and compression. This latter being less obvious, but perhaps the most important; Dr. Feldman Barrett explains how we use this ability to layer summaries of our memories, perceptions, and assumptions, to allow us to think in abstractions—something that powers much of what we do that separates us from other animals.
Bottom line: if you’d like to learn more about that big wet organ between your ears, what it does for you, and how it goes about doing it, then this book gives a very practical foundation from which to build.
Click here to check out Seven and a Half Lessons about the Brain, and learn more about yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What To Do If Having A Stroke Alone?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Thank you for the video about what to do if you have a heart attack alone, what about what to do if you have a stroke alone?❞
(for anyone who missed that video, here it is)
That’s a good question, especially as stroke risk is rising in the industrialized world in general, and the US in particular.
However, let’s start with the caveat that if you are having a stroke, there’s a good chance you will forget what we are about to say, what with the immediate effects it has on the brain. That said…
The general advice when it comes to looking after someone else who is experiencing a stroke, is, “don’t”.
In other words, call emergency services, and don’t do anything else, e.g:
- don’t give them anything to eat or drink
- don’t give them any medications
- don’t let them go to sleep
- don’t let them talk you out of calling emergency services
- don’t let them drive themselves to hospital
- don’t drive them to hospital yourself either*
*This is for two reasons:
- an ambulance crew has skills and resources that you don’t, and can begin treatment en-route, and also,
- not all hospitals have appropriate resources to treat stroke, so the ambulance crew will know to drive to one that does, instead of driving to a random hospital and hoping for the best
So, flipping this for if it’s you having the stroke, and you’re cognizant enough to remember this:
- do call an ambulance; stay on the line and don’t do anything else unless instructed by the emergency services.
In order to do that, of course it’s important to recognize the symptoms; you probably know these but just in case, the mnemonic is “FAST”:
- Face: is there weakness on one side of their face?
- Arms: if they raise both arms, does one drift downwards?
- Speech: if they speak, is their speech slurred or otherwise unusual?
- Time: to call emergency services
It’s great to not get caught out by surprise, so you might also want to check out:
6 Signs Of Stroke (One Month In Advance)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
No, taking drugs like Ozempic isn’t ‘cheating’ at weight loss or the ‘easy way out’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hundreds of thousands of people worldwide are taking drugs like Ozempic to lose weight. But what do we actually know about them? This month, The Conversation’s experts explore their rise, impact and potential consequences.
Obesity medication that is effective has been a long time coming. Enter semaglutide (sold as Ozempic and Wegovy), which is helping people improve weight-related health, including lowering the risk of a having a heart attack or stroke, while also silencing “food noise”.
As demand for semaglutide increases, so are claims that taking it is “cheating” at weight loss or the “easy way out”.
We don’t tell people who need statin medication to treat high cholesterol or drugs to manage high blood pressure they’re cheating or taking the easy way out.
Nor should we shame people taking semaglutide. It’s a drug used to treat diabetes and obesity which needs to be taken long term and comes with risks and side effects, as well as benefits. When prescribed for obesity, it’s given alongside advice about diet and exercise.
How does it work?
Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1RA). This means it makes your body’s own glucagon-like peptide-1 hormone, called GLP-1 for short, work better.
GLP-1 gets secreted by cells in your gut when it detects increased nutrient levels after eating. This stimulates insulin production, which lowers blood sugars.
GLP-1 also slows gastric emptying, which makes you feel full, and reduces hunger and feelings of reward after eating.
GLP-1 receptor agonist (GLP-1RA) medications like Ozempic help the body’s own GLP-1 work better by mimicking and extending its action.
Some studies have found less GLP-1 gets released after meals in adults with obesity or type 2 diabetes mellitus compared to adults with normal glucose tolerance. So having less GLP-1 circulating in your blood means you don’t feel as full after eating and get hungry again sooner compared to people who produce more.
GLP-1 has a very short half-life of about two minutes. So GLP-1RA medications were designed to have a very long half-life of about seven days. That’s why semaglutide is given as a weekly injection.
What can users expect? What does the research say?
Higher doses of semaglutide are prescribed to treat obesity compared to type 2 diabetes management (up to 2.4mg versus 2.0mg weekly).
A large group of randomised controlled trials, called STEP trials, all tested weekly 2.4mg semaglutide injections versus different interventions or placebo drugs.
Trials lasting 1.3–2 years consistently found weekly 2.4 mg semaglutide injections led to 6–12% greater weight loss compared to placebo or alternative interventions. The average weight change depended on how long medication treatment lasted and length of follow-up.
Higher doses of semaglutide are prescribed for obesity than for type 2 diabetes. fcm82/Shutterstock Weight reduction due to semaglutide also leads to a reduction in systolic and diastolic blood pressure of about 4.8 mmHg and 2.5 mmHg respectively, a reduction in triglyceride levels (a type of blood fat) and improved physical function.
Another recent trial in adults with pre-existing heart disease and obesity, but without type 2 diabetes, found adults receiving weekly 2.4mg semaglutide injections had a 20% lower risk of specific cardiovascular events, including having a non-fatal heart attack, a stroke or dying from cardiovascular disease, after three years follow-up.
Who is eligible for semaglutide?
Australia’s regulator, the Therapeutic Goods Administration (TGA), has approved semaglutide, sold as Ozempic, for treating type 2 diabetes.
However, due to shortages, the TGA had advised doctors not to start new Ozempic prescriptions for “off-label use” such as obesity treatment and the Pharmaceutical Benefits Scheme doesn’t currently subsidise off-label use.
The TGA has approved Wegovy to treat obesity but it’s not currently available in Australia.
When it’s available, doctors will be able to prescribe semaglutide to treat obesity in conjunction with lifestyle interventions (including diet, physical activity and psychological support) in adults with obesity (a BMI of 30 or above) or those with a BMI of 27 or above who also have weight-related medical complications.
What else do you need to do during Ozempic treatment?
Checking details of the STEP trial intervention components, it’s clear participants invested a lot of time and effort. In addition to taking medication, people had brief lifestyle counselling sessions with dietitians or other health professionals every four weeks as a minimum in most trials.
Support sessions were designed to help people stick with consuming 2,000 kilojoules (500 calories) less daily compared to their energy needs, and performing 150 minutes of moderate-to-vigorous physical activity, like brisk walking, dancing and gardening each week.
STEP trials varied in other components, with follow-up time periods varying from 68 to 104 weeks. The aim of these trials was to show the effect of adding the medication on top of other lifestyle counselling.
Trial participants also exercised for 150 minutes a week. Elena Nichizhenova/Shutterstock A review of obesity medication trials found people reported they needed less cognitive behaviour training to help them stick with the reduced energy intake. This is one aspect where drug treatment may make adherence a little easier. Not feeling as hungry and having environmental food cues “switched off” may mean less support is required for goal-setting, self-monitoring food intake and avoiding things that trigger eating.
But what are the side effects?
Semaglutide’s side-effects include nausea, diarrhoea, vomiting, constipation, indigestion and abdominal pain.
In one study these led to discontinuation of medication in 6% of people, but interestingly also in 3% of people taking placebos.
More severe side-effects included gallbladder disease, acute pancreatitis, hypoglycaemia, acute kidney disease and injection site reactions.
To reduce risk or severity of side-effects, medication doses are increased very slowly over months. Once the full dose and response are achieved, research indicates you need to take it long term.
Given this long-term commitment, and associated high out-of-pocket cost of medication, when it comes to taking semaglutide to treat obesity, there is no way it can be considered “cheating”.
Read the other articles in The Conversation’s Ozempic series here.
Clare Collins, Laureate Professor in Nutrition and Dietetics, University of Newcastle
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: