Redcurrants vs Cranberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing redcurrants to cranberries, we picked the redcurrants.
Why?
First know: here we’re comparing raw redcurrants to raw cranberries, with no additives in either case. If you buy jelly made from either, or if you buy dried fruits but the ingredients list has a lot of added sugar and often some vegetable oil, then that’s going to be very different. But for now… Let’s look at just the fruits:
In terms of macros, redcurrants are higher in carbs, but also higher in fiber, and have the lower glycemic index as cranberries have nearly 2x the GI.
When it comes to vitamins, redcurrants have more of vitamins B1, B2, B6, B9, C, K, and choline, while cranberries have more of vitamins A, B5, and E. In other words, a clear win for redcurrants.
In the category of minerals, redcurrants sweep even more convincingly with a lot more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc. On the other hand, cranberries boast a little more manganese; they also have about 2x the sodium.
Both berries have generous amounts of assorted phytochemicals (flavonoids and others), and/but nothing to set one ahead of the other.
As per any berries that aren’t poisonous, both of these are fine choices for most people most of the time, but redcurrants win with room to spare in most categories.
Want to learn more?
You might like to read:
Health Benefits Of Cranberries (But: You’d Better Watch Out)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
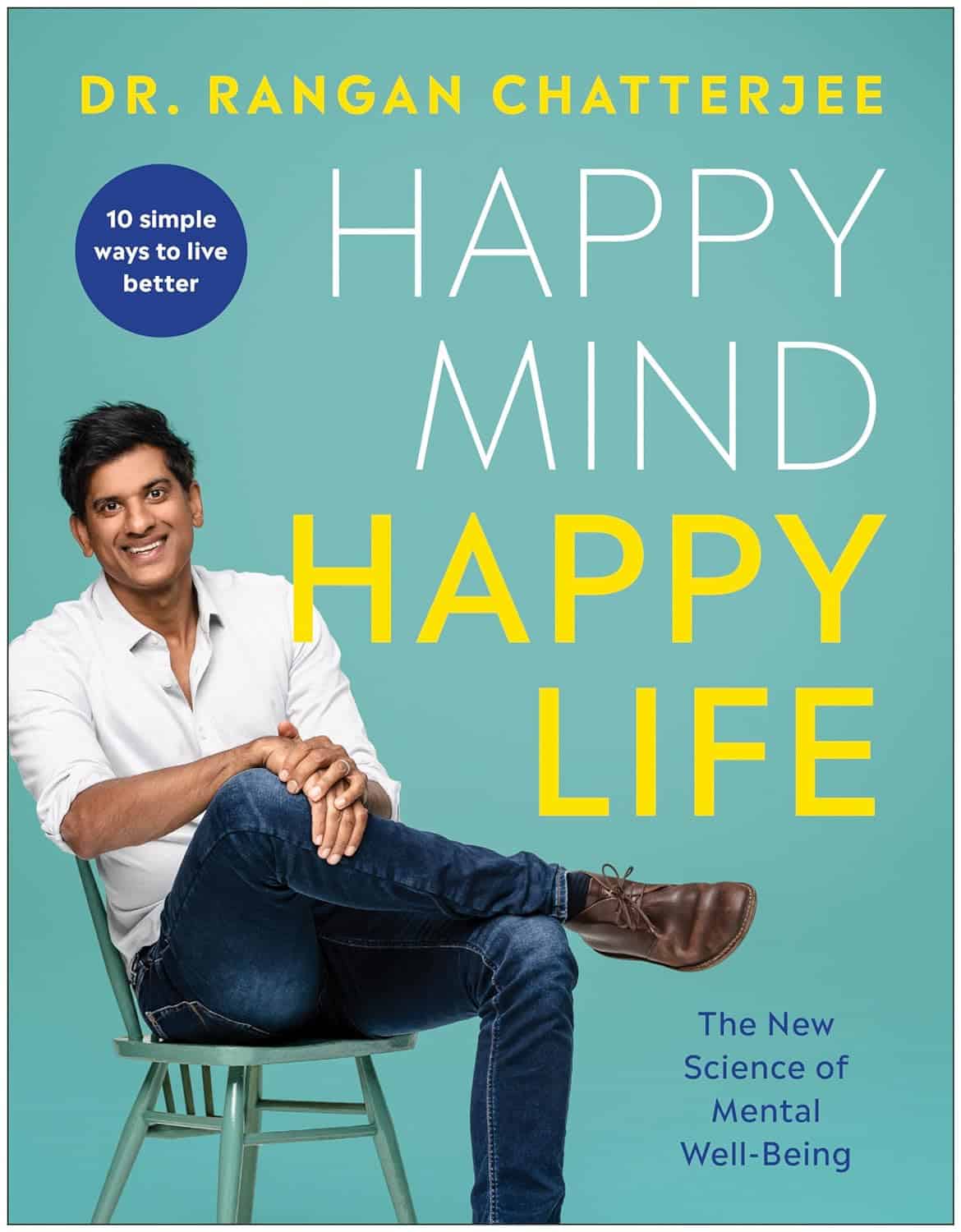
Happy Mind, Happy Life – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s start with a “why”. If happiness doesn’t strike you as a worthwhile goal in and of itself, Dr. Chatterjee discusses the health implications of happiness/unhappiness.
And, yes, including in studies where other factors were controlled for, so he shows how happiness/unhappiness does really have a causal role in health—it’s not just a matter of “breaking news: sick people are less happy”.
The author, a British GP (General Practitioner, the equivalent of what the US calls a “family doctor”) with decades of experience, has found a lot of value in the practice of holistic medicine. For this reason, it’s what he recommends to his patients at work, in his books, his blog, and his regular spot on a popular BBC breakfast show.
The writing style is relaxed and personable, without skimping on information density. Indeed, Dr. Chatterjee offers many pieces of holistic health advice, and dozens of practical exercises to boost your happiness and proof you against adversity.
Because, whatever motivational speakers may say, we can’t purely “think ourselves happy”; sometimes we have real external threats and bad things in life. But, we can still improve our experience of even these things, not to mention suffer less, and get through it in better shape with a smile at the end of it.
Bottom line: if you’d like to be happier and healthier (who wouldn’t?), then this book is a sure-fire way to set you on that path.
Click here to check out Happy Mind, Happy Life and upgrade yours!
Share This Post
-
Nasal Hair; How Far To Go?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
t’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝As a man in his sixties I find I need to trim my nasal hair quite frequently, otherwise it sticks out in an unsightly manner. But I’m never sure how severely I should cut the hairs back, or even how best to do it. Please advise.❞
As you might know, those hairs are really important for our health, so let’s start by mentioning that yes, trimming is the way, not plucking!
In an ideal world, we’d not trim them further back than the entrance to our nostrils, but given the constant nature of hair-growing, that could become a Sisyphean task.
A good compromise, if you’re not up for trimming when you get up and having visible hairs by evening, is to put the scissors away (if you haven’t already) and use a nasal hair trimmer; these are good at a) trimming nasal hairs b) abstaining from trimming them too far back.
By all means shop around, but here’s an example product on Amazon, for your convenience!
- Note 1: despite the product description, please do not stick this in your ear (or any other orifice that’s not your nose, for the love of all that is holey)
- Note 2: we chose that one for a reason; the shape of the head prevents overtrimming.
- In contrast, we do not recommend this cheaper one that has a different shape head for a closer trim, which in this case, is not what we want.
Enjoy!
Share This Post
-
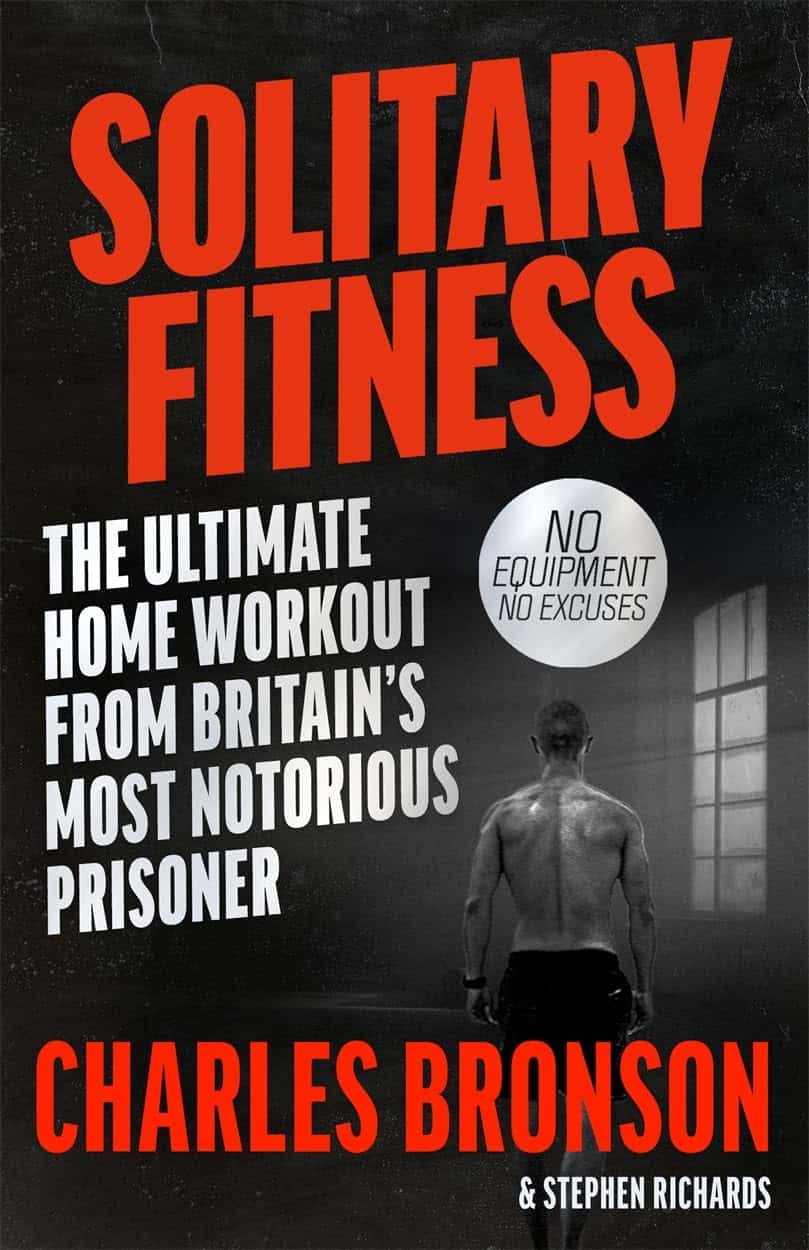
Solitary Fitness – by Charles Bronson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes it can seem that every new diet and/or exercise regime you want to try will change your life, if just you first max out your credit card on restocking your kitchen and refurbishing your home gym, not to mention buying all the best supplements, enjoying the latest medical gadgets, and so on and so forth.
And often… Most of those things genuinely are good! And it’s great that such things are becoming more accessible and available.
But… Wouldn’t it be nice to know how to have excellent strength and fitness without any of that, even if just as a “bare bones” protocol to fall back on? That’s what Manson provides in this book.
The writing style is casual and friendly; Manson is not exactly an academic, but he knows his stuff when it comes to what works. And a good general rule of thumb is: if it’s something that he can do in his jail cell, we can surely do it in the comfort of our homes.
Bottom line: if you want functional strength and fitness with zero gimmicks, this is the book for you (as an aside, it’s also simply an interesting and recommendable read, sociologically speaking, but that’s another matter entirely).
Share This Post
Related Posts
-
How to Prevent Dementia – by Dr. Richard Restak
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written about this topic here, we know. But there’s a lot more we can do to be on guard against, and pre-emptively strengthen ourselves against, dementia.
The author, a neurologist, takes us on a detailed exploration of dementia in general, with a strong focus on Alzheimer’s in particular, as that accounts for more than half of all dementia cases.
But what if you can’t avoid it? It could be that with the wrong genes and some other factor(s) outside of your control, it will get you if something else doesn’t get you first.
Rather than scaremongering, Dr. Restak tackles this head-on too, and discusses how symptoms can be managed, to make the illness less anxiety-inducing, and look to maintain quality of life as much as possible.
The style of the book is… it reads a lot like an essay compilation. Good essays, then organized and arranged in a sensible order for reading, but distinct self-contained pieces. There are ten or eleven chapters (depending on how we count them), each divided into few or many sections. All this makes for:
- A very “read a bit now and a bit later and a bit the next day” book, if you like
- A feeling of a very quick pace, if you prefer to sit down and read it in one go
Either way, it’s a very informative read.
Bottom line: if you’d like to better understand the many-headed beast that is dementia, this book gives a far more comprehensive overview than we could here, and also explains the prophylactic interventions available.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Vaginal Probiotics: What Does The Science Say?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Is there any merit to vaginal probiotics?❞
What a fun question! First let’s break it down, as this could mean two different things:
- Probiotics, which you consume, using your mouth, which are marketed as benefiting vaginal health
- Probiotics taken as a vaginal pessary/suppository, to act directly there
The former has limited evidence for it, but generally speaking, improving one’s gut health improves all other areas of health, so it’s not surprising if it helps this too.
See for example:
Some notes:
- candidal vaginitis means a yeast infection causing vaginal inflammation
- bacterial vaginosis means a vaginal bacterial imbalance (generally also featuring vaginal inflammation, though it can be asymptomatic)
In the latter case, the “imbalance” in question is usually a shortage of Lactobacillus sp. (that is to say, the diverse species of the Lactobacillus genus) resulting in an overgrowth of other kinds of bacteria, which in turn results in changing the vaginal microbiome to make it warmer and more acidic than it should be.
While a healthy vagina shouldn’t smell of roses, it shouldn’t smell fishy either; if it does, that’s a sign of bacterial vaginosis.
What it’s supposed to be like: slightly bitter, slightly salty, distinctly umami, along with a cocktail of personal pheromones (and if menstruating or otherwise* vaginally bleeding, then of course add: iron/”metallic”). The pheromones will also reflect any hormonal changes, but should never make anything smell bad, just different.
*e.g. due to PCOS, fibroids, etc. Note that in the case of PCOS, it may also smell a little different (if it does, then usually: a little more musky), due to often different hormone levels. Again: it still shouldn’t smell bad, though, just different.
In the above-linked study, taking more live Lactobacillus acidophilus (in yogurt, eating it, with their mouths) improved levels of L. acidophilus in the vagina. While the study authors concluded “this ingestion of yogurt may have reduced episodes of bacterial vaginosis”, which is rather a weak claim, it can be argued that it merely improving the levels of L. acidophilus in the vagina was already a win.
That was a small (n=42, and only 7 followed through to completion) and old (1996) study, and it bears mentioning that most of the studies into this seem to be small and old, but conclude similarly with weakly positive statements.
However, it does make a difference what kind of Lactobacillus is used, for example in this next study…
- L. fermentum RC-14 worked well (90% success rate)
- L. rhamnosus GR-1 worked somewhat (40% success rate)
- L. rhamnosus GG did not work (0% success rate)
So, diversity is key, and getting a wide range of Lactobacillus sp. seems to be a safe bet.
Short version: enjoying probiotics as part of your diet probably improves vaginal health, just like it improves pretty much everything else.
See also: Make Friends With Your Gut (You Can Thank Us Later)
You would think that this would mean that taking probiotics as a vaginal pessary/suppository would be even better, but the results are weaker, as in this study, which produced temporary improvements in about half the study group, with only 3 out of 28 being free of bacterial vaginosis the next month:
Treatment of bacterial vaginosis with lactobacilli
This study got better results, with a 61% success rate:
Important note
Do note that this last category, involving topical treatments (i.e., manually introducing Lactobacillus sp. to the vagina) were all in cases of pre-existing bacterial vaginosis, not as a prophylactic and/or general health-improving thing.
If your vagina seems happy right now, then do not mess with its happy bacterial balance!
And at all times (regardless of whether it seems happy right now or not): do not douche (it does not need it and will not benefit from it; the vagina is self-cleaning*) as this will wash out many of your Lactobacilli and will do absolutely nothing against any Candida there (C. albicans being a rooted fungus, whereas Lactobacillus is a sausage-shaped bacterium with many tiny appendages but no actual ability to stay put), so Candida will flourish in the Lactobacillus’s absence.
*by the vagina, we are referring to the vaginal canal. The vulva—the outside part consisting of the two pairs of labia, the glans clitoris, and clitoral hood—are not self-cleaning, and should just be washed gently per your normal bath/shower routine; that’s perfectly fine and good.
And definitely don’t put any “cleansing” toiletries inside the vagina (or any toiletries at all, for that matter), even if they are sold and marketed for that purpose; they will not help and they will harm.
Also, due to their neighborliness, messing up the microbiome inside the vagina is a common way to also get Candida inside the urethra:
How To Avoid Urinary Tract Infections (UTIs)
One other option
Finally, unless you have a “very good friend” you have a pressing urge to swap germs with, you might want to leave this one to the scientists, but we share this paper just for interest:
Lastly…
Going back to oral supplementation, if you’d like to try that then check out this for further notes on what, why, how, etc:
How Much Difference Do Probiotic Supplements Make To Health?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Brown Rice vs Russet Potatoes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing brown rice to russet potatoes, we picked the rice.
Why?
First we’ll note: for brevity and to avoid undue repetitiveness, we’re henceforth going to just say “rice” and “potato”, respectively, but values and conclusions are still for brown rice and russet potatoes. Also, we are including the flesh and skin into the metrics for the potato (without the skin, many nutrients are no longer present).
In terms of macros, the rice has more fiber, carbs, and protein. It’s difficult to compare glycemic indices in this case, because they both need cooking before eating, and how one cooks them (and whether one cools them) along with other preparatory methods will change the GI considerably. Thus, we’ll simply go with the more nutritionally dense option, and that’s the rice.
In the category of vitamins, the rice has much more of vitamins B1, B2, B3, B5, B6, B7, B9, E, and choline, while the potato has more of vitamins C and K. A clear win for rice (and by the way, that’s 60x the vitamin E, but as potatoes don’t have much vitamin E, in practical terms, it’s actually the B-vitamins where rice’s strengths really show, as potatoes aren’t a bad source but rice is amazing).
When it comes to minerals, rice has a lot more copper, iron, magnesium, manganese, phosphorus, selenium, and zinc, while potato has more calcium and potassium. Another easy win for rice.
You may be wondering about phytic acid: brown rice contains this by default, and it is something of an antinutrient (i.e., if left as-is, it reduces the bioavailability of other nutrients), and/but the phytic acid content is reduced to negligible by two things: soaking and heating (especially if those two things are combined) ← doing this the way described results in bioavailability of nutrients that’s even better than if there were just no phytic acid, albeit it requires you having the time to soak, and do so at temperature.
All in all, adding up the sections makes for an overall win for brown rice, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Carb-Strong or Carb-Wrong? Should You Go Light Or Heavy On Carbs?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: