Fall Asleep In 2 Minutes (Doctor Explains)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beyond “sleep hygiene”, Dr. Siobhan Deshauer has insights to share:
Rest for your body and mind
First, do still do the basics. That means dimming/filtering lights for an hour before bed, lowering the room temperature a little, ensuring you have nice fresh sheets, not having alcohol or caffeine before bed, and getting out of bed if you’re not asleep within half an hour, to avoid associating being in bed with wakefulness.
Next, the extra tips:
- Progressive relaxation: tense and relax each muscle group from toes to head
- Box breathing: inhale, hold, exhale, and hold for 4 seconds each; helps calm the nervous system (it’s called “box breathing” because of the 4:4:4:4 setup)
- Diaphragmatic breathing: focus on belly breathing, with longer exhalation to activate the parasympathetic nervous system (note that this can, and even ideally should, be done at the same time as the previous)
- Cognitive shuffling: think of words starting with each letter of a chosen word while visualizing them (this is like “counting sheep”, but does the job better—the job in question being preventing your brain from moving to anything more strenuous or stressful)
For more on all of these plus some extra side-along advice, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Non-Sleep Deep Rest: A Neurobiologist’s Take ← a way to get many of the benefits of sleep, while awake
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
“I Stretched Every Day For 30 Days: Game Changer!”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How much can an unflexible person really improve in just 20 minutes per day for a month? Makari Espe finds out:
Consistency really is key
We’re supposed to stretch at least 3 times per week; for many people, the reality is often more like 2 times per year (often the 1st and 2nd of January).
So, how quickly can such neglect be turned around?
Upon initial testing, she found she was even less flexible than thought, and set about her work:
The stretches she used were from random 20-minute full body stretch videos on YouTube, of which there are many, but she used a different one each day. As she went along, she found some favorite kinds of stretching and some favorite instructors, and settled on mostly Peloton stretching videos—she also switched to evening stretching sessions instead of morning.
Along the way, she already noticed gradual improvement in mobility and reduced body tension, and after 3 weeks, it had become a habit that she started craving.
The final test? There’s a marked improvement; see the video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Yoga Teacher: “If I wanted to get flexible in 2025, here’s what I’d do”
Take care!
Share This Post
-
In Defense of Food – by Michael Pollan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Eat more like the French. Or the Italians. Or the Japanese. Or…
Somehow, whatever we eat is not good enough, and we should always be doing it differently!
Michael Pollan takes a more down-to-Earth approach.
He kicks off by questioning the wisdom of thinking of our food only in terms of nutritional profiles, and overthinking healthy-eating. He concludes, as many do, that a “common-sense, moderate” approach is needed.
And yet, most people who believe they are taking a “common-sense, moderate” approach to health are in fact over-fed yet under-nourished.
So, how to fix this?
He offers us a reframe: to think of food as a relationship, and health being a product of it:
- If we are constantly stressing about a relationship, it’s probably not good.
- On the other hand, if we are completely thoughtless about it, it’s probably not good either.
- But if we can outline some good, basic principles and celebrate it with a whole heart? It’s probably at the very least decent.
The style is very casual and readable throughout. His conclusions, by the way, can be summed up as “Eat real food, make it mostly plants, and make it not too much”.
However, to summarize it thusly undercuts a lot of the actual value of the book, which is the principles for discerning what is “real food” and what is “not too much”.
Bottom line: if you’re tired of complicated eating plans, this book can help produce something very simple, attainable, and really quite good.
Click here to check out In Defense of Food, for some good, hearty eating.
Share This Post
-
The Joy of Saying No – by Natalie Lue
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superficially, this seems an odd topic for an entire book. “Just say no”, after all, surely! But it’s not so simple as that, is it?
Lue looks into what underpins people-pleasing, first. Then, she breaks it down into five distinct styles of people-pleasing that each come from slightly different motivations and ways of perceiving how we interact with those around us.
Lest this seem overly complicated, those five styles are what she calls: gooding, efforting, avoiding, saving, suffering.
She then looks out how to have a healthier relationship with our yes/no decisions; first by observing, then by creating healthy boundaries. “Healthy” is key here; this isn’t about being a jerk to everyone! Quite the contrary, it involves being honest about what we can and cannot reasonably take on.
The last section is about improving and troubleshooting this process, and constitutes a lot of the greatest value of the book, since this is where people tend to err the most.
Bottom line: this book is informative, clear, and helpful. And far from disappointing everyone with “no”, we can learn to really de-stress our relationships with others—and ourselves.
Share This Post
Related Posts
-
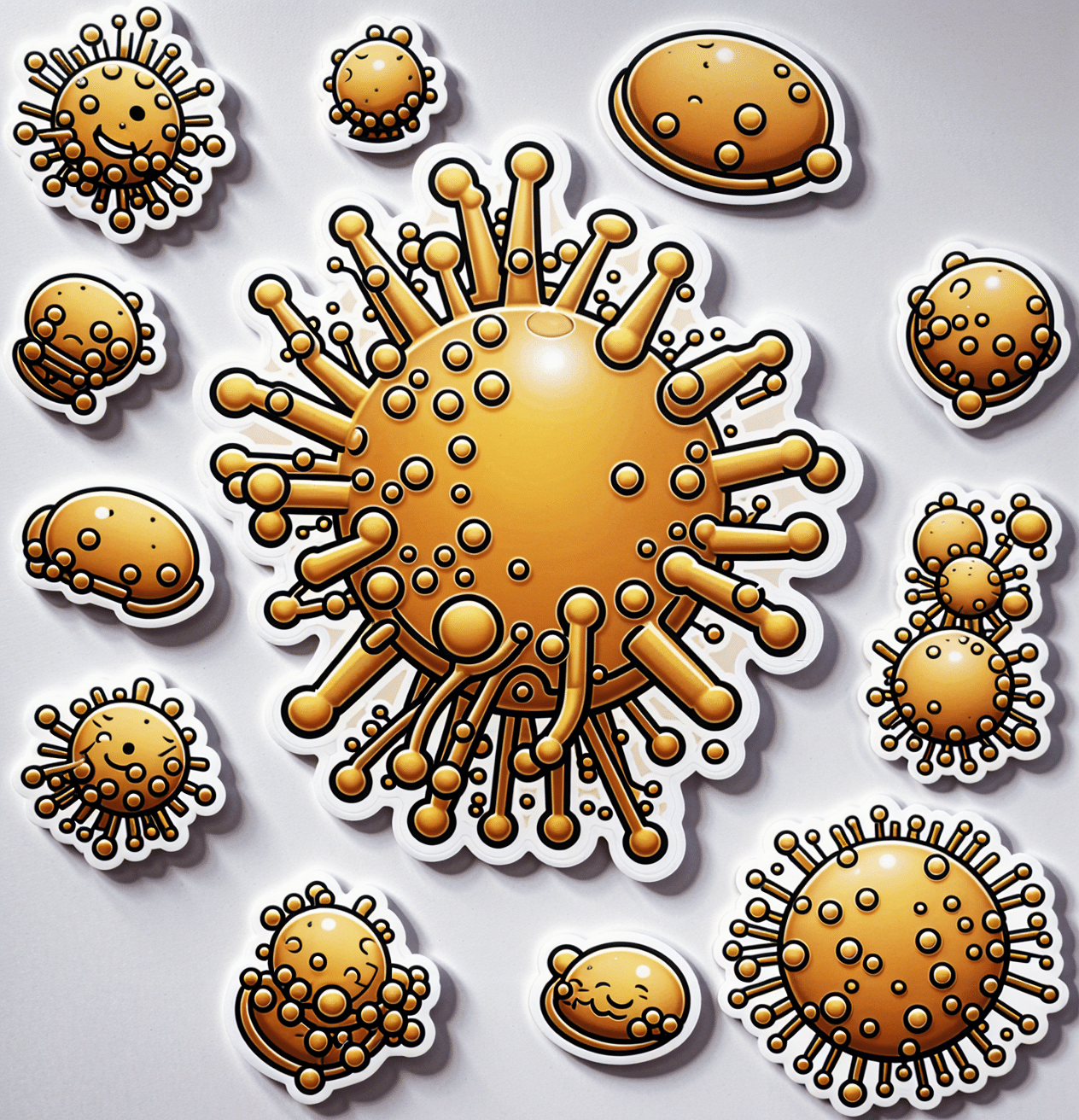
Understanding Cellulitis: Skin And Soft Tissue Infections
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference between a minor passing skin complaint, and a skin condition that’s indicative of something more serious? Dr. Thomas Watchman explains:
More than skin-deep
Cellulitis sounds benign enough, like having a little cellulite perhaps, but in fact it means an infection of the skin and—critically—the underlying soft tissues.
Normally, the skin acts as a barrier against infections, but this barrier can be breached by physical trauma (i.e. an injury that broke the skin), eczema, fungal nail infections, skin ulcers, and other similar things that disrupt the skin’s ability to protect us.
Things to watch out for: Dr. Watchman advises we keep an eye out for warm, reddened skin, swelling, and blisters. Specifically, a golden-yellow crust to these likely indicates a Staphylococcus aureus infection (hence the name).
There’s a scale of degrees of severity:
- Class 1: No systemic toxicity or comorbidities
- Class 2: Systemic toxicity or comorbidities present
- Class 3: Significant systemic toxicity or comorbidities with risk of significant deterioration
- Class 4: Sepsis or life-threatening infection
…with antibiotics being recommended in the latter two cases there, or in other cases for frail, young, old, or immunocompromised patients. Given the rather “scorched earth” results of antibiotics (they cause a lot of collateral iatrogenic damage), this can be taken as a sign of how seriously such infections should be taken.
For more about all this, including visual guides, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Of Brains & Breakouts: The Brain-Skin Doctor
- Beyond Supplements: The Real Immune-Boosters!
- Antibiotics? You Might Want To Think Thrice
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chili Chestnut, Sweet Apricot, & Whipped Feta Toasts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a delightful breakfast or light lunch option, full of gut-healthy ingredients and a fair list of healthy polyphenols too.
You will need
- ½ baguette, sliced into ½” slices; if making your own, feel free to use our Delicious Quinoa Avocado Bread recipe. If buying shop-bought, a sourdough baguette will likely be the healthiest option, and tasty too.
- 4 oz feta cheese; if you are vegan, a plant-based version will work in culinary terms, but will have a different (less gut-healthy) nutritional profile, as plant-based cheeses generally use a lot of coconut oil and potato starch, and are not actually fermented.
- 1 tbsp yogurt; your preference what kind; live-cultured with minimal additives is of course best—and this time, plant-based is also just as good, healthwise, since they are fermented and contain more or less the same beneficial bacteria, and have a good macro profile too.
- 4 oz precooked chestnuts, finely chopped
- 6 dried apricots, finely chopped
- ¼ bulb garlic, grated
- 2 tsp harissa paste
- 1 tsp black pepper, coarse ground
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil, for frying
- Optional garnish: finely chopped chives
Method
(we suggest you read everything at least once before doing anything)
1) Combine the feta and yogurt in a small, high-speed blender and process into a smooth purée. If it isn’t working, add 1 tbsp kettle-hot water and try again.
2) Heat the oil in a skillet over a medium heat; add the garlic and when it starts to turn golden, add the chestnuts and harissa, as well as the black pepper and MSG/salt. Stir for about 2 minutes, and then stir in the apricots and take it off the heat.
3) Toast the baguette slices under the grill. If you’re feeling bold about the multitasking, you can start this while still doing the previous step, for optimal timing. If not, simply doing it in the order presented is fine.
4) Assemble: spread the whipped feta over the toast; add the apricot-chestnut mixture, followed by the finely chopped chives if using, and serve immediately:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Apricots vs Peaches – Which is Healthier?
- Why You Should Diversify Your Nuts!
- Capsaicin For Weight Loss And Against Inflammation
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Sea Salt vs MSG – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Best Foods For Collagen Production
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Andrea Suarez gives us the low-down on collagen synthesis and maintenance. Collagen is the most abundant protein in our body, and it can be fairly described as “the stuff that holds us together”. It’s particularly important for joints and bones too, though many people’s focus on it is for the skin. Whatever your priorities, collagen levels are something it pays to be mindful of, as they usually drop quite sharply after a certain age. What certain age? Well, that depends a lot on you, and your diet and lifestyle. But it can start to decline from the age of 30 with often noticeable drop-offs in one’s mid-40s and again in one’s mid-60s.
Showing us what we’re made of
There’s a lot more to having good collagen levels than just how much collagen we consume (which for vegetarians/vegans, will be “none”, unless using the “except if for medical reasons” exemption, which is probably a little tenuous in the case of collagen but nevertheless it’s a possibility; this exemption is usually one that people use for, say, a nasal spray vaccine that contains gelatine, or a medicinal tablet that contains lactose, etc).
Rather, having good collagen levels is also a matter of what we eat that allows us to synthesize our own collagen (which includes: its ingredients, and various “helper” nutrients), as well as what dietary adjustments we make to avoid our extant collagen getting broken down, degraded, and generally lost.
Here’s what Dr. Suarez recommends:
Protein-rich foods (but watch out)
- Protein is essential for collagen production.
- Sources: fish, soy, lean meats (but not red meats, which—counterintuitively—degrade collagen), eggs, lentils.
- Egg whites are high in lysine, vital for collagen synthesis.
- Bone broth is a natural source of collagen.
Omega-3 fatty acids
- Omega-3s are anti-inflammatory and protect skin collagen.
- Sources: walnuts, chia seeds, flax seeds, fatty fish (e.g. mackerel, sardines).
Leafy greens
- Leafy dark green vegetables (e.g. kale, spinach) are rich in vitamins C and B9.
- Vitamin C is crucial for collagen synthesis and acts as an antioxidant.
- Vitamin B9 supports skin cell division and DNA repair.
Red fruits & vegetables
- Red fruits/vegetables (e.g. tomatoes, red bell peppers) contain lycopene, an antioxidant that protects collagen from UV damage (so, that aspect is mostly relevant for skin, but antioxidants are good things to have in all of the body in any case).
Orange-colored vegetables
- Carrots and sweet potatoes are rich in vitamin A, which helps in collagen repair and synthesis.
- Vitamin A is best from food, not supplements, to avoid potential toxicity.
Fruits rich in vitamin C
- Citrus fruits, kiwi, and berries are loaded with vitamin C and antioxidants, essential for collagen synthesis and skin health.
Soy
- Soy products (e.g. tofu, soybeans) contain isoflavones, which reduce inflammation and inhibit enzymes that degrade collagen.
- Soy is associated with lower risks of chronic diseases.
Garlic
- Garlic contains sulfur, taurine, and lipoic acid, important for collagen production and repair.
What to avoid:
- Reduce foods high in advanced glycation end products (AGEs), which damage collagen and promote inflammation.
- AGEs are found in fried, roasted, or grilled fatty proteinous foods (e.g. meat, including synthetic meat, and yes, including grass-fed nicely marketed meat—although processed meat such as bacon and sausages are even worse than steaks etc).
- Switch to cooking methods like boiling or steaming to reduce AGE levels.
- Processed foods, sugary pastries, and red meats contribute to collagen degradation.
General diet tips:
- Incorporate more plant-based, antioxidant-rich foods.
- Opt for slow cooking to reduce AGEs.
- Since sustainability is key, choose foods you enjoy for a collagen-boosting diet that you won’t seem like a chore a month later.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
We Are Such Stuff As Fish Are Made Of ← our main feature research review about collagen
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: