Good to Go – by Christie Aschwanden
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many of us may more often need to recover from a day of moving furniture than running a marathon, but the science of recovery can still teach us a lot. The author, herself an endurance athlete and much-decorated science journalist, sets out to do just that.
She explores a lot of recovery methods, and examines whether the science actually backs them up, and if so, to what degree. She also, in true science journalism style, talks to a lot of professionals ranging from fellow athletes to fellow scientists, to get their input too—she is nothing if not thorough, and this is certainly not a book of one person’s opinion with something to sell.
Indeed, on the contrary, her findings show that some of the best recovery methods are the cheapest, or even free. She also looks at the psychological aspect though, and why many people are likely to continue with things that objectively do not work better than placebo.
The style is very easy-reading jargon-free pop-science, while nevertheless being backed up with hundreds of studies cited in the bibliography—a perfect balance of readability and reliability.
Bottom line: for those who wish to be better informed about how to recover quickly and easily, this book is a treasure trove of information well-presented.
Click here to check out Good To Go, and always be good to go!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Synergistic Brain-Training
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let The Games Begin (But It Matters What Kind)
Exercise is good for brain health; we’ve written about this before, for example:
How To Reduce Your Alzheimer’s Risk ← there are many advices here, but exercise, especially cardiovascular exercise in this case, is an important item on the list!
Today it’s Psychology Sunday though, and we’re going to talk about looking after brain health by means of brain-training, via games.
“Brain-training” gets a lot of hype and flak:
- Hype: do sudoku every day and soon you will have an IQ of 200 and still have a sharp wit at the age of 120
- Flak: brain-training is usually training only one kind of cognitive function, with limited transferability to the rest of life
The reality is somewhere between the two. Brain training really does improve not just outwardly measurable cognitive function, but also internally measurable improvements visible on brain scans, for example:
- Cognitive training modified age-related brain changes in older adults with subjective memory decline
- Functional brain changes associated with cognitive training in healthy older adults: A preliminary ALE meta-analysis
But what about the transferability?
Let us play
This is where game-based brain-training comes in. And, the more complex the game, the better the benefits, because there is more chance of applicability to life, e.g:
- Sudoku: very limited applicability
- Crosswords: language faculties
- Chess: spatial reasoning, critical path analysis, planning, memory, focus (also unlike the previous two, chess tends to be social for most people, and also involve a lot of reading, if one is keen)
- Computer games: wildly varied depending on the game. While an arcade-style “shoot-em-up” may do little for the brain, there is a lot of potential for a lot of much more relevant brain-training in other kinds of games: it could be planning, problem-solving, social dynamics, economics, things that mirror the day-to-day challenges of running a household, even, or a business.
- It’s not that the skills are useful, by the way. Playing “Stardew Valley” will not qualify you to run a real farm, nor will playing “Civilization” qualify you to run a country. But the brain functions used and trained? Those are important.
It becomes easily explicable, then, why these two research reviews with very similar titles got very different results:
- A Game a Day Keeps Cognitive Decline Away? A Systematic Review and Meta-Analysis of Commercially-Available Brain Training Programs in Healthy and Cognitively Impaired Older Adults
- Game-based brain training for improving cognitive function in community-dwelling older adults: A systematic review and meta-regression
The first review found that game-based brain-training had negligible actual use. The “games” they looked at? BrainGymmer, BrainHQ, CogMed, CogniFit, Dakim, Lumosity, and MyBrainTrainer. In other words, made-for-purpose brain-trainers, not actual computer games per se.
The second reviewfound that game-based training was very beneficial. The games they looked at? They didn’t name them, but based on the descriptions, they were actual multiplayer online turn-based computer games, not made-for-purpose brain-trainers.
To summarize the above in few words: multiplayer online turn-based computer games outperform made-for-purpose brain-trainers for cognitive improvement.
Bringing synergy
However, before you order that expensive gaming-chair for marathon gaming sessions (research suggests a tail-off in usefulness after about an hour of continuous gaming per session, by the way), be aware that cognitive training and (physical) exercise training combined, performed close in time to each other or simultaneously, perform better than the sum of either alone:
See also:
❝Simultaneous training was the most efficacious approach for cognition, followed by sequential combinations and cognitive training alone, and significantly better than physical exercise.
Our findings suggest that simultaneously and sequentially combined interventions are efficacious for promoting cognitive alongside physical health in older adults, and therefore should be preferred over implementation of single-domain training❞
~ Dr. Hanna Malmberg Gavelin et al.
Take care!
Share This Post

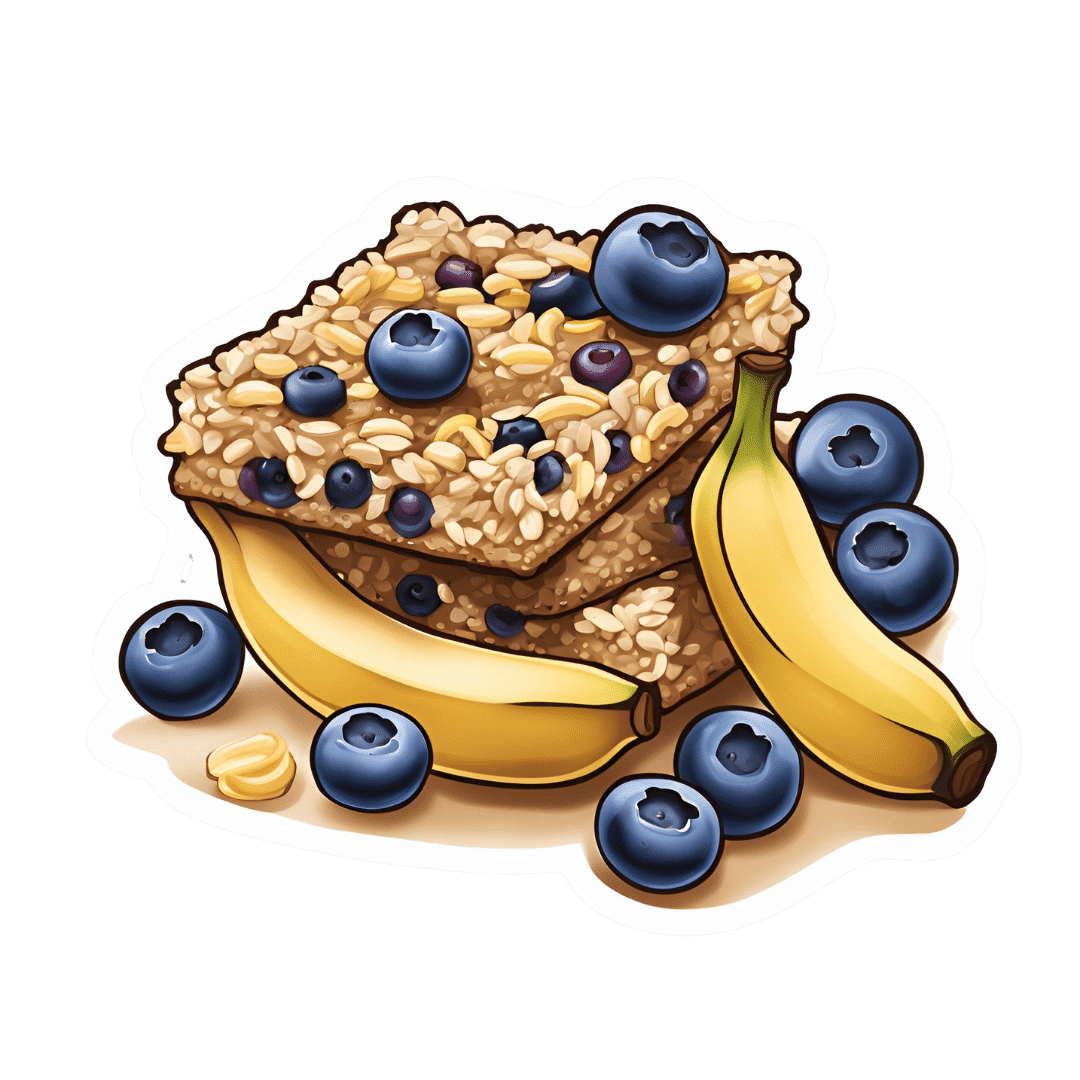
Blueberry & Banana Collagen Baked Oats
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Good news for vegans/vegetarians! While we include an optional tablespoon of collagen powder in this recipe, the whole recipe is already geared around collagen synthesis, so it’s very collagen-boosting even with just the plants, providing collagen’s building blocks of protein, zinc, and vitamins C and D (your miraculous body will use these to assemble the collagen inside you).
You will need
- 2 cups oats, whence the protein and zinc
- 1 cup milk (your preference what kind; we recommend almond for flavor; whether you choose plant or animal though, it should be fortified with vitamin D)
- 2 bananas, peeled and mashed
- 4 oz blueberries, whence the vitamin C (frozen is fine) (chopped dried apricots are also a fine substitute if that’s more convenient)
- 1 oz flaked almonds, whence the protein and zinc
- 1 tbsp pumpkin seeds, whence the protein and zinc
- 1 tbsp flax seeds, whence the protein and zinc
- Optional: 1 tbsp maple syrup
- Optional: 1 tbsp collagen powder, dissolved in 1 oz hot water
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃.
2) Mix the oats with 2 cups boiling water; allow to stand for 10–15 minutes, and then drain any excess water.
3) Mix the mashed bananas with the remaining ingredients except the milk and blueberries, stirring thoroughly.
4) Add the softened oats, and stir those in thoroughly too.
5) Add the milk and blueberries, in that order, stirring gently if using fresh blueberries, lest they get crushed.
6) Pour the mixture into an 8″ square cake tin that you have lined with baking paper, and smooth the top.
7) Bake for about 40 minutes or until firm and golden brown. Allow to cool; it will firm up more while it does.
8) Cut into squares or bars, and serve or store for later.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
We Are Such Stuff As Fish Are Made Of ← our main feature about collagen
Take care!
Share This Post

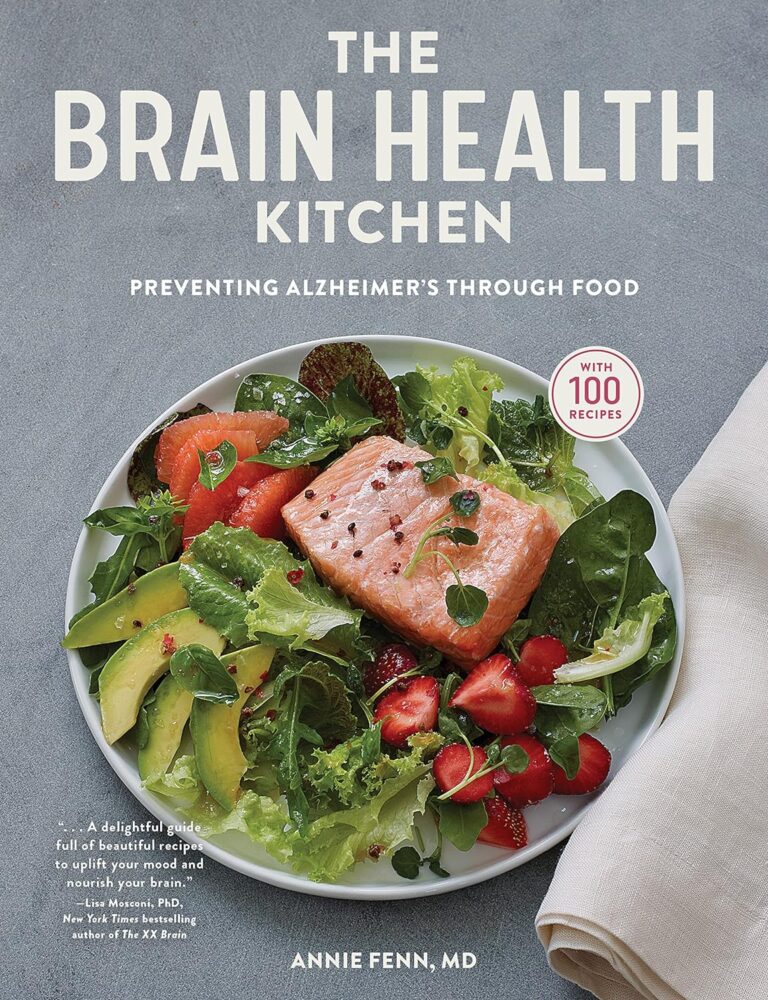
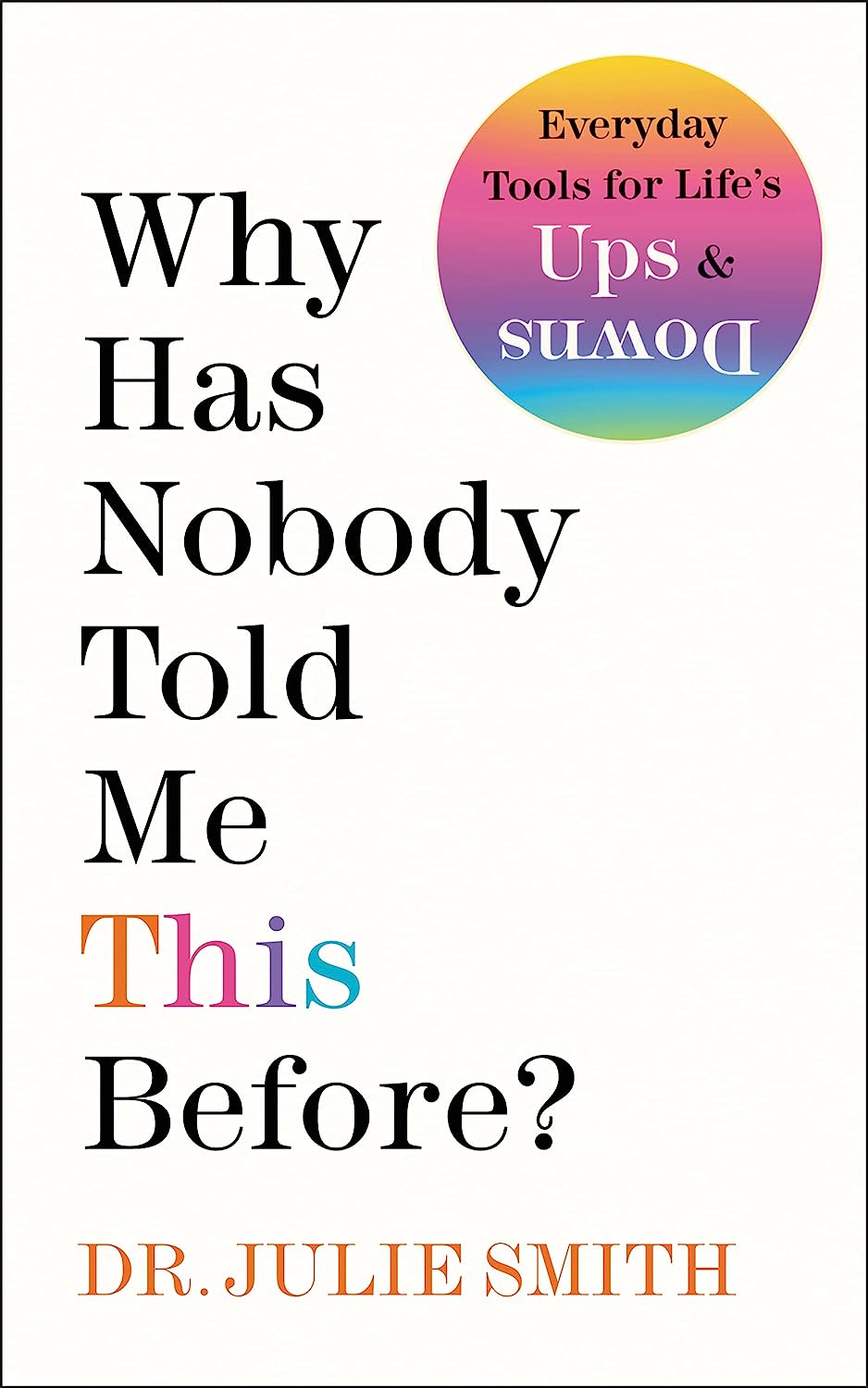
Why Has Nobody Told Me This Before? – by Dr. Julie Smith
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superficially, this can be called a “self-help” book, but that undersells it rather. It’s a professionally-written (as in, by a professional psychologist) handbook full of resources. Its goal? Optimizing your mental health to help you stay resilient no matter what life throws your way.
While the marketing of this book is heavily centered around Dr. Smith’s Internet Celebrity™ status, a lot of her motivation for writing it seems to be precisely so that she can delve deeper into the ideas that her social media “bites” don’t allow room for.
Many authors of this genre pad their chapters with examples; there are no lengthy story-telling asides here, and her style doesn’t need them. She knows her field well, and knows well how to communicate the ideas that may benefit the reader.
The main “meat” of the book? Tips, tricks, guides, resources, systems, flowcharts, mental frameworks, and “if all else fails, do this” guidance. The style of the book is clear and simple, with very readable content that she keeps free from jargon without “dumbing down” or patronizing the reader.
All in all, a fine set of tools for anyone’s “getting through life” toolbox.
Get Your Personal Copy Of “Why Has Nobody Told Me This Before?” on Amazon Now!
Share This Post
Related Posts

How to Think More Effectively – by Alain de Botton
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our brain is our most powerful organ, and our mind is an astonishing thing. So why do we sometimes go off-piste?
The School of Life‘s Alain de Botton lays out for us a framework of cumulative thinking, directions for effort, and unlikely tools for cognitive improvement.
The book especially highlights the importance of such things as…
- making time for cumulative thinking
- not, however, trying to force it
- working with, rather than in spite of, distractions
- noting and making use of our irrationalities
- taking what we think/do both seriously and lightly, at once
- practising constructive self-doubt
The style is as clear and easy as you may have come to expect from Alain de Botton / The School of Life, and yet, its ideas are still likely to challenge every reader in some (good!) way.
Bottom line: if you would like what you think, say, do to be more meaningful, this book will help you to make the most of your abilities!
Click here to check out How To Think More Effectively, and upgrade your thought processes!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

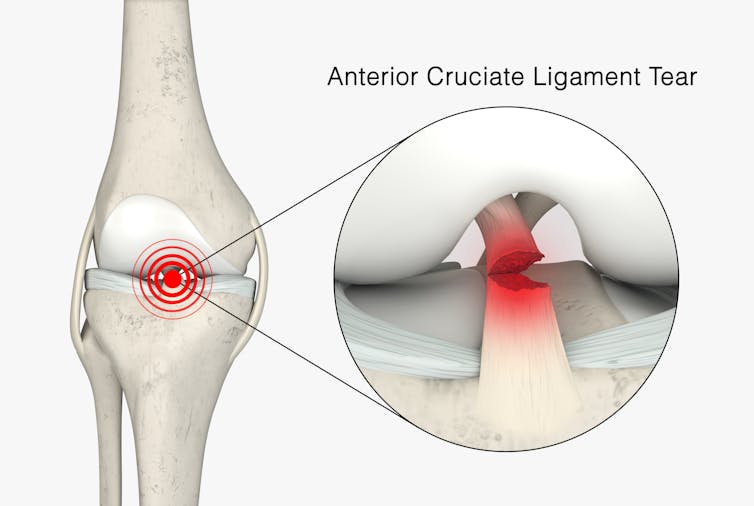
Surgery is the default treatment for ACL injuries in Australia. But it’s not the only way
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The anterior cruciate ligament (ACL) is an important ligament in the knee. It runs from the thigh bone (femur) to the shin bone (tibia) and helps stabilise the knee joint.
Injuries to the ACL, often called a “tear” or a “rupture”, are common in sport. While a ruptured ACL has just sidelined another Matildas star, people who play sport recreationally are also at risk of this injury.
For decades, surgical repair of an ACL injury, called a reconstruction, has been the primary treatment in Australia. In fact, Australia has among the highest rates of ACL surgery in the world. Reports indicate 90% of people who rupture their ACL go under the knife.
Although surgery is common – around one million are performed worldwide each year – and seems to be the default treatment for ACL injuries in Australia, it may not be required for everyone.

PeopleImages.com – Yuri A/Shutterstock What does the research say?
We know ACL ruptures can be treated using reconstructive surgery, but research continues to suggest they can also be treated with rehabilitation alone for many people.
Almost 15 years ago a randomised clinical trial published in the New England Journal of Medicine compared early surgery to rehabilitation with the option of delayed surgery in young active adults with an ACL injury. Over half of people in the rehabilitation group did not end up having surgery. After five years, knee function did not differ between treatment groups.
The findings of this initial trial have been supported by more research since. A review of three trials published in 2022 found delaying surgery and trialling rehabilitation leads to similar outcomes to early surgery.
A 2023 study followed up patients who received rehabilitation without surgery. It showed one in three had evidence of ACL healing on an MRI after two years. There was also evidence of improved knee-related quality of life in those with signs of ACL healing compared to those whose ACL did not show signs of healing.

Experts used to think an ACL tear couldn’t heal without surgery – now there’s evidence it can. SKYKIDKID/Shutterstock Regardless of treatment choice the rehabilitation process following ACL rupture is lengthy. It usually involves a minimum of nine months of progressive rehabilitation performed a few days per week. The length of time for rehabilitation may be slightly shorter in those not undergoing surgery, but more research is needed in this area.
Rehabilitation starts with a physiotherapist overseeing simple exercises right through to resistance exercises and dynamic movements such as jumping, hopping and agility drills.
A person can start rehabilitation with the option of having surgery later if the knee remains unstable. A common sign of instability is the knee giving way when changing direction while running or playing sports.
To rehab and wait, or to go straight under the knife?
There are a number of reasons patients and clinicians may opt for early surgical reconstruction.
For elite athletes, a key consideration is returning to sport as soon as possible. As surgery is a well established method, athletes (such as Matilda Sam Kerr) often opt for early surgical reconstruction as this gives them a more predictable timeline for recovery.
At the same time, there are risks to consider when rushing back to sport after ACL reconstruction. Re-injury of the ACL is very common. For every month return to sport is delayed until nine months after ACL reconstruction, the rate of knee re-injury is reduced by 51%.

For people who opt to try rehabilitation, the option of having surgery later is still there. PeopleImages.com – Yuri A/Shutterstock Historically, another reason for having early surgical reconstruction was to reduce the risk of future knee osteoarthritis, which increases following an ACL injury. But a review showed ACL reconstruction doesn’t reduce the risk of knee osteoarthritis in the long term compared with non-surgical treatment.
That said, there’s a need for more high-quality, long-term studies to give us a better understanding of how knee osteoarthritis risk is influenced by different treatments.
Rehab may not be the only non-surgical option
Last year, a study looking at 80 people fitted with a specialised knee brace for 12 weeks found 90% had evidence of ACL healing on their follow-up MRI.
People with more ACL healing on the three-month MRI reported better outcomes at 12 months, including higher rates of returning to their pre-injury level of sport and better knee function. Although promising, we now need comparative research to evaluate whether this method can achieve similar results to surgery.
What to do if you rupture your ACL
First, it’s important to seek a comprehensive medical assessment from either a sports physiotherapist, sports physician or orthopaedic surgeon. ACL injuries can also have associated injuries to surrounding ligaments and cartilage which may influence treatment decisions.
In terms of treatment, discuss with your clinician the pros and cons of management options and whether surgery is necessary. Often, patients don’t know not having surgery is an option.
Surgery appears to be necessary for some people to achieve a stable knee. But it may not be necessary in every case, so many patients may wish to try rehabilitation in the first instance where appropriate.
As always, prevention is key. Research has shown more than half of ACL injuries can be prevented by incorporating prevention strategies. This involves performing specific exercises to strengthen muscles in the legs, and improve movement control and landing technique.
Anthony Nasser, Senior Lecturer in Physiotherapy, University of Technology Sydney; Joshua Pate, Senior Lecturer in Physiotherapy, University of Technology Sydney, and Peter Stubbs, Senior Lecturer in Physiotherapy, University of Technology Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Tiramisu Crunch Bites
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s coffee, it’s creamy, it’s nutty, it’s chocolatey, what’s not to love? It has all the well-loved flavors of tiramisu, but this recipe is a simple one, and it’s essentially stuffed dates in a way you’ve never had them before. They’re delectable, decadent, and decidedly good for your health. These things are little nutrient-bombs that’ll keep you reaching for more.
You will need
- Coffee (we will discuss this)
- 150g (5.5oz) mascarpone (if vegan or lactose-intolerant, can be substituted with vegan varieties, or at a pinch, pressed silken tofu)
- 500g (1lb) dates (Medjool are ideal)
- Twice as many almonds as you have dates
- 50g (2oz) dark chocolate (the darkest, bitterest, you can find)
- Edible flower petals if you can source them (some shops sell dried rose petals for this purpose)
Method
(we suggest you read everything at least once before doing anything)
1) Take the mascarpone and whisk (or blend) it with the coffee. What kind of coffee, you ask? Many will use instant coffee (1tbsp granules mixed with enough boiling water to dissolve it), and that is actually healthiest (counterintuitive but true) but if you care for flavor over health, and have the means to make espresso, make it ristretto (so, stop it halfway through filling up an espresso cup), let it cool, and use that. Absolute bonus for flavor (not for health): if you have the means to make Turkish coffee, use an equivalent amount of that (again, cooled).
You will now have coffee-flavoured mascarpone. It’s great for your gut and full of antioxidant polyphenols. Set it aside for the moment.
2) Take the dark chocolate and melt it. Please don’t microwave it or try to do it in a pan directly over the hob; instead, you will need to use a Bain-Marie. If you don’t have one made-for-purpose, you can place a metal or heatproof glass bowl in a saucepan, with something to stop it from touching the floor of the pan. Then boil water in the pan (without letting the water get into the bowl), and melt the chocolate in the bowl—this will allow you to melt it evenly without burning the chocolate.
You will now have melted dark chocolate. It has its own set of polyphenols, and is great for everything from the brain to the gut microbiome.
3) Cut the dates lengthways on one side and remove the stone. Stuff them carefully with the coffee-flavored mascarpone (you can use a teaspoon, or use a piping kit if you have one). Add a couple of almonds to each one. Place them all on a big plate, and drizzle the melted chocolate over them. Add the petals if you have them.
The dates and almonds deliver extra vitamins and minerals in abundance (not to mention, lots of fiber), and also are an amazing combination even just by themselves. With the mascarpone and chocolate added, this winning on new levels. We’re not done yet, though…
4) Chill them in the fridge for about 30 minutes.
Serve!

Learn more
For those interested in some of the science of what we have going on today:
- Make The Heart-Healthiest Coffee ← this is about cafestol content and why instant is heart-healthiest (alas)
- The Bitter Truth About Coffee (Or Is It) ← this is about the health benefits (and some risks, but mostly benefits) of coffee
- Why You Should Diversify Your Nuts ← almonds are a top-tier choice, but other nuts are good too! This recipe could work well with hazelnuts, for example (we wouldn’t call it “tiramisu crunch bites” in that case, though, since the flavor profile would change)
- Which Sugars Are Healthier, And Which Are Just The Same? ← for any worrying “aren’t dates sugary, though?”
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: