What happens in my brain when I get a migraine? And what medications can I use to treat it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Migraine is many things, but one thing it’s not is “just a headache”.
“Migraine” comes from the Greek word “hemicrania”, referring to the common experience of migraine being predominantly one-sided.
Some people experience an “aura” preceding the headache phase – usually a visual or sensory experience that evolves over five to 60 minutes. Auras can also involve other domains such as language, smell and limb function.
Migraine is a disease with a huge personal and societal impact. Most people cannot function at their usual level during a migraine, and anticipation of the next attack can affect productivity, relationships and a person’s mental health.

What’s happening in my brain?
The biological basis of migraine is complex, and varies according to the phase of the migraine. Put simply:
The earliest phase is called the prodrome. This is associated with activation of a part of the brain called the hypothalamus which is thought to contribute to many symptoms such as nausea, changes in appetite and blurred vision.
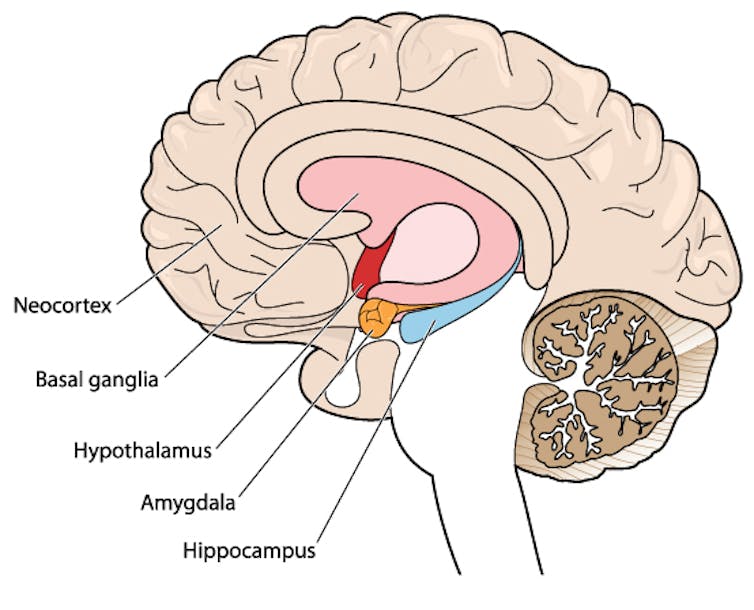
Next is the aura phase, when a wave of neurochemical changes occur across the surface of the brain (the cortex) at a rate of 3–4 millimetres per minute. This explains how usually a person’s aura progresses over time. People often experience sensory disturbances such as flashes of light or tingling in their face or hands.
In the headache phase, the trigeminal nerve system is activated. This gives sensation to one side of the face, head and upper neck, leading to release of proteins such as CGRP (calcitonin gene-related peptide). This causes inflammation and dilation of blood vessels, which is the basis for the severe throbbing pain associated with the headache.
Finally, the postdromal phase occurs after the headache resolves and commonly involves changes in mood and energy.
What can you do about the acute attack?
A useful way to conceive of migraine treatment is to compare putting out campfires with bushfires. Medications are much more successful when applied at the earliest opportunity (the campfire). When the attack is fully evolved (into a bushfire), medications have a much more modest effect.
Aspirin
For people with mild migraine, non-specific anti-inflammatory medications such as high-dose aspirin, or standard dose non-steroidal medications (NSAIDS) can be very helpful. Their effectiveness is often enhanced with the use of an anti-nausea medication.
Triptans
For moderate to severe attacks, the mainstay of treatment is a class of medications called “triptans”. These act by reducing blood vessel dilation and reducing the release of inflammatory chemicals.
Triptans vary by their route of administration (tablets, wafers, injections, nasal sprays) and by their time to onset and duration of action.
The choice of a triptan depends on many factors including whether nausea and vomiting is prominent (consider a dissolving wafer or an injection) or patient tolerability (consider choosing one with a slower onset and offset of action).
As triptans constrict blood vessels, they should be used with caution (or not used) in patients with known heart disease or previous stroke.

Gepants
Some medications that block or modulate the release of CGRP, which are used for migraine prevention (which we’ll discuss in more detail below), also have evidence of benefit in treating the acute attack. This class of medication is known as the “gepants”.
Gepants come in the form of injectable proteins (monoclonal antibodies, used for migraine prevention) or as oral medication (for example, rimegepant) for the acute attack when a person has not responded adequately to previous trials of several triptans or is intolerant of them.
They do not cause blood vessel constriction and can be used in patients with heart disease or previous stroke.
Ditans
Another class of medication, the “ditans” (for example, lasmiditan) have been approved overseas for the acute treatment of migraine. Ditans work through changing a form of serotonin receptor involved in the brain chemical changes associated with the acute attack.
However, neither the gepants nor the ditans are available through the Pharmaceutical Benefits Scheme (PBS) for the acute attack, so users must pay out-of-pocket, at a cost of approximately A$300 for eight wafers.
What about preventing migraines?
The first step is to see if lifestyle changes can reduce migraine frequency. This can include improving sleep habits, routine meal schedules, regular exercise, limiting caffeine intake and avoiding triggers such as stress or alcohol.
Despite these efforts, many people continue to have frequent migraines that can’t be managed by acute therapies alone. The choice of when to start preventive treatment varies for each person and how inclined they are to taking regular medication. Those who suffer disabling symptoms or experience more than a few migraines a month benefit the most from starting preventives.

Almost all migraine preventives have existing roles in treating other medical conditions, and the physician would commonly recommend drugs that can also help manage any pre-existing conditions. First-line preventives include:
- tablets that lower blood pressure (candesartan, metoprolol, propranolol)
- antidepressants (amitriptyline, venlafaxine)
- anticonvulsants (sodium valproate, topiramate).
Some people have none of these other conditions and can safely start medications for migraine prophylaxis alone.
For all migraine preventives, a key principle is starting at a low dose and increasing gradually. This approach makes them more tolerable and it’s often several weeks or months until an effective dose (usually 2- to 3-times the starting dose) is reached.
It is rare for noticeable benefits to be seen immediately, but with time these drugs typically reduce migraine frequency by 50% or more.
‘Nothing works for me!’
In people who didn’t see any effect of (or couldn’t tolerate) first-line preventives, new medications have been available on the PBS since 2020. These medications block the action of CGRP.
The most common PBS-listed anti-CGRP medications are injectable proteins called monoclonal antibodies (for example, galcanezumab and fremanezumab), and are self-administered by monthly injections.
These drugs have quickly become a game-changer for those with intractable migraines. The convenience of these injectables contrast with botulinum toxin injections (also effective and PBS-listed for chronic migraine) which must be administered by a trained specialist.
Up to half of adolescents and one-third of young adults are needle-phobic. If this includes you, tablet-form CGRP antagonists for migraine prevention are hopefully not far away.
Data over the past five years suggest anti-CGRP medications are safe, effective and at least as well tolerated as traditional preventives.
Nonetheless, these are used only after a number of cheaper and more readily available first-line treatments (all which have decades of safety data) have failed, and this also a criterion for their use under the PBS.
Mark Slee, Associate Professor, Clinical Academic Neurologist, Flinders University and Anthony Khoo, Lecturer, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
3 signs your diet is causing too much muscle loss – and what to do about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When trying to lose weight, it’s natural to want to see quick results. So when the number on the scales drops rapidly, it seems like we’re on the right track.
But as with many things related to weight loss, there’s a flip side: rapid weight loss can result in a significant loss of muscle mass, as well as fat.
So how you can tell if you’re losing too much muscle and what can you do to prevent it?
EvMedvedeva/Shutterstock Why does muscle mass matter?
Muscle is an important factor in determining our metabolic rate: how much energy we burn at rest. This is determined by how much muscle and fat we have. Muscle is more metabolically active than fat, meaning it burns more calories.
When we diet to lose weight, we create a calorie deficit, where our bodies don’t get enough energy from the food we eat to meet our energy needs. Our bodies start breaking down our fat and muscle tissue for fuel.
A decrease in calorie-burning muscle mass slows our metabolism. This quickly slows the rate at which we lose weight and impacts our ability to maintain our weight long term.
How to tell you’re losing too much muscle
Unfortunately, measuring changes in muscle mass is not easy.
The most accurate tool is an enhanced form of X-ray called a dual-energy X-ray absorptiometry (DXA) scan. The scan is primarily used in medicine and research to capture data on weight, body fat, muscle mass and bone density.
But while DEXA is becoming more readily available at weight-loss clinics and gyms, it’s not cheap.
There are also many “smart” scales available for at home use that promise to provide an accurate reading of muscle mass percentage.
Some scales promise to tell us our muscle mass. Lee Charlie/Shutterstock However, the accuracy of these scales is questionable. Researchers found the scales tested massively over- or under-estimated fat and muscle mass.
Fortunately, there are three free but scientifically backed signs you may be losing too much muscle mass when you’re dieting.
1. You’re losing much more weight than expected each week
Losing a lot of weight rapidly is one of the early signs that your diet is too extreme and you’re losing too much muscle.
Rapid weight loss (of more than 1 kilogram per week) results in greater muscle mass loss than slow weight loss.
Slow weight loss better preserves muscle mass and often has the added benefit of greater fat mass loss.
One study compared people in the obese weight category who followed either a very low-calorie diet (500 calories per day) for five weeks or a low-calorie diet (1,250 calories per day) for 12 weeks. While both groups lost similar amounts of weight, participants following the very low-calorie diet (500 calories per day) for five weeks lost significantly more muscle mass.
2. You’re feeling tired and things feel more difficult
It sounds obvious, but feeling tired, sluggish and finding it hard to complete physical activities, such as working out or doing jobs around the house, is another strong signal you’re losing muscle.
Research shows a decrease in muscle mass may negatively impact your body’s physical performance.
3. You’re feeling moody
Mood swings and feeling anxious, stressed or depressed may also be signs you’re losing muscle mass.
Research on muscle loss due to ageing suggests low levels of muscle mass can negatively impact mental health and mood. This seems to stem from the relationship between low muscle mass and proteins called neurotrophins, which help regulate mood and feelings of wellbeing.
So how you can do to maintain muscle during weight loss?
Fortunately, there are also three actions you can take to maintain muscle mass when you’re following a calorie-restricted diet to lose weight.
1. Incorporate strength training into your exercise plan
While a broad exercise program is important to support overall weight loss, strength-building exercises are a surefire way to help prevent the loss of muscle mass. A meta-analysis of studies of older people with obesity found resistance training was able to prevent almost 100% of muscle loss from calorie restriction.
Relying on diet alone to lose weight will reduce muscle along with body fat, slowing your metabolism. So it’s essential to make sure you’ve incorporated sufficient and appropriate exercise into your weight-loss plan to hold onto your muscle mass stores.
Strength-building exercises help you retain muscle. BearFotos/Shutterstock But you don’t need to hit the gym. Exercises using body weight – such as push-ups, pull-ups, planks and air squats – are just as effective as lifting weights and using strength-building equipment.
Encouragingly, moderate-volume resistance training (three sets of ten repetitions for eight exercises) can be as effective as high-volume training (five sets of ten repetitions for eight exercises) for maintaining muscle when you’re following a calorie-restricted diet.
2. Eat more protein
Foods high in protein play an essential role in building and maintaining muscle mass, but research also shows these foods help prevent muscle loss when you’re following a calorie-restricted diet.
But this doesn’t mean just eating foods with protein. Meals need to be balanced and include a source of protein, wholegrain carb and healthy fat to meet our dietary needs. For example, eggs on wholegrain toast with avocado.
3. Slow your weight loss plan down
When we change our diet to lose weight, we take our body out of its comfort zone and trigger its survival response. It then counteracts weight loss, triggering several physiological responses to defend our body weight and “survive” starvation.
Our body’s survival mechanisms want us to regain lost weight to ensure we survive the next period of famine (dieting). Research shows that more than half of the weight lost by participants is regained within two years, and more than 80% of lost weight is regained within five years.
However, a slow and steady, stepped approach to weight loss, prevents our bodies from activating defence mechanisms to defend our weight when we try to lose weight.
Ultimately, losing weight long-term comes down to making gradual changes to your lifestyle to ensure you form habits that last a lifetime.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Charles Perkins Centre Research Program Leader, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
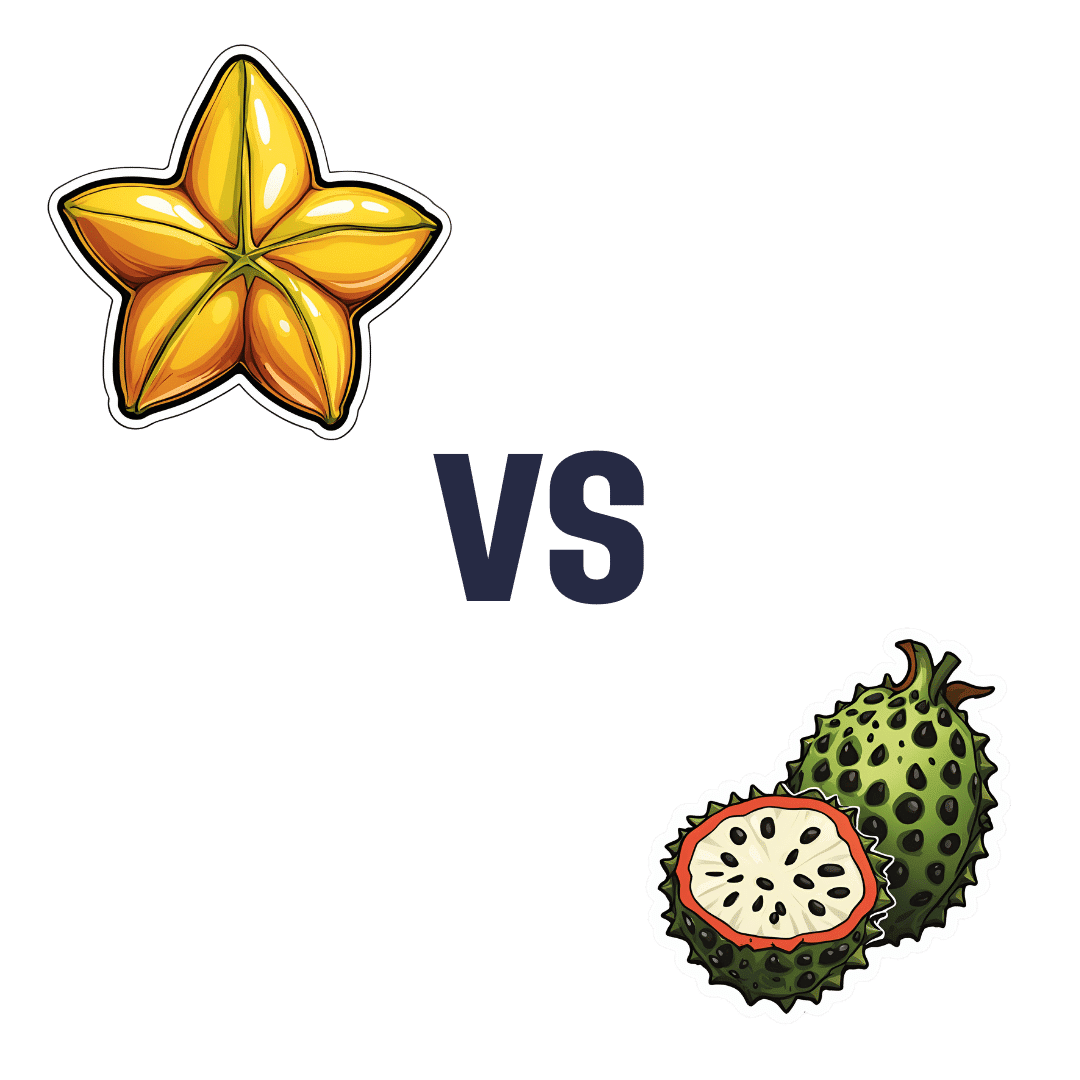
Starfruit vs Soursop – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing starfruit to soursop, we picked the soursop.
Why?
First, by starfruit, we also mean carambola, which is a different name for the same fruit, and by soursop we also mean graviola/guyabano/guanábana, which are different namers for the same fruit. Now, as for their health qualities:
In terms of macros, the soursop has more carbs and fiber, the ratio of which also give it the lower glycemic index. So, a win for soursop here.
When it comes to vitamins, starfruit has more of vitamins A, B5, C, and E, while soursop has more of vitamins B1, B2, B3, B6, B7, B9, and K. Another win for soursop.
In the category of minerals, starfruit has slightly more copper, manganese, and zinc, while soursop has much more calcium, iron, magnesium, phosphorus, and potassium. One more win for soursop!
Adding up the sections makes for a clear and overwhelming win for soursop, but let’s address to quick safety considerations while we’re here:
- Soursop extract has been claimed to be an effective cancer treatment. It isn’t. There is no evidence for this at all; just one unscrupulous company that spread the claims.
- Soursop contains annonacin, a neurotoxin. That sounds scary, but much like with apple seeds and cyanide, the quantities you’d have to consume to suffer ill effects are absurd. Remember how capsaicin (as found in hot peppers) is also a neurotoxin, too and has many health benefits. Humans have a long and happy tradition of enjoying things that are toxic at high doses, but in small doses are neutral or even beneficial. Pretty much all things we can consume (including oxygen, and water) are toxic at sufficient doses.
In short, both of these fruits are fine and good, neither will treat cancer, but both will help to keep you in good health. As for nutritional density, the soursop wins in every category.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← soursop has no special cancer treatment properties, but actual evidence shows these fruits are beneficial (being good as a preventative, and also definitely a worthy adjunct to—but not a replacement for—mainstream anticancer therapies if you have cancer).
Take care!
Share This Post
-
Reading At Night: Good Or Bad For Sleep? And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Would be interested in your views about “reading yourself to sleep”. I find that current affairs magazines and even modern novels do exactly the opposite. But Dickens – ones like David Copperfield and Great Expectations – I find wonderfully effective. It’s like entering a parallel universe where none of your own concerns matter. Any thoughts on the science that may explain this?!❞
Anecdotally: this writer is (like most writers) a prolific reader, and finds reading some fiction last thing at night is a good way to create a buffer between the affairs of the day and the dreams of night—but I could never fall asleep that way, unless I were truly sleep-deprived. The only danger is if I “one more chapter” my way deep into the night! For what it’s worth, bedtime reading for me means a Kindle self-backlit with low, soft lighting.
Scientifically: this hasn’t been a hugely researched area, but there are studies to work from. But there are two questions at hand (at least) here:
- one is about reading, and
- the other is about reading from electronic devices with or without blue light filters.
Here’s a study that didn’t ask the medium of the book, and concluded that reading a book in bed before going to sleep improved sleep quality, compared to not reading a book in bed:
Here’s a study that concluded that reading on an iPad (with no blue light filter) that found no difference in any metrics except EEG (so, there was no difference on time spent in different sleep states or sleep onset latency), but advised against it anyway because of the EEG readings (which showed slow wave activity being delayed by approximately 30 minutes, which is consistent with melatonin production mechanics):
Here’s another study that didn’t take EEG readings, and/but otherwise confirmed no differences being found:
We’re aware this goes against general “sleep hygiene” advice in two different ways:
- General advice is to avoid electronic devices before bedtime
- General advice is to not do activities besides sleep (and sex) in bed
…but, we’re committed to reporting the science as we find it!
Enjoy!
Share This Post
Related Posts
-
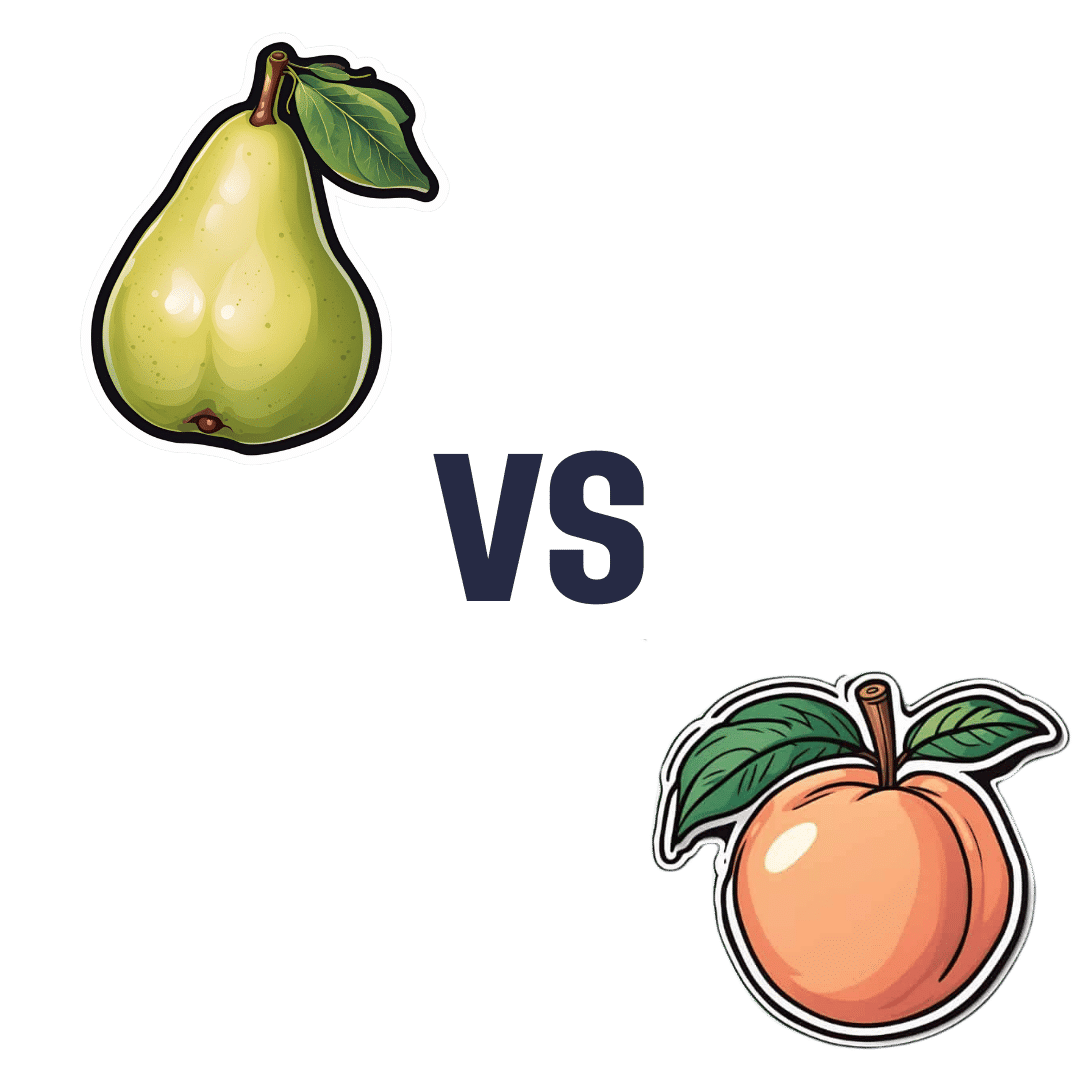
Pear vs Peach – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pears to peaches, we picked the peaches.
Why?
Both are great! But peaches are exceptional in some ways that pears just can’t match up to:
In terms of macros, pears have more carbs and fiber, the ratio of which results in an approximately equal glycemic index. Thus, we’ll say that pears win this round by virtue of being the nutritionally denser option.
Looking at the vitamins, pears have (slightly) more of vitamins B6, B9, and K, while peaches have (much) more of vitamins A, B1, B2, B3, B5, B7, C, E, and choline—thus sweeping this category easily for peaches.
In the category of minerals, pears have more calcium and copper, while peaches have more iron, magnesium, manganese, phosphorus, potassium, and zinc. This time, the margins of difference for each mineral are comparably low (i.e. pears are close behind peaches on all those minerals), but still, by strength of numbers, it’s a clear win for peaches.
When it comes to polyphenols, not only do peaches have more, but also, they have anticancer properties that pears don’t—see our link below for more about that!
Meanwhile, adding up the sections makes for an overall win for peaches, but as ever when it comes to fruits, by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← peaches in the #2 spot! They induce cell death in cancer cells while sparing healthy ones
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s the difference between physical and chemical sunscreens? And which one should you choose?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sun exposure can accelerate ageing, cause skin burns, erythema (a skin reaction), skin cancer, melasmas (or sun spots) and other forms of hyperpigmentation – all triggered by solar ultraviolet radiation.
Approximately 80% of skin cancer cases in people engaged in outdoor activities are preventable by decreasing sun exposure. This can be done in lots of ways including wearing protective clothing or sunscreens.
But not all sunscreens work in the same way. You might have heard of “physical” and “chemical” sunscreens. What’s the difference and which one is right for you?
How sunscreens are classified
Sunscreens are grouped by their use of active inorganic and organic ultraviolet (UV) filters. Chemical sunscreens use organic filters such as cinnamates (chemically related to cinnamon oil) and benzophenones. Physical sunscreens (sometimes called mineral sunscreens) use inorganic filters such as titanium and zinc oxide.
These filters prevent the effects of UV radiation on the skin.
Organic UV filters are known as chemical filters because the molecules in them change to stop UV radiation reaching the skin. Inorganic UV filters are known as physical filters, because they work through physical means, such as blocking, scattering and reflection of UV radiation to prevent skin damage.
Nano versus micro
The effectiveness of the filters in physical sunscreen depends on factors including the size of the particle, how it’s mixed into the cream or lotion, the amount used and the refraction index (the speed light travels through a substance) of each filter.
When the particle size in physical sunscreens is large, it causes the light to be scattered and reflected more. That means physical sunscreens can be more obvious on the skin, which can reduce their cosmetic appeal.
Nanoparticulate forms of physical sunscreens (with tiny particles smaller than 100 nanometers) can improve the cosmetic appearance of creams on the skin and UV protection, because the particles in this size range absorb more radiation than they reflect. These are sometimes labelled as “invisible” zinc or mineral formulations and are considered safe.
So how do chemical sunscreens work?
Chemical UV filters work by absorbing high-energy UV rays. This leads to the filter molecules interacting with sunlight and changing chemically.
When molecules return to their ground (or lower energy) state, they release energy as heat, distributed all over the skin. This may lead to uncomfortable reactions for people with skin sensitivity.
Generally, UV filters are meant to stay on the epidermis (the first skin layer) surface to protect it from UV radiation. When they enter into the dermis (the connective tissue layer) and bloodstream, this can lead to skin sensitivity and increase the risk of toxicity. The safety profile of chemical UV filters may depend on whether their small molecular size allows them to penetrate the skin.
Chemical sunscreens, compared to physical ones, cause more adverse reactions in the skin because of chemical changes in their molecules. In addition, some chemical filters, such as dibenzoylmethane tend to break down after UV exposure. These degraded products can no longer protect the skin against UV and, if they penetrate the skin, can cause cell damage.
Due to their stability – that is, how well they retain product integrity and effectiveness when exposed to sunlight – physical sunscreens may be more suitable for children and people with skin allergies.
Although sunscreen filter ingredients can rarely cause true allergic dermatitis, patients with photodermatoses (where the skin reacts to light) and eczema have higher risk and should take care and seek advice.
What to look for
The best way to check if you’ll have a reaction to a physical or chemical sunscreen is to patch test it on a small area of skin.
And the best sunscreen to choose is one that provides broad-spectrum protection, is water and sweat-resistant, has a high sun protection factor (SPF), is easy to apply and has a low allergy risk.
Health authorities recommend sunscreen to prevent sun damage and cancer. Chemical sunscreens have the potential to penetrate the skin and may cause irritation for some people. Physical sunscreens are considered safe and effective and nanoparticulate formulations can increase their appeal and ease of use.
Yousuf Mohammed, Dermatology researcher, The University of Queensland and Khanh Phan, Postdoctoral research associate, Frazer Institute, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Skincare – by Caroline Hirons
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our skin is our largest organ, and it affects (and is affected by) most of what it contains. In other words, us.
So how do we look after this organ? Caroline Hirons lays it bare for us, in this very clear (and well-illustrated with many photos) book that gives a ground-upwards explanation of:
- Our skin’s layers and features and what they do
- The many ways our skin can be different from others
- What lifestyle factors to worry about (or not)
- What exactly the many kinds of skincare products do
- How to understand which ones are actually for our skin
- How to craft the ideal skincare routine for any individual
- What should go into a personalized skincare kit
Because, as it turns out, shockingly we can’t trust advertising. Not only is it advertising, but also, they don’t know us. What will be perfect for one person’s skin may ruin another’s, and labels can be very misleading.
A strength of this book is how Hirons demystifies all that, so we can ignore the claims and just know what a product will actually do, from its ingredients.
She also covers the changes that occur in various life processes, including puberty, pregnancy, menopause, and just plain aging. In other words, what to do when what’s been working suddenly doesn’t anymore.
Bottom line: this is a great book for anyone (though: especially those of us with female hormones) who wants to understand the skin you’re in and how to keep it well-nourished and glowingly healthy.
Click here to check out “Skincare” and take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: