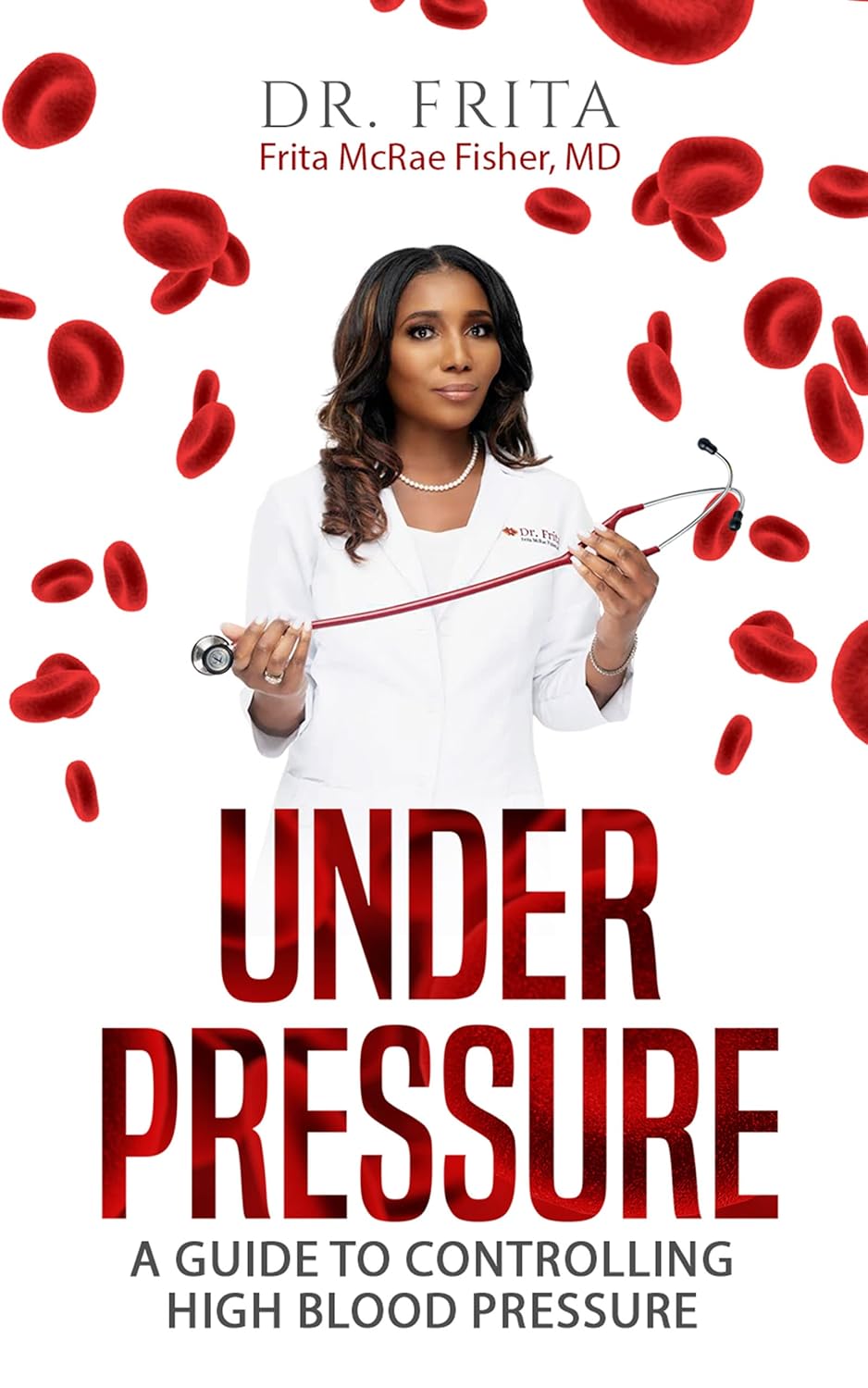
Under Pressure: A Guide To Controlling High Blood Pressure – by Dr. Frita Fisher
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hypertension kills a lot of people, and does so with little warning—it can be asymptomatic before it gets severe enough to cause harm, and once it causes harm, well, one heart attack or stroke is already one too many.
Aimed more squarely at people in the 35–45 danger zone (young enough to not be getting regular blood pressure checks, old enough that it may have been building up for decades), this is a very good primer on blood pressure, factors affecting it, what goes wrong, what to do about it, and how to make a good strategy for managing it for life.
The style is easy-reading, making this short (91 pages) book a very quick read, but an informative one.
Bottom line: if you are already quite knowledgeable about blood pressure and blood pressure management, this one’s probably not for you. But if you’re in the category of “what do those numbers mean again?”, then this is a very handy book to have, to get you up to speed so that you can handle things as appropriate.
Click here to check out Under Pressure, and get/keep yours under control!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Should We Skip Shampoo?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝What’s the science on “no poo”? Is it really better for hair? There are so many mixed reports out there.❞
First, for any unfamiliar: this is not about constipation; rather, it is about skipping shampoo, and either:
- Using an alternative cleaning agent, such as vinegar and/or sodium bicarbonate
- Using nothing at all, just conditioner when wet and brushing when dry
Let’s examine why the trend became a thing: the thinking went “shampoo does not exist in nature, and most of our body is more or less self-cleaning; shampoos remove oils from hair, and the body has to produce more sebum to compensate, resulting in a rapid cycle of dry and greasy hair”.
Now let’s fact-check each of those:
- shampoo does not exist in nature: true (except in the sense that everything that exists can be argued to exist in nature, since nature encompasses everything—but the point is that shampoo is a purely artificial human invention)
- most of our body is more or less self-cleaning: true, but our hair is not, for the same reason our nails are not: they’re not really a living part of the overall organism that is our body, so much as a keratinous protrusion of neatly stacked and hardened dead cells from our body. Dead things are not self-cleaning.
- shampoos remove oils from hair: true; that is what they were invented for and they do it well
- the body has to produce more sebum to compensate, resulting in a rapid cycle of dry and greasy hair: false; or at least, there is no evidence for this.
Our hair’s natural oils are great at protecting it, and also great at getting dirt stuck in it. For the former reason we want the oil there; for the latter reason, we don’t.
So the trick becomes: how to remove the oil (and thus the dirt stuck in it) and then put clean oil back (but not too much, because we don’t want it greasy, just, shiny and not dry)?
The popular answer is: shampoo to clean the hair, conditioner to put an appropriate amount of oil* back.
*these days, mostly not actually oil, but rather silicon-based substitutes, that do the same job of protecting hair and keeping it shiny and not brittle, without attracting so much dirt. Remember also that silicon is inert and very body safe; its molecules are simply too large to be absorbed, which is why it gets used in hair products, some skin products, and lube.
See also: Water-based Lubricant vs Silicon-based Lubricant – Which is Healthier?
If you go “no poo”, then what will happen is either you dry your hair out much worse by using vinegar or (even worse) bicarbonate of soda, or you just have oil (and any dirt stuck in it) in your hair for the life of the hair. As in, each individual strand of hair has a lifespan, and when it falls out, the dirt will go with it. But until that day, it’s staying with you, oil and dirt and all.
If you use a conditioner after using those “more natural” harsh cleaners* that aren’t shampoo, then you’ll undo a lot of the damage done, and you’ll probably be fine.
*in fact, if you’re going to skip shampoo, then instead of vinegar or bicarbonate of soda, dish soap from your kitchen may actually do less damage, because at least it’s pH-balanced. However, please don’t use that either.
If you’re going to err one way or the other with regard to pH though, erring on the side of slightly acidic is much better than slightly alkaline.
More on pH: Journal of Trichology | The Shampoo pH can Affect the Hair: Myth or Reality?
If you use nothing, then brushing a lot will mitigate some of the accumulation of dirt, but honestly, it’s never going to be clean until you clean it.
Our recommendation
When your hair seems dirty, and not before, wash it with a simple shampoo (most have far too many unnecessary ingredients; it just needs a simple detergent, and the rest is basically for marketing; to make it foam completely unnecessarily but people like foam, to make it thicker so it feels more substantial, to make it smell nice, to make it a color that gives us confidence it has ingredients in it, etc).
Then, after rinsing, enjoy a nice conditioner. Again there are usually a lot of unnecessary ingredients, but an argument can be made this time for some being more relevant as unlike with the shampoo, many ingredients are going to remain on your hair after rinsing.
Between washes, if you have long hair, consider putting some hair-friendly oil (such as argan oil or coconut oil) on the tips daily, to avoid split ends.
And if you have tight curly hair, then this advice goes double for you, because it takes a lot longer for natural oils to get from your scalp to the ends of your hair. For those of us with straight hair, it pretty much zips straight on down there within a day or two; not so if you have beautiful 4C curls to take care of!
For more on taking care of hair gently, check out:
Gentler Hair Care Options, According To Science
Take care!
Share This Post
-
We looked at over 166,000 psychiatric records. Over half showed people were admitted against their will
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Picture two people, both suffering from a serious mental illness requiring hospital admission. One was born in Australia, the other in Asia.
Hopefully, both could be treated on a voluntary basis, taking into account their individual needs, preferences and capacity to consent. If not, you might imagine they should be equally likely to receive treatment against their will (known colloquially as being “sectioned” or “scheduled”).
However, our research published in British Journal of Psychiatry Open suggests this is not the case.
In the largest study globally of its kind, we found Australians are more likely to be treated in hospital for their acute mental illness against their will if they are born overseas, speak a language other than English or are unemployed.
What we did and what we found
We examined more than 166,000 episodes of voluntary and involuntary psychiatric care in New South Wales public hospitals between 2016 and 2021. Most admissions (54%) included at least one day of involuntary care.
Being brought to hospital via legal means, such as by police or via a court order, was strongly linked to involuntary treatment.
While our study does not show why this is the case, it may be due to mental health laws. In NSW, which has similar laws to most jurisdictions in Australia, doctors may treat a person on an involuntary basis if they present with certain symptoms indicating serious mental illness (such as hallucinations and delusions) which cause them to require protection from serious harm, and there is no other less-restrictive care available. Someone who has been brought to hospital by police or the courts may be more likely to meet the legal requirement of requiring protection from serious harm.
The likelihood of involuntary care was also linked to someone’s diagnosis. A person with psychosis or organic brain diseases, such as dementia and delirium, were about four times as likely to be admitted involuntarily compared to someone with anxiety or adjustment disorders (conditions involving a severe reaction to stressors).
However, our data suggest non-clinical factors contribute to the decision to impose involuntary care.
Compared with people born in Australia, we found people born in Asia were 42% more likely to be treated involuntarily.
People born in Africa or the Middle East were 32% more likely to be treated this way.
Overall, people who spoke a language other than English were 11% more likely to receive involuntary treatment compared to those who spoke English as their first language.
Some international researchers have suggested higher rates of involuntary treatment seen in people born overseas might be due to higher rates of psychotic illness. But our research found a link between higher rates of involuntary care in people born overseas or who don’t speak English regardless of their diagnosis.
We don’t know why this is happening. It is likely to reflect a complex interplay of factors about both the people receiving treatment and the way services are provided to them.
People less likely to be treated involuntarily included those who hold private health insurance, and those referred through a community health centre or outpatients unit.
Our findings are in line with international studies. These show higher rates of involuntary treatment among people from Black and ethnic minority groups, and people living in areas of higher socioeconomic disadvantage.
A last resort? Or should we ban it?
Both the NSW and Australian mental health commissions have called involuntary psychiatric care an avoidable harm that should only be used as a last resort.
Despite this, one study found Australia’s rate of involuntary admissions has increased by 3.4% per year and it has one of the highest rates of involuntary admissions in the world.
Involuntary psychiatric treatment is also under increasing scrutiny globally.
When Australia signed up to the UN Convention on the Rights of Persons with Disabilities, it added a declaration noting it would allow for involuntary treatment of people with mental illness where such treatments are “necessary, as a last resort and subject to safeguards”.
However, the UN has rejected this, saying it is a fundamental human right “to be free from involuntary detention in a mental health facility and not to be forced to undergo mental health treatment”.
Others question if involuntary treatment could ever be removed entirely.
Where to from here?
Our research not only highlights concerns regarding how involuntary psychiatric treatment is implemented, it’s a first step towards decreasing its use. Without understanding how and when it is used it will be difficult to create effective interventions to reduce it.
But Australia is still a long way from significantly reducing involuntary treatment.
We need to provide more care options outside hospital, ones accessible to all Australians, including those born overseas, who don’t speak English, or who come from disadvantaged communities. This includes intervening early enough that people are supported to not become so unwell they end up being referred for treatment via police or the criminal justice system.
More broadly, we need to do more to reduce stigma surrounding mental illness and to ensure poverty and discrimination are tackled to help prevent more people becoming unwell in the first place.
Our study also shows we need to do more to respect the autonomy of someone with serious mental illness to choose if they are treated. That’s whether they are in NSW or other jurisdictions.
And legal reform is required to ensure more states and territories more fully reflect the principal that people who have the capacity to make such decisions should have the right to decline mental health treatment in the same way they would any other health care.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Amy Corderoy, Medical doctor and PhD candidate studying involuntary psychiatric treatment, School of Psychiatry, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
DVT Risk Management Beyond The Socks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I know I am at higher risk of DVT after having hip surgery, any advice beside compression stockings?❞
First of all, a swift and easy recovery to you!
Surgery indeed increases the risk of deep vein thrombosis (henceforth: DVT), and hip or knee surgery especially so, for obvious reasons.
There are other risk factors you can’t control, like genetics (family history of DVT as an indicator) and age, but there are some that you can, including:
- smoking (so, ideally don’t; do speak to your doctor before quitting though, in case withdrawal might be temporarily worse for you than smoking)
- obesity (so, losing weight is good if overweight, but if this is going to happen, it’ll mostly happen in the kitchen not the gym, which may be a relief as you’re probably not the very most up for exercise at present)
- See also: Lose Weight, But Healthily
- sedentariness (so, while you’re probably not running marathons right now, please do try to keep moving, even if only gently)
Beyond that, yes compression socks, but also frequent gentle massage can help a lot to avoid clots forming.
Also, no surprises, a healthy diet will help, especially one that’s good for general heart health. Check out for example the Mediterranean DASH diet:
Four Ways To Upgrade The Mediterranean Diet
Also, obviously, speak with your doctor/pharmacist if you haven’t already about possible medications, including checking whether any of your current medications increase the risk and could be swapped for something that doesn’t.
Take care!
Share This Post
Related Posts
-
Which Sugars Are Healthier, And Which Are Just The Same?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From Apples to Bees, and High-Fructose Cs
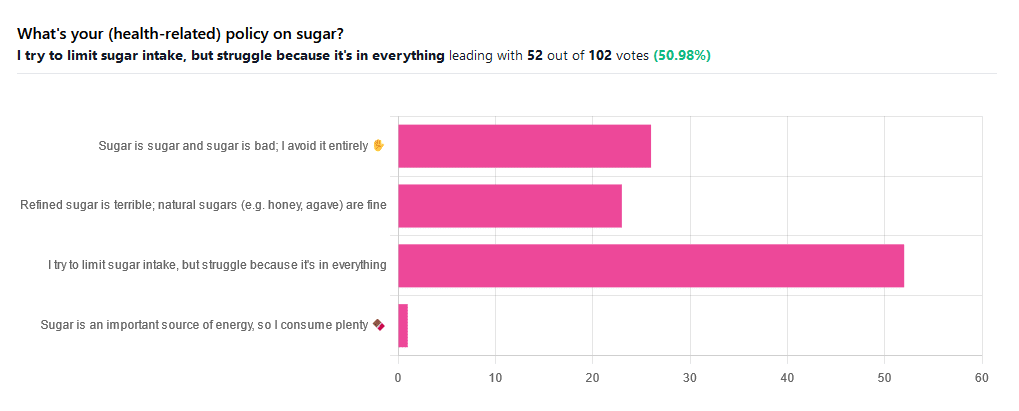
We asked you for your (health-related) policy on sugar. The trends were as follows:
- About half of all respondents voted for “I try to limit sugar intake, but struggle because it’s in everything”
- About a quarter of all respondents voted for “Refined sugar is terrible; natural sugars (e.g. honey, agave) are fine”
- About a quarter of all respondents voted for “Sugar is sugar and sugar is bad; I avoid it entirely”
- One (1) respondent voted for “Sugar is an important source of energy, so I consume plenty”
Writer’s note: I always forget to vote in these, but I’d have voted for “I try to limit sugar intake, but struggle because it’s in everything”.
Sometimes I would like to make my own [whatever] to not have the sugar, but it takes so much more time, and often money too.
So while I make most things from scratch (and typically spend about an hour cooking each day), sometimes store-bought is the regretfully practical timesaver/moneysaver (especially when it comes to condiments).
So, where does the science stand?
There has, of course, been a lot of research into the health impact of sugar.
Unfortunately, a lot of it has been funded by sugar companies, which has not helped. Conversely, there are also studies funded by other institutions with other agendas to push, and some of them will seek to make sugar out to be worse than it is.
So for today’s mythbusting overview, we’ve done our best to quality-control studies for not having financial conflicts of interest. And of course, the usual considerations of favoring high quality studies where possible Large sample sizes, good method, human subjects, that sort of thing.
Sugar is sugar and sugar is bad: True or False?
False and True, respectively.
- Sucrose is sucrose, and is generally bad.
- Fructose is fructose, and is worse.
Both ultimately get converted into glycogen (if not used immediately for energy), but for fructose, this happens mostly* in the liver, which a) taxes it b) goes very unregulated by the pancreas, causing potentially dangerous blood sugar spikes.
This has several interesting effects:
- Because fructose doesn’t directly affect insulin levels, it doesn’t cause insulin insensitivity (yay)
- Because fructose doesn’t directly affect insulin levels, this leaves hyperglycemia untreated (oh dear)
- Because fructose is metabolized by the liver and converted to glycogen which is stored there, it’s one of the main contributors to non-alcoholic fatty liver disease (at this point, we’re retracting our “yay”)
Read more: Fructose and sugar: a major mediator of non-alcoholic fatty liver disease
*”Mostly” in the liver being about 80% in the liver. The remaining 20%ish is processed by the kidneys, where it contributes to kidney stones instead. So, still not fabulous.
Fructose is very bad, so we shouldn’t eat too much fruit: True or False?
False! Fruit is really not the bad guy here. Fruit is good for you!
Fruit does contain fructose yes, but not actually that much in the grand scheme of things, and moreover, fruit contains (unless you have done something unnatural to it) plenty of fiber, which mitigates the impact of the fructose.
- A medium-sized apple (one of the most sugary fruits there is) might contain around 11g of fructose
- A tablespoon of high-fructose corn syrup can have about 27g of fructose (plus about 3g glucose)
Read more about it: Effects of high-fructose (90%) corn syrup on plasma glucose, insulin, and C-peptide in non-insulin-dependent diabetes mellitus and normal subjects
However! The fiber content (in fruit) mitigates the impact of the fructose almost entirely anyway.
And if you take fruits that are high in sugar and/but high in polyphenols, like berries, they now have a considerable net positive impact on glycemic health:
- Polyphenols and Glycemic Control
- Polyphenols and their effects on diabetes management: A review
- Dietary polyphenols as antidiabetic agents: Advances and opportunities
You may be wondering: what was that about “unless you have done something unnatural to it”?
That’s mostly about juicing. Juicing removes much (or all) of the fiber, and if you do that, you’re basically back to shooting fructose into your veins:
- Effect of Fruit Juice on Glucose Control and Insulin Sensitivity in Adults: A Meta-Analysis of 12 Randomized Controlled Trials
- Intake of Fruit, Vegetables, and Fruit Juices and Risk of Diabetes in Women
Natural sugars like honey, agave, and maple syrup, are healthier than refined sugars: True or False?
True… Sometimes, and sometimes marginally.
This is partly because of the glycemic index and glycemic load. The glycemic index scores tail off thus:
- table sugar = 65
- maple syrup = 54
- honey = 46
- agave syrup = 15
So, that’s a big difference there between agave syrup and maple syrup, for example… But it might not matter if you’re using a very small amount, which means it may have a high glycemic index but a low glycemic load.
Note, incidentally, that table sugar, sucrose, is a disaccharide, and is 50% glucose and 50% fructose.
The other more marginal health benefits come from that fact that natural sugars are usually found in foods high in other nutrients. Maple syrup is very high in manganese, for example, and also a fair source of other minerals.
But… Because of its GI, you really don’t want to be relying on it for your nutrients.
Wait, why is sugar bad again?
We’ve been covering mostly the more “mythbusting” aspects of different forms of sugar, rather than the less controversial harms it does, but let’s give at least a cursory nod to the health risks of sugar overall:
- Obesity and associated metabolic risk
- Main contributor to non-alcoholic fatty liver disease
- Increased risk of heart disease
- Insulin resistance and diabetes risk
- Cellular aging (shortened telomeres)
- 95% increased cancer risk
That last one, by the way, was a huge systematic review of 37 large longitudinal cohort studies. Results varied depending on what, specifically, was being examined (e.g. total sugar, fructose content, sugary beverages, etc), and gave up to 200% increased cancer risk in some studies on sugary beverages, but 95% increased risk is a respectable example figure to cite here, pertaining to added sugars in foods.
And finally…
The 56 Most Common Names for Sugar (Some Are Tricky)
How many did you know?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healing Cracked Fingers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Question. Suffer from cracked (split) finger tips in the cold weather. Very painful, is there something I can take to ward off this off. Appreciate your daily email.❞
Ouch, painful indeed! Aside from good hydration (which is something we easily forget in cold weather), there’s no known internal guard against this*, but from the outside, oil-based moisturizers are the way to go.
Olive oil, coconut oil, jojoba oil, and shea butter are all fine options.
If the skin is broken such that infection is possible, then starting with an antiseptic ointment/cream is sensible. A good example product is Savlon, unless you are allergic to its active ingredient chlorhexidine.
*However, if perchance you are also suffering from peripheral neuropathy (a common comorbidity of cracked skin in the extremities), then lion’s main mushroom can help with that.
Writer’s anecdote: I myself started suffering from peripheral neuropathy in my hands earlier this year, doubtlessly due to some old injuries of mine.
However, upon researching for the above articles, I was inspired to try lion’s mane mushroom for myself. I take it daily, and have now been free of symptoms of peripheral neuropathy for several months.
Here’s an example product on Amazon, by the way
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy sex drive In Our Fifties
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: What’s a healthy sex drive for someone in their 50s?
A: If you’re happy with it, it’s healthy! If you’re not, it’s not.
This means… If you’re not (happy) and thus it’s not (healthy), you have two main options:
- Find a way to be happier without changing it (i.e., change your perspective)
- Find a way to change your sex drive (presumably: “increase it”, but we don’t like to assume)
There are hormonal and pharmaceutical remedies that may help (whatever your sex), so do speak with your doctor/pharmacist.
Additionally, if a boost to sex drive is what’s wanted, then almost anything that is good for your heart will help.
We wrote about heart health yesterday:
What Matters Most For Your Heart?
That was specifically about dietary considerations, so you might also want to check out:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: