Saunas: Health Benefits (& Caveats)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Heat Is On
In Tuesday’s newsletter, we asked you your (health-related) opinion on saunas, and got the above-depicted, below-described, set of responses:

- About 53% said it is “a healthful activity with many benefits”
- About 25% said it is “best avoided; I feel like I’m dying in there”
- About 12% said “it feels good and therefore can’t be all bad”
So what does the science say?
The heat of saunas carries a health risk: True or False?
False, generally speaking, for any practical purposes. Of course, anything in life comes with a health risk, but statistically speaking, your shower at home is a lot more dangerous than a sauna (risk of slipping with no help at hand).
It took a bit of effort to find a paper on the health risks of saunas, because all the papers on PubMed etc coming up for those keywords were initially papers with “reduces the risk of…”, i.e. ways in which the sauna is healthy.
However, we did find one:
❝Contraindications to sauna bathing include unstable angina pectoris, recent myocardial infarction, and severe aortic stenosis.
Sauna bathing is safe, however, for most people with coronary heart disease with stable angina pectoris or old myocardial infarction.
Very few acute myocardial infarctions and sudden deaths occur in saunas, but alcohol consumption during sauna bathing increases the risk of hypotension, arrhythmia, and sudden death, and should be avoided. ❞
~ Dr. Matti Hannuksela & Dr. Samer Ellahham
Source: Benefits and risks of sauna bathing
So, very safe for most people, safe even for most people with heart disease, but there are exceptions so check with your own doctor of course.
And drinking alcohol anywhere is bad for the health, but in a sauna it’s a truly terrible idea. As an aside, please don’t drink alcohol in the shower, either (risk of slipping with no help at hand, and this time, broken glass too).
On the topic of it being safe for most people’s hearts, see also:
Beneficial effects of sauna bathing for heart failure patients
As an additional note, those who have a particular sensitivity to the heat, may (again please check with your own doctor, as your case may vary) actually benefit from moderate sauna use, to reduce the cardiovascular strain that your body experiences during heatwaves (remember, you can get out of a sauna more easily than you can get out of a heatwave, so for many people it’s a lot easier to do moderation and improve thermoregulatory responses):
Sauna usage can bring many health benefits: True or False?
True! Again, at least for most people. As well as the above-discussed items, here’s one for mortality rates in healthy Finnish men:
Not only that, also…
❝The Finnish saunas have the most consistent and robust evidence regarding health benefits and they have been shown to decrease the risk of health outcomes such as hypertension, cardiovascular disease, thromboembolism, dementia, and respiratory conditions; may improve the severity of musculoskeletal disorders, COVID-19, headache and flu, while also improving mental well-being, sleep, and longevity.
Finnish saunas may also augment the beneficial effects of other protective lifestyle factors such as physical activity.
The beneficial effects of passive heat therapies may be linked to their anti-inflammatory, cytoprotective and anti-oxidant properties and synergistic effects on neuroendocrine, circulatory, cardiovascular and immune function.
Passive heat therapies, notably Finnish saunas, are emerging as potentially powerful and holistic strategies to promoting health and extending the healthspan in all populations. ❞
~ Dr. Jari Laukkanen & Dr. Setor Kunutsor
(the repeated clarification of “Finnish sauna” is not a matter of fervent nationalism, by the way, but rather a matter of disambiguating it from Swedish sauna, which has some differences, most notably a lack of steam)
That reminds us: in Scandinavia, it is usual to use a sauna naked, and in Finland in particular, it is a common social activity amongst friends, coworkers, etc. In the US, many people are not so comfortable with nudity, and indeed, many places that provide saunas, may require the wearing of swimwear. But…
Just one problem: if you’re wearing swimwear because you’ve just been swimming in a pool, you now have chlorinated water soaked into your swimwear, which in the sauna, will become steam + chlorine gas. That’s not so good for your health (and is one reason, beyond tradition and simple normalization, for why swimwear is usually not permitted in Finnish saunas).
Want to read more?
You might like our previous main feature,
Turning Up The Heat Against Diabetes & Alzheimer’s ← you guessed it, sauna may be beneficial against these too
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How the stress of playing chess can be fatal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The death of a chess player in the middle of a match at the world’s most prestigious competition may have shocked those who view the game as a relaxing pastime. Kurt Meier, 67, collapsed during his final match in the tournament and died in hospital later that day. But chess, like any other game or sport, can lead to an immense amount of stress, which can be bad for a competitor’s physical health too.
We tend to associate playing sport or games with good health and well-being. And there are a countless number of studies showing playing games has an association with feeling happier. While this argument is true for recreational players, the story can be different for the elite, where success and failure are won and lost by the finest margins and where winning can mean funding and a future, and losing can mean poverty and unemployment. If this is the case, can being successful at a sport or game actually be bad for you?
Competitive anxiety
Elite competition can be stressful because the outcome is so important to the competitors. We can measure stress using a whole range of physiological indicators such as heart rate and temperature, and responses such as changes in the intensity of our emotions.
Emotions provide a warning of threat. So if you feel that achieving your goal is going to be difficult, then expect to feel intense emotions. The leading candidate that signals we are experiencing stress is anxiety, characterised by thoughts of worry, fears of dread about performance, along with accompanying physiological responses such as increased heart rate and sweaty palms. If these symptoms are experienced regularly or chronically, then this is clearly detrimental to health.
This stress response is probably not restricted to elite athletes. Intense emotions are linked to trying to achieve important goals and while it isn’t the only situation where it occurs, it is just very noticeable in sport.
The causes of stress
It makes more sense to focus on what the causes of stress are rather than where we experience it. The principle is that the more important the goal is to achieve, then the greater the propensity for the situation to intensify emotions.
Emotions intensify also by the degree of uncertainty and competing, at whatever level of a sport, is uncertain when the opposition is trying its hardest to win the contest and also has a motivation to succeed. The key point is that almost all athletes at any level can suffer bouts of stress, partly due to high levels of motivation.
A stress response is also linked to how performance is judged and reported. Potentially stressful tasks tend to be ones where performance is public and feedback is immediate. In chess – as with most sporting contests – we see who the winner is and can start celebrating success or commiserating failure as soon as the game is over.
There are many tasks which have similar features. Giving a speech in public, taking an academic examination, or taking your driving test are all examples of tasks that can illicit stress. Stress is not restricted to formal tasks but can also include social tasks. Asking a potential partner for a date, hand in marriage, and meeting the in-laws for the first time can be equally stressful.
Winning a contest or going on a date relate to higher-order goals about how we see ourselves. If we define ourselves as “being a good player” or “being attractive or likeable” then contrasting information is likely to associate with unpleasant emotions. You will feel devastated if you are turned down when asking someone out on a date, for instance, and if this was repeated, it could lead to reduced self-esteem and depression.
The key message here is to recognise what your goals are and think about how important they are. If you want to achieve them with a passion and if the act of achieving them leads to intense and sometimes unwanted emotions, then it’s worth thinking about doing some work to manage these emotions.
Andrew Lane, Professor in Sport and Learning, University of Wolverhampton
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Be Your Future Self Now – by Dr. Benjamin Hardy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Affirmations in the mirror are great and all, but they can only get you so far! And if you’re a regular reader of our newsletter, you probably know about the power of small daily habits adding up and compounding over time. So what does this book offer, that’s different?
“Be Your Future Self Now” beelines the route “from here to there”, with a sound psychological approach. On which note…
The book’s subtitle mentions “the science of intentional transformation”, and while Dr. Hardy is a psychologist, he’s an organizational psychologist (which doesn’t really pertain to this topic). It’s not a science-heavy book, but it is heavy on psychological rationality.
Where Dr. Hardy does bring psychology to bear, it’s in large part that! He teaches us how to overcome our biases that cause us to stumble blindly into the future… rather than intentfully creating our own future to step into. For example:
Most people (regardless of age!) acknowledge what a different person they were 10 years ago… but assume they’ll be basically the same person 10 years from now as they are today, just with changed circumstances.
Radical acceptance of the inevitability of change is the first step to taking control of that change.
That’s just one example, but there are many, and this is a book review not a book summary!
In short: if you’d like to take much more conscious control of the direction your life will take, this is a book for you.
Click here to get your copy of “Be Your Future Self Now” from Amazon!
Share This Post
-
10 Powerful Tips To Improve Lymph Flow – by Laurel West
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The lymphatic system is a large part of the body’s “clean-up” system, as well having an important role in fighting cancer specifically. As such, while it doesn’t get nearly as much popular attention as our circulatory system or our nervous system, say, it is critically important.
The author, a massage therapist, knows her stuff when it comes to lymph, and shows that here.
As this is a very lean book, weighing in at a mere 87 pages, you can imagine it gets straight to the point.
So will we! The titular “10 powerful tips” are:
- Drink water
- Matcha meditation
- Breathwork
- Dry brushing
- Hydrotherapy
- Stretching
- Sweating
- Lymphatic facial massage
- Advanced lymphatic massage
- Anti-inflammatory diet
Of course, she does explain each of those; some are more obvious than others; “drink water” takes less explanation than “advanced lymphatic massage”, say.
The style is, as you might expect, concise. It’s more of a primer than a textbook, and it does communicate its ideas clearly.
Bottom line: if you’d like to manage your lymph better, this book is an excellent way to get started.
Click here to check out 10 Powerful Tips To Improve Lymph Flow, and improve your lymph flow.
Share This Post
Related Posts
-
Why Many Nonprofit (Wink, Wink) Hospitals Are Rolling in Money
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One owns a for-profit insurer, a venture capital company, and for-profit hospitals in Italy and Kazakhstan; it has just acquired its fourth for-profit hospital in Ireland. Another owns one of the largest for-profit hospitals in London, is partnering to build a massive training facility for a professional basketball team, and has launched and financed 80 for-profit start-ups. Another partners with a wellness spa where rooms cost $4,000 a night and co-invests with “leading private equity firms.”
Do these sound like charities?
These diversified businesses are, in fact, some of the country’s largest nonprofit hospital systems. And they have somehow managed to keep myriad for-profit enterprises under their nonprofit umbrella — a status that means they pay little or no taxes, float bonds at preferred rates, and gain numerous other financial advantages.
Through legal maneuvering, regulatory neglect, and a large dollop of lobbying, they have remained tax-exempt charities, classified as 501(c)(3)s.
“Hospitals are some of the biggest businesses in the U.S. — nonprofit in name only,” said Martin Gaynor, an economics and public policy professor at Carnegie Mellon University. “They realized they could own for-profit businesses and keep their not-for-profit status. So the parking lot is for-profit; the laundry service is for-profit; they open up for-profit entities in other countries that are expressly for making money. Great work if you can get it.”
Many universities’ most robust income streams come from their technically nonprofit hospitals. At Stanford University, 62% of operating revenue in fiscal 2023 was from health services; at the University of Chicago, patient services brought in 49% of operating revenue in fiscal 2022.
To be sure, many hospitals’ major source of income is still likely to be pricey patient care. Because they are nonprofit and therefore, by definition, can’t show that thing called “profit,” excess earnings are called “operating surpluses.” Meanwhile, some nonprofit hospitals, particularly in rural areas and inner cities, struggle to stay afloat because they depend heavily on lower payments from Medicaid and Medicare and have no alternative income streams.
But investments are making “a bigger and bigger difference” in the bottom line of many big systems, said Ge Bai, a professor of health care accounting at the Johns Hopkins University Bloomberg School of Public Health. Investment income helped Cleveland Clinic overcome the deficit incurred during the pandemic.
When many U.S. hospitals were founded over the past two centuries, mostly by religious groups, they were accorded nonprofit status for doling out free care during an era in which fewer people had insurance and bills were modest. The institutions operated on razor-thin margins. But as more Americans gained insurance and medical treatments became more effective — and more expensive — there was money to be made.
Not-for-profit hospitals merged with one another, pursuing economies of scale, like joint purchasing of linens and surgical supplies. Then, in this century, they also began acquiring parts of the health care systems that had long been for-profit, such as doctors’ groups, as well as imaging and surgery centers. That raised some legal eyebrows — how could a nonprofit simply acquire a for-profit? — but regulators and the IRS let it ride.
And in recent years, partnerships with, and ownership of, profit-making ventures have strayed further and further afield from the purported charitable health care mission in their community.
“When I first encountered it, I was dumbfounded — I said, ‘This not charitable,’” said Michael West, an attorney and senior vice president of the New York Council of Nonprofits. “I’ve long questioned why these institutions get away with it. I just don’t see how it’s compliant with the IRS tax code.” West also pointed out that they don’t act like charities: “I mean, everyone knows someone with an outstanding $15,000 bill they can’t pay.”
Hospitals get their tax breaks for providing “charity care and community benefit.” But how much charity care is enough and, more important, what sort of activities count as “community benefit” and how to value them? IRS guidance released this year remains fuzzy on the issue.
Academics who study the subject have consistently found the value of many hospitals’ good work pales in comparison with the value of their tax breaks. Studies have shown that generally nonprofit and for-profit hospitals spend about the same portion of their expenses on the charity care component.
Here are some things listed as “community benefit” on hospital systems’ 990 tax forms: creating jobs; building energy-efficient facilities; hiring minority- or women-owned contractors; upgrading parks with lighting and comfortable seating; creating healing gardens and spas for patients.
All good works, to be sure, but health care?
What’s more, to justify engaging in for-profit business while maintaining their not-for-profit status, hospitals must connect the business revenue to that mission. Otherwise, they pay an unrelated business income tax.
“Their CEOs — many from the corporate world — spout drivel and turn somersaults to make the case,” said Lawton Burns, a management professor at the University of Pennsylvania’s Wharton School. “They do a lot of profitable stuff — they’re very clever and entrepreneurial.”
The truth is that a number of not-for-profit hospitals have become wealthy diversified business organizations. The most visible manifestation of that is outsize executive compensation at many of the country’s big health systems. Seven of the 10 most highly paid nonprofit CEOs in the United States run hospitals and are paid millions, sometimes tens of millions, of dollars annually. The CEOs of the Gates and Ford foundations make far less, just a bit over $1 million.
When challenged about the generous pay packages — as they often are — hospitals respond that running a hospital is a complicated business, that pharmaceutical and insurance execs make much more. Also, board compensation committees determine the payout, considering salaries at comparable institutions as well as the hospital’s financial performance.
One obvious reason for the regulatory tolerance is that hospital systems are major employers — the largest in many states (including Massachusetts, Pennsylvania, Minnesota, Arizona, and Delaware). They are big-time lobbying forces and major donors in Washington and in state capitals.
But some patients have had enough: In a suit brought by a local school board, a judge last year declared that four Pennsylvania hospitals in the Tower Health system had to pay property taxes because its executive pay was “eye popping” and it demonstrated “profit motives through actions such as charging management fees from its hospitals.”
A 2020 Government Accountability Office report chided the IRS for its lack of vigilance in reviewing nonprofit hospitals’ community benefit and recommended ways to “improve IRS oversight.” A follow-up GAO report to Congress in 2023 said, “IRS officials told us that the agency had not revoked a hospital’s tax-exempt status for failing to provide sufficient community benefits in the previous 10 years” and recommended that Congress lay out more specific standards. The IRS declined to comment for this column.
Attorneys general, who regulate charity at the state level, could also get involved. But, in practice, “there is zero accountability,” West said. “Most nonprofits live in fear of the AG. Not hospitals.”
Today’s big hospital systems do miraculous, lifesaving stuff. But they are not channeling Mother Teresa. Maybe it’s time to end the community benefit charade for those that exploit it, and have these big businesses pay at least some tax. Communities could then use those dollars in ways that directly benefit residents’ health.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
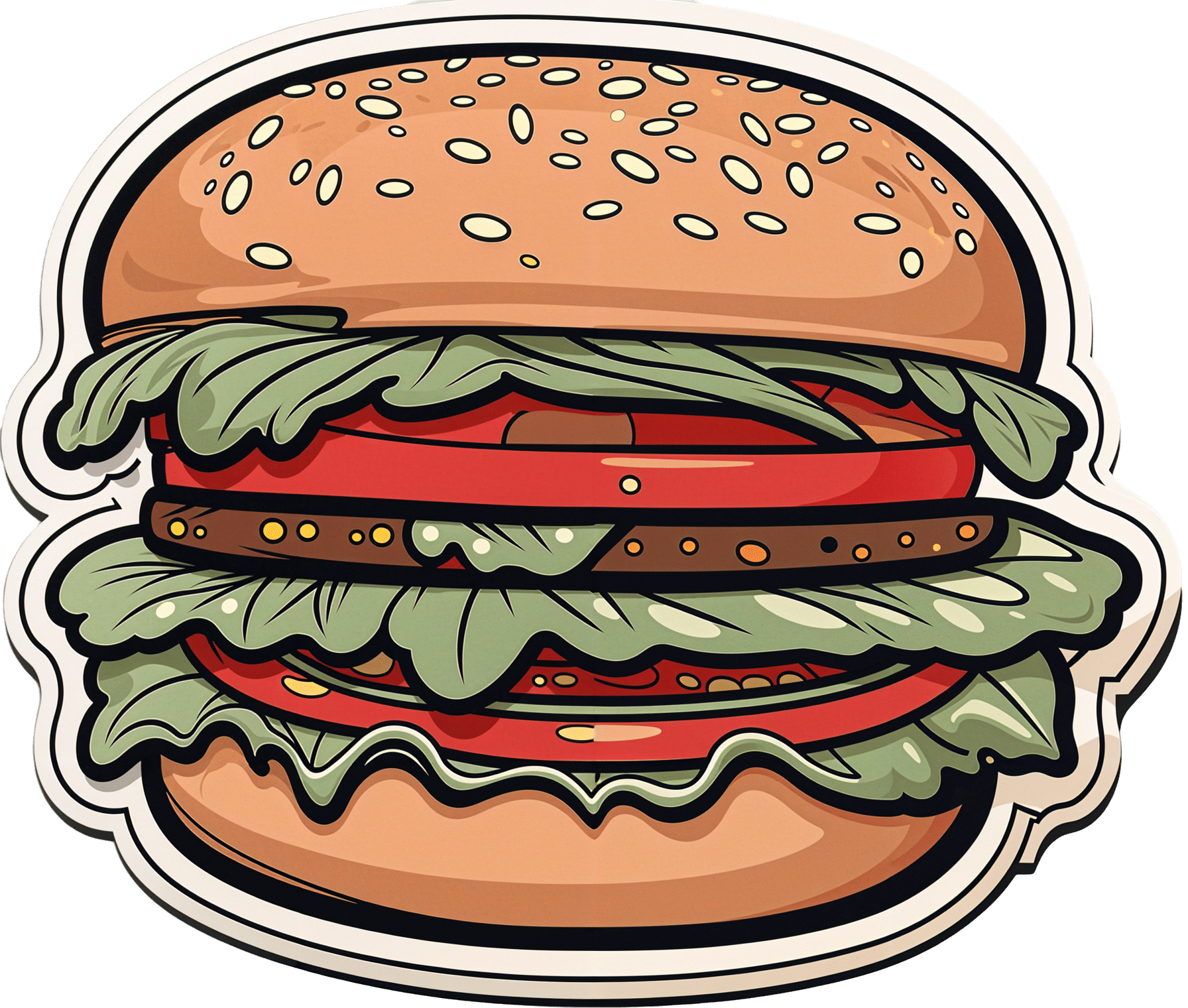
Are plant-based burgers really bad for your heart? Here’s what’s behind the scary headlines
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’re hearing a lot about ultra-processed foods and the health effects of eating too many. And we know plant-based foods are popular for health or other reasons.
So it’s not surprising new research out this week including the health effects of ultra-processed, plant-based foods is going to attract global attention.
And the headlines can be scary if that research and the publicity surrounding it suggests eating these foods increases your risk of heart disease, stroke or dying early.
Here’s how some media outlets interpreted the research. The Daily Mail ran with:
Vegan fake meats are linked to increase in heart deaths, study suggests: Experts say plant-based diets can boost health – but NOT if they are ultra-processed
The New York Post’s headline was:
Vegan fake meats linked to heart disease, early death: study
But when we look at the study itself, it seems the media coverage has focused on a tiny aspect of the research, and is misleading.
So does eating supermarket plant-based burgers and other plant-based, ultra-processed foods really put you at greater risk of heart disease, stroke and premature death?
Here’s what prompted the research and what the study actually found.
Nina Firsova/Shutterstock Remind me, what are ultra-processed foods?
Ultra-processed foods undergo processing and reformulation with additives to enhance flavour, shelf-life and appeal. These include everything from packet macaroni cheese and pork sausages, to supermarket pastries and plant-based mince.
There is now strong and extensive evidence showing ultra-processed foods are linked with an increased risk of many physical and mental chronic health conditions.
Although researchers question which foods should be counted as ultra-processed, or if all of them are linked to poorer health, the consensus is that, generally, we should be eating less of them.
We also know plant-based diets are popular. These are linked with a reduced risk of chronic health conditions such as heart disease and stroke, cancer and diabetes. And supermarkets are stocking more plant-based, ultra-processed food options.
How about the new study?
The study looked for any health differences between eating plant-based, ultra-processed foods compared to eating non-plant based, ultra-processed foods. The researchers focused on the risk of cardiovascular disease (such as heart disease and stroke) and deaths from it.
Plant-based, ultra-processed foods in this study included mass-produced packaged bread, pastries, buns, cakes, biscuits, cereals and meat alternatives (fake meats). Ultra-processed foods that were not plant-based included milk-based drinks and desserts, sausages, nuggets and other reconstituted meat products.
The researchers used data from the UK Biobank. This is a large biomedical database that contains de-identified genetic, lifestyle (diet and exercise) and health information and biological samples from half a million UK participants. This databank allows researchers to determine links between this data and a wide range of diseases, including heart disease and stroke.
They used data from nearly 127,000 people who provided details of their diet between 2009 and 2012. The researchers linked this to their hospital records and death records. On average, the researchers followed each participant’s diet and health for nine years.
Plant-based, ultra-processed foods included in this study included packaged supermarket bread. doublelee/Shutterstock What did the study find?
With every 10% increase of total energy from plant-sourced, ultra-processed foods there was an associated 5% increased risk of cardiovascular disease (such as heart disease or stroke) and a 12% higher risk of dying from cardiovascular disease.
But for every 10% increase in plant-sourced, non-ultra-processed foods consumed there was an associated 7% lower risk of cardiovascular disease and a 13% lower risk of dying from cardiovascular disease.
The researchers found no evidence for an association between all plant-sourced foods (whether or not they were ultra-processed) and either an increased or decreased risk of cardiovascular disease or dying from it.
This was an observational study, where people recalled their diet using questionnaires. When coupled with other data, this can only tell us if someone’s diet is associated with a particular risk of a health outcome. So we cannot say that, in this case, the ultra-processed foods caused the heart disease and deaths from it.
Why has media coverage focused on fake meats?
Much of the media coverage has focused on the apparent health risks associated with eating fake meats, such as sausages, burgers, nuggets and even steaks.
These are considered ultra-processed foods. They are made by deconstructing whole plant foods such as pea, soy, wheat protein, nuts and mushrooms, and extracting the protein. They are then reformulated with additives to make the products look, taste and feel like traditional red and white meats.
However this was only one type of plant-based, ultra-processed food analysed in this study. This only accounted for an average 0.2% of the dietary energy intake of all the participants.
Compare this to bread, pastries, buns, cakes and biscuits, which are other types of plant-based, ultra-processed foods. These accounted for 20.7% of total energy intake in the study.
This image was at the top of the media release. Screenshot/Imperial It’s hard to say why the media focused on fake meat. But there is one clue in the media release issued to promote the research.
Although the media release did not mention the words “fake meat”, an image of plant-based burgers, sausages and meat balls or rissoles featured prominently.
The introduction of the study itself also mentions plant-sourced, ultra-processed foods, such as sausages, nuggets and burgers.
So it’s no wonder people can be confused.
Does this mean fake meats are fine?
Not necessarily. This study analysed the total intake of plant-based, ultra-processed foods, which included fake meats, albeit a very small proportion of people’s diets.
From this study alone we cannot tell if there would be a different outcome if someone ate large amounts of fake meats.
In fact, a recent review of fake meats found there was not enough evidence to determine their impact on health.
We also need more recent data to reflect current eating patterns of fake meats. This study used dietary data collected from 2009 to 2012, and fake meats have become more popular since.
What if I really like fake meat?
We have known for a while that ultra-processed foods can harm our health. This study tells us that regardless if an ultra-processed food is plant-based or not, it may still be harmful.
We know fake meat can contain large amounts of saturated fats (from coconut or palm oil), salt and sugar.
So like other ultra-processed foods, they should be eaten infrequently. The Australian Dietary Guidelines currently recommends people should only consume foods like this sometimes and in small amounts.
Are some fake meats healthier than others?
Check the labels and nutrition information panels. Look for those lowest in fat and salt. Burgers and sausages that are a “pressed cake” of minced ingredients such as nuts, beans and vegetables will be preferable to reformulated products that look identical to meat.
You can also eat whole plant-based protein foods such as legumes. These include beans, lentils, chickpeas and soy beans. As well as being high in protein and fibre, they also provide essential nutrients such as iron and zinc. Using spices and mushrooms alongside these in your recipes can replicate some of the umami taste associated with meat.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Joy of Movement – by Dr. Kelly McGonigal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We know that exercise is good for us. Obviously. We know that that exercise will make us feel good. In principle.
So why is that exercise bike wearing the laundry instead, or the weights bench gathering dust?
Dr. Kelly McGonigal explores our relationship with exercise, both the formal (organized, planned, exercise that looks like exercise) and the informal (ad hoc, casual, exercise that looks like just having a nice time).
Moreover: she starts with the why, and moves to the how. The trick she plays on us here is to get us very fired up on the many tangible benefits that will make a big difference in all areas of our lives… And then shows us how easy it can be to unlock those, and how we can make it even easier.
And as to making it stick? Exercise can be addictive, and/but it’s one of the few addictions that is almost always healthful rather than deleterious. And, there are tricks we can use to heighten that, thresholds that once we pass, we just keep going.
She also looks at the evolutionary tendency of exercise to be connection-building, as part of a community, friend group, or couple.
And, yes, she gives attention also to undertaking exercise when circumstances aren’t ideal, or our bodies simply won’t allow certain things.
In short: if any book can get you shaking off the cobwebs, this is the one.
Click here to check out The Joy Of Movement on Amazon today, and get your body moving!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: