Pneumonia: Prevention Is Better Than Cure
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pneumonia: What We Can & Can’t Do About It
Pneumonia is a significant killer of persons over the age of 65, with the risk increasing with age after that, rising very sharply around the age of 85:
While pneumonia is treatable, especially in young healthy adults, the risks get more severe in the older age brackets, and it’s often the case that someone goes into hospital with one thing, then develops pneumonia, which the person was already not in good physical shape to fight, because of whatever hospitalized them in the first place:
American Lung Association | Pneumonia Treatment and Recovery
Other risk factors besides age
There are a lot of things that can increase our risk factor for pneumonia; they mainly fall into the following categories:
- Autoimmune diseases
- Other diseases of the immune system (e.g. HIV)
- Medication-mediated immunosuppression (e.g. after an organ transplant)
- Chronic lung diseases (e.g. asthma, COPD, Long Covid, emphysema, etc)
- Other serious health conditions ← we know this one’s broad, but it encompasses such things as diabetes, heart disease, and cancer
See also:
Why Chronic Obstructive Pulmonary Disease (COPD) Is More Likely Than You Think
Things we can do about it
When it comes to risks, we can’t do much about our age and some of the other above factors, but there are other things we can do to reduce our risk, including:
- Get vaccinated against pneumonia if you are over 65 and/or have one of the aforementioned risk factors. This is not perfect (it only reduces the risk for certain kinds of infection) and may not be advisable for everyone (like most vaccines, it can put the body through its paces a bit after taking it), so speak with your own doctor about this, of course.
- See also: Vaccine Mythbusting
- Avoid contagion. While pneumonia itself is not spread person-to-person, it is caused by bacteria or viruses (there are numerous kinds) that are opportunistic and often become a secondary infection when the immune system is already busy with the first one. So, if possible avoid being in confined spaces with many people, and do wash your hands regularly (as a lot of germs are transferred that way and can get into the respiratory tract because you touched your face or such).
- See also: The Truth About Handwashing
- If you have a cold, or flu, or other respiratory infection, take it seriously, rest well, drink fluids, get good immune-boosting nutrients. There’s no such thing as “just a cold”; not anymore.
- Look after your general health too—health doesn’t exist in a vacuum, and nor does disease. Every part of us affects every other part of us, so anything that can be in good order, you want to be in good order.
This last one, by the way? It’s an important reminder that while some diseases (such as some of the respiratory infections that can precede pneumonia) are seasonal, good health isn’t.
We need to take care of our health as best we can every day along the way, because we never know when something could change.
Want to do more?
Check out: Seven Things To Do For Good Lung Health!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is ADHD Being Over-Diagnosed For Cash?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is ADHD Being Systematically Overdiagnosed?
The BBC’s investigative “Panorama” program all so recently did a documentary in which one of their journalists—who does not have ADHD—went to three private clinics and got an ADHD diagnosis from each of them:
- The BBC documentary: Private ADHD Clinics Exposed (28 mins)
- Their “5 Minutes” version: ADHD Undercover: How I Was Misdiagnosed (6 mins)
So… Is it really a case of show up, pay up, and get a shiny new diagnosis?
The BBC Panorama producers cherry-picked 3 private providers, and during those clinical assessments, their journalist provided answers that would certainly lead to a diagnosis.
This was contrasted against a three-hour assessment with an NHS psychiatrist—something that rarely happens in the NHS. Which prompts the question…
How did he walk into a 3-hour psychiatrist assessment, when most people have to wait in long waiting lists for a much more cursory appointment first with assorted gatekeepers, before going on another long waiting list, for an also-much-shorter appointment with a psychiatrist?
That would be because the NHS psychiatrist was given advance notification that this was part of an investigation and would be filmed (the private clinics were not gifted the same transparency)
So, maybe just a tad unequal treatment!
In case you’re wondering, here’s what that very NHS psychiatrist had to say on the topic:
Is it really too easy to be diagnosed with ADHD?
(we’ll give you a hint—remember Betteridge’s Law!)
❝Since the documentary aired, I have heard from people concerned that GPs could now be more likely to question legitimate diagnoses.
But as an NHS psychiatrist it is clear to me that the root of this issue is not overdiagnosis.
Instead, we are facing the combined challenges of remedying decades of underdiagnosis and NHS services that were set up when there was little awareness of ADHD.❞
~ Dr. Mike Smith, Psychiatrist
The ADHD foundation, meanwhile, has issued its own response, saying:
❝We are disappointed that BBC Panorama has opted to broadcast a poorly researched, sensationalist piece of television journalism.❞
Share This Post
-
Chatter – by Dr. Ethan Kross
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is about much more than just one’s internal monologue. It does tackle that, but also the many non-verbal rabbit-holes that our brains can easily disappear into.
The author is an experimental psychologist, and brings his professional knowledge and experience to bear on this problem—citing many studies, including his own studies from his own lab, in which he undertook to answer precisely the implicit questions of “How can I…” in terms of tackling these matters, from root anxiety (for example) to end-state executive dysfunction (for example).
The writing style isn’t dense science though, and is very approachable for all.
The greatest value in this book lies in its prescriptive element, that is to say, its advice, especially in the category of evidence-based things we can do to improve matters for ourselves; beyond generic things like “mindfulness-based stress reduction” to much more specific things like “observe yourself in the 3rd person for a moment” and “take a break to imagine looking back on this later” and “interrupt yourself with a brief manual task”. With these sorts of interventions and more, we can shift the voice in our head from critic to coach.
Bottom line: if you would like your brain to let you get on with the things you actually want to do instead of constantly sidetracking you, this is the book for you.
Share This Post
-
What will aged care look like for the next generation? More of the same but higher out-of-pocket costs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aged care financing is a vexed problem for the Australian government. It is already underfunded for the quality the community expects, and costs will increase dramatically. There are also significant concerns about the complexity of the system.
In 2021–22 the federal government spent A$25 billion on aged services for around 1.2 million people aged 65 and over. Around 60% went to residential care (190,000 people) and one-third to home care (one million people).
The final report from the government’s Aged Care Taskforce, which has been reviewing funding options, estimates the number of people who will need services is likely to grow to more than two million over the next 20 years. Costs are therefore likely to more than double.
The taskforce has considered what aged care services are reasonable and necessary and made recommendations to the government about how they can be paid for. This includes getting aged care users to pay for more of their care.
But rather than recommending an alternative financing arrangement that will safeguard Australians’ aged care services into the future, the taskforce largely recommends tidying up existing arrangements and keeping the status quo.
No Medicare-style levy
The taskforce rejected the aged care royal commission’s recommendation to introduce a levy to meet aged care cost increases. A 1% levy, similar to the Medicare levy, could have raised around $8 billion a year.
The taskforce failed to consider the mix of taxation, personal contributions and social insurance which are commonly used to fund aged care systems internationally. The Japanese system, for example, is financed by long-term insurance paid by those aged 40 and over, plus general taxation and a small copayment.
Instead, the taskforce puts forward a simple, pragmatic argument that older people are becoming wealthier through superannuation, there is a cost of living crisis for younger people and therefore older people should be required to pay more of their aged care costs.
Separating care from other services
In deciding what older people should pay more for, the taskforce divided services into care, everyday living and accommodation.
The taskforce thought the most important services were clinical services (including nursing and allied health) and these should be the main responsibility of government funding. Personal care, including showering and dressing were seen as a middle tier that is likely to attract some co-payment, despite these services often being necessary to maintain independence.
The task force recommended the costs for everyday living (such as food and utilities) and accommodation expenses (such as rent) should increasingly be a personal responsibility.
Aged care users will pay more of their share for cooking and cleaning.
Lizelle Lotter/ShutterstockMaking the system fairer
The taskforce thought it was unfair people in residential care were making substantial contributions for their everyday living expenses (about 25%) and those receiving home care weren’t (about 5%). This is, in part, because home care has always had a muddled set of rules about user co-payments.
But the taskforce provided no analysis of accommodation costs (such as utilities and maintenance) people meet at home compared with residential care.
To address the inefficiencies of upfront daily fees for packages, the taskforce recommends means testing co-payments for home care packages and basing them on the actual level of service users receive for everyday support (for food, cleaning, and so on) and to a lesser extent for support to maintain independence.
It is unclear whether clinical and personal care costs and user contributions will be treated the same for residential and home care.
Making residential aged care sustainable
The taskforce was concerned residential care operators were losing $4 per resident day on “hotel” (accommodation services) and everyday living costs.
The taskforce recommends means tested user contributions for room services and everyday living costs be increased.
It also recommends that wealthier older people be given more choice by allowing them to pay more (per resident day) for better amenities. This would allow providers to fully meet the cost of these services.
Effectively, this means daily living charges for residents are too low and inflexible and that fees would go up, although the taskforce was clear that low-income residents should be protected.
Moving from buying to renting rooms
Currently older people who need residential care have a choice of making a refundable up-front payment for their room or to pay rent to offset the loans providers take out to build facilities. Providers raise capital to build aged care facilities through equity or loan financing.
However, the taskforce did not consider the overall efficiency of the private capital market for financing aged care or alternative solutions.
Instead, it recommended capital contributions be streamlined and simplified by phasing out up-front payments and focusing on rental contributions. This echoes the royal commission, which found rent to be a more efficient and less risky method of financing capital for aged care in private capital markets.
It’s likely that in a decade or so, once the new home care arrangements are in place, there will be proportionally fewer older people in residential aged care. Those who do go are likely to be more disabled and have greater care needs. And those with more money will pay more for their accommodation and everyday living arrangements. But they may have more choice too.
Although the federal government has ruled out an aged care levy and changes to assets test on the family home, it has yet to respond to the majority of the recommendations. But given the aged care minister chaired the taskforce, it’s likely to provide a good indication of current thinking.
Hal Swerissen, Emeritus Professor, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Correct An Upper Spine Hump (Simple Stretch & Exercise)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Generally called a neck hump in this video, it can be in the cervical (neck) vertebrae or it can be in the thoracic (upper back) vertebrae. It’s also known as a dowager’s hump, buffalo hump, or kyphosis.
However, it can be fixed:
What to do
First understand the cause: it generally comes from poor posture, especially from prolonged desk work or phone use.
With that in mind…
- Posture adjustments: lean back in a chair to counter gravity’s pull on your head. Avoid slumping; keep your head aligned with your spine.
- Stretching: lie flat on the floor without pillows to restore spinal alignment. Gradually reduce pillow height during sleep to decrease neck hyperflexion.
- Neck retraction: pull chin straight back while keeping your eyes looking forwards. Hold for 15 seconds, gradually increasing to 60 seconds. Perform 10 repetitions, resting between sets.
- Strengthening: lean forward and pull the chin back against gravity. Hold, or repeat for 10 repetitions. Over time, increase duration to a minute.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Pains That Good Posture Now Can Help You Avoid Later
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Migraine Mythbusting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Migraine: When Headaches Are The Tip Of The Neurological Iceberg
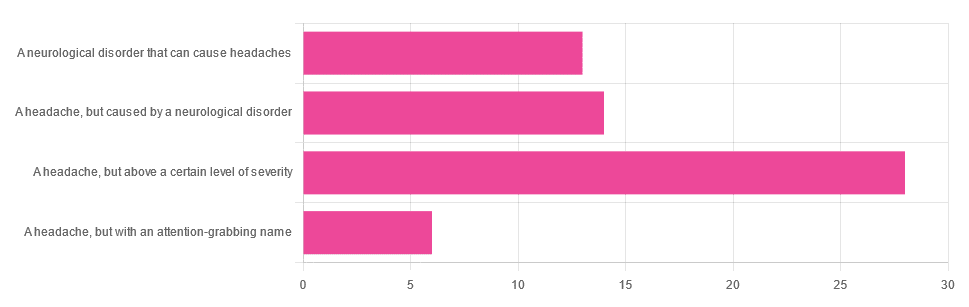
Yesterday, we asked you “What is a migraine?” and got the above-depicted, below-described spread of responses:
- Just under 46% said “a headache, but above a certain level of severity”
- Just under 23% said “a headache, but caused by a neurological disorder”
- Just over 21% said “a neurological disorder that can cause headaches”
- Just under 10% said “a headache, but with an attention-grabbing name”
So… What does the science say?
A migraine is a headache, but above a certain level of severity: True or False?
While that’s usually a very noticeable part of it… That’s only one part of it, and not a required diagnostic criterion. So, in terms of defining what a migraine is, False.
Indeed, migraine may occur without any headache, let alone a severe one, for example: Abdominal Migraine—though this is much less well-researched than the more common with-headache varieties.
Here are the defining characteristics of a migraine, with the handy mnemonic 5-4-3-2-1:
- 5 or more attacks
- 4 hours to 3 days in duration
- 2 or more of the following:
- Unilateral (affects only one side of the head)
- Pulsating
- Moderate or severe pain intensity
- Worsened by or causing avoidance of routine physical activity
- 1 or more of the following:
- Nausea and/or vomiting
- Sensitivity to both light and sound
Source: Cephalalgia | ICHD-II Classification: Parts 1–3: Primary, Secondary and Other
As one of our subscribers wrote:
❝I have chronic migraine, and it is NOT fun. It takes away from my enjoyment of family activities, time with friends, and even enjoying alone time. Anyone who says a migraine is just a bad headache has not had to deal with vertigo, nausea, loss of balance, photophobia, light sensitivity, or a host of other symptoms.❞
Migraine is a neurological disorder: True or False?
True! While the underlying causes aren’t known, what is known is that there are genetic and neurological factors at play.
❝Migraine is a recurrent, disabling neurological disorder. The World Health Organization ranks migraine as the most prevalent, disabling, long-term neurological condition when taking into account years lost due to disability.
Considerable progress has been made in elucidating the pathophysiological mechanisms of migraine, associated genetic factors that may influence susceptibility to the disease❞
Source: JHP | Mechanisms of migraine as a chronic evolutive condition
Migraine is just a headache with a more attention-grabbing name: True or False?
Clearly, False.
As we’ve already covered why above, we’ll just close today with a nod to an old joke amongst people with chronic illnesses in general:
“Are you just saying that because you want attention?”
“Yes… Medical attention!”
Want to learn more?
You can find a lot of resources at…
NIH | National Institute of Neurological Disorders & Stroke | Migraine
and…
The Migraine Trust ← helpfully, this one has a “Calm mode” to tone down the colorscheme of the website!
Particularly useful from the above site are its pages:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Apples vs Bananas – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apples to bananas, we picked the bananas.
Why?
Both apples and bananas contain lots of vitamins, but bananas contain far more of Vitamins A, B, and C.
Apples beat bananas only for vitamins E and K.
This may seem like “well that’s 2 vs 3; that’s pretty close” until one remembers that vitamin B is actually eight vitamins in a trenchcoat. Bananas have more of vitamins B1, B2, B3, B5, B6, and B9.
If you’re wondering about the other numbers: neither fruit contains vitamins B7 (biotin) or B12 (cobalamins of various kinds). Vitamins B4, B8, B10, and B11 do not exist as such (due to changes in how vitamins are classified).
Both apples and bananas contain lots of minerals, but bananas contain far more of iron, magnesium, phosphorus, potassium, zinc, copper, manganese, and selenium.
Apples beat bananas only for calcium (and then, only very marginally)
Both apples and bananas have plenty of fiber.
Apples have marginally less sugar, but given the fiber content, this is pretty much moot when it comes to health considerations, and apples are higher in fructose in any case.
In short, both are wonderful fruits (and we encourage you to enjoy both!), and/but bananas beat apples healthwise in almost all measures.
PS: top tip if you find it challenging to get bananas at the right level of ripeness for eating… Try sun-dried! Not those hard chip kinds (those are mechanically and/or chemically dried, and usually have added sugar and preservatives), but sun-dried.
Here’s an example product on Amazon
Warning: since there aren’t many sun-dried bananas available on Amazon, double-check you haven’t been redirected to mechanically/chemically dried ones, as Amazon will try that sometimes!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: