Menopause can bring increased cholesterol levels and other heart risks. Here’s why and what to do about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Menopause is a natural biological process that marks the end of a woman’s reproductive years, typically between 45 and 55. As women approach or experience menopause, common “change of life” concerns include hot flushes, sweats and mood swings, brain fog and fatigue.
But many women may not be aware of the long-term effects of menopause on the heart and blood vessels that make up the cardiovascular system. Heart disease accounts for 35% of deaths in women each year – more than all cancers combined.
What should women – and their doctors – know about these risks?
Hormones protect hearts – until they don’t
As early as 1976, the Framingham Heart Study reported more than twice the rates of cardiovascular events in postmenopausal than pre-menopausal women of the same age. Early menopause (younger than age 40) also increases heart risk.
Before menopause, women tend to be protected by their circulating hormones: oestrogen, to a lesser extent progesterone and low levels of testosterone.
These sex hormones help to relax and dilate blood vessels, reduce inflammation and improve lipid (cholesterol) levels. From the mid-40s, a decline in these hormone levels can contribute to unfavourable changes in cholesterol levels, blood pressure and weight gain – all risk factors for heart disease.

4 ways hormone changes impact heart risk
1. Dyslipidaemia– Menopause often involves atherogenic changes – an unhealthy imbalance of lipids in the blood, with higher levels of total cholesterol, triglycerides, and low-density lipoprotein (LDL-C), dubbed the “bad” cholesterol. There are also reduced levels of high-density lipoprotein (HDL-C) – the “good” cholesterol that helps remove LDL-C from blood. These changes are a major risk factor for heart attack or stroke.
2. Hypertension – Declines in oestrogen and progesterone levels during menopause contribute to narrowing of the large blood vessels on the heart’s surface, arterial stiffness and raise blood pressure.
3. Weight gain – Females are born with one to two million eggs, which develop in follicles. By the time they stop ovulating in midlife, fewer than 1,000 remain. This depletion progressively changes fat distribution and storage, from the hips to the waist and abdomen. Increased waist circumference (greater than 80–88 cm) has been reported to contribute to heart risk – though it is not the only factor to consider.
4. Comorbidities – Changes in body composition, sex hormone decline, increased food consumption, weight gain and sedentary lifestyles impair the body’s ability to effectively use insulin. This increases the risk of developing metabolic syndromes such as type 2 diabetes.
While risk factors apply to both genders, hypertension, smoking, obesity and type 2 diabetes confer a greater relative risk for heart disease in women.
So, what can women do?
Every woman has a different level of baseline cardiovascular and metabolic risk pre-menopause. This is based on their genetics and family history, diet, and lifestyle. But all women can reduce their post-menopause heart risk with:
- regular moderate intensity exercise such as brisk walking, pushing a lawn mower, riding a bike or water aerobics for 30 minutes, four or five times every week
- a healthy heart diet with smaller portion sizes (try using a smaller plate or bowl) and more low-calorie, nutrient-rich foods such as vegetables, fruit and whole grains
- plant sterols (unrefined vegetable oil spreads, nuts, seeds and grains) each day. A review of 14 clinical trials found plant sterols, at doses of at least 2 grams a day, produced an average reduction in serum LDL-C (bad cholesterol) of about 9–14%. This could reduce the risk of heart disease by 25% in two years
- less unhealthy (saturated or trans) fats and more low-fat protein sources (lean meat, poultry, fish – especially oily fish high in omega-3 fatty acids), legumes and low-fat dairy
- less high-calorie, high-sodium foods such as processed or fast foods
- a reduction or cessation of smoking (nicotine or cannabis) and alcohol
- weight-gain management or prevention.

What about hormone therapy medications?
Hormone therapy remains the most effective means of managing hot flushes and night sweats and is beneficial for slowing the loss of bone mineral density.
The decision to recommend oestrogen alone or a combination of oestrogen plus progesterone hormone therapy depends on whether a woman has had a hysterectomy or not. The choice also depends on whether the hormone therapy benefit outweighs the woman’s disease risks. Where symptoms are bothersome, hormone therapy has favourable or neutral effects on coronary heart disease risk and medication risks are low for healthy women younger than 60 or within ten years of menopause.
Depending on the level of stroke or heart risk and the response to lifestyle strategies, some women may also require medication management to control high blood pressure or elevated cholesterol levels. Up until the early 2000s, women were underrepresented in most outcome trials with lipid-lowering medicines.
The Cholesterol Treatment Trialists’ Collaboration analysed 27 clinical trials of statins (medications commonly prescribed to lower cholesterol) with a total of 174,000 participants, of whom 27% were women. Statins were about as effective in women and men who had similar risk of heart disease in preventing events such as stroke and heart attack.
Every woman approaching menopause should ask their GP for a 20-minute Heart Health Check to help better understand their risk of a heart attack or stroke and get tailored strategies to reduce it.
Treasure McGuire, Assistant Director of Pharmacy, Mater Health SEQ in conjoint appointment as Associate Professor of Pharmacology, Bond University and as Associate Professor (Clinical), The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Evidence doesn’t support spinal cord stimulators for chronic back pain – and they could cause harm
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In an episode of ABC’s Four Corners this week, the use of spinal cord stimulators for chronic back pain was brought into question.
Spinal cord stimulators are devices implanted surgically which deliver electric impulses directly to the spinal cord. They’ve been used to treat people with chronic pain since the 1960s.
Their design has changed significantly over time. Early models required an external generator and invasive surgery to implant them. Current devices are fully implantable, rechargeable and can deliver a variety of electrical signals.
However, despite their long history, rigorous experimental research to test the effectiveness of spinal cord stimulators has only been conducted this century. The findings don’t support their use for treating chronic pain. In fact, data points to a significant risk of harm.
What does the evidence say?
One of the first studies used to support the effectiveness of spinal cord stimulators was published in 2005. This study looked at patients who didn’t get relief from initial spinal surgery and compared implantation of a spinal cord stimulator to a repeat of the spinal surgery.
Although it found spinal cord stimulation was the more effective intervention for chronic back pain, the fact this study compared the device to something that had already failed once is an obvious limitation.
Later studies provided more useful evidence. They compared spinal cord stimulation to non-surgical treatments or placebo devices (for example, deactivated spinal cord stimulators).
A 2023 Cochrane review of the published comparative studies found nearly all studies were restricted to short-term outcomes (weeks). And while some studies appeared to show better pain relief with active spinal cord stimulation, the benefits were small, and the evidence was uncertain.
Only one high-quality study compared spinal cord stimulation to placebo up to six months, and it showed no benefit. The review concluded the data doesn’t support the use of spinal cord stimulation for people with back pain.
What about the harms?
The experimental studies often had small numbers of participants, making any estimate of the harms of spinal cord stimulation difficult. So we need to look to other sources.
A review of adverse events reported to Australia’s Therapeutic Goods Administration found the harms can be serious. Of the 520 events reported between 2012 and 2019, 79% were considered “severe” and 13% were “life threatening”.
We don’t know exactly how many spinal cord stimulators were implanted during this period, however this surgery is done reasonably widely in Australia, particularly in the private and workers compensation sectors. In 2023, health insurance data showed more than 1,300 spinal cord stimulator procedures were carried out around the country.
In the review, around half the reported harms were due to a malfunction of the device itself (for example, fracture of the electrical lead, or the lead moved to the wrong spot in the body). The other half involved declines in people’s health such as unexplained increased pain, infection, and tears in the lining around the spinal cord.
More than 80% of the harms required at least one surgery to correct the problem. The same study reported four out of every ten spinal cord stimulators implanted were being removed.
Chronic back pain can be debilitating. CGN089/Shutterstock High costs
The cost here is considerable, with the devices alone costing tens of thousands of dollars. Adding associated hospital and medical costs, the total cost for a single procedure averages more than $A50,000. With many patients undergoing multiple repeat procedures, it’s not unusual for costs to be measured in hundreds of thousands of dollars.
Rebates from Medicare, private health funds and other insurance schemes may go towards this total, along with out-of-pocket contributions.
Insurers are uncertain of the effectiveness of spinal cord stimulators, but because their implantation is listed on the Medicare Benefits Schedule and the devices are approved for reimbursement by the government, insurers are forced to fund their use.
Industry influence
If the evidence suggests no sustained benefit over placebo, the harms are significant and the cost is high, why are spinal cord stimulators being used so commonly in Australia? In New Zealand, for example, the devices are rarely used.
Doctors who implant spinal cord stimulators in Australia are well remunerated and funding arrangements are different in New Zealand. But the main reason behind the lack of use in New Zealand is because pain specialists there are not convinced of their effectiveness.
In Australia and elsewhere, the use of spinal cord stimulators is heavily promoted by the pain specialists who implant them, and the device manufacturers, often in unison. The tactics used by the spinal cord stimulator device industry to protect profits have been compared to tactics used by the tobacco industry.
A 2023 paper describes these tactics which include flooding the scientific literature with industry-funded research, undermining unfavourable independent research, and attacking the credibility of those who raise concerns about the devices.
It’s not all bad news
Many who suffer from chronic pain may feel disillusioned after watching the Four Corners report. But it’s not all bad news. Australia happens to be home to some of the world’s top back pain researchers who are working on safe, effective therapies.
New approaches such as sensorimotor retraining, which includes reassurance and encouragement to increase patients’ activity levels, cognitive functional therapy, which targets unhelpful pain-related thinking and behaviour, and old approaches such as exercise, have recently shown benefits in robust clinical research.
If we were to remove funding for expensive, harmful and ineffective treatments, more funding could be directed towards effective ones.
Ian Harris, Professor of Orthopaedic Surgery, UNSW Sydney; Adrian C Traeger, Research Fellow, Institute for Musculoskeletal Health, University of Sydney, and Caitlin Jones, Postdoctoral Research Associate in Musculoskeletal Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
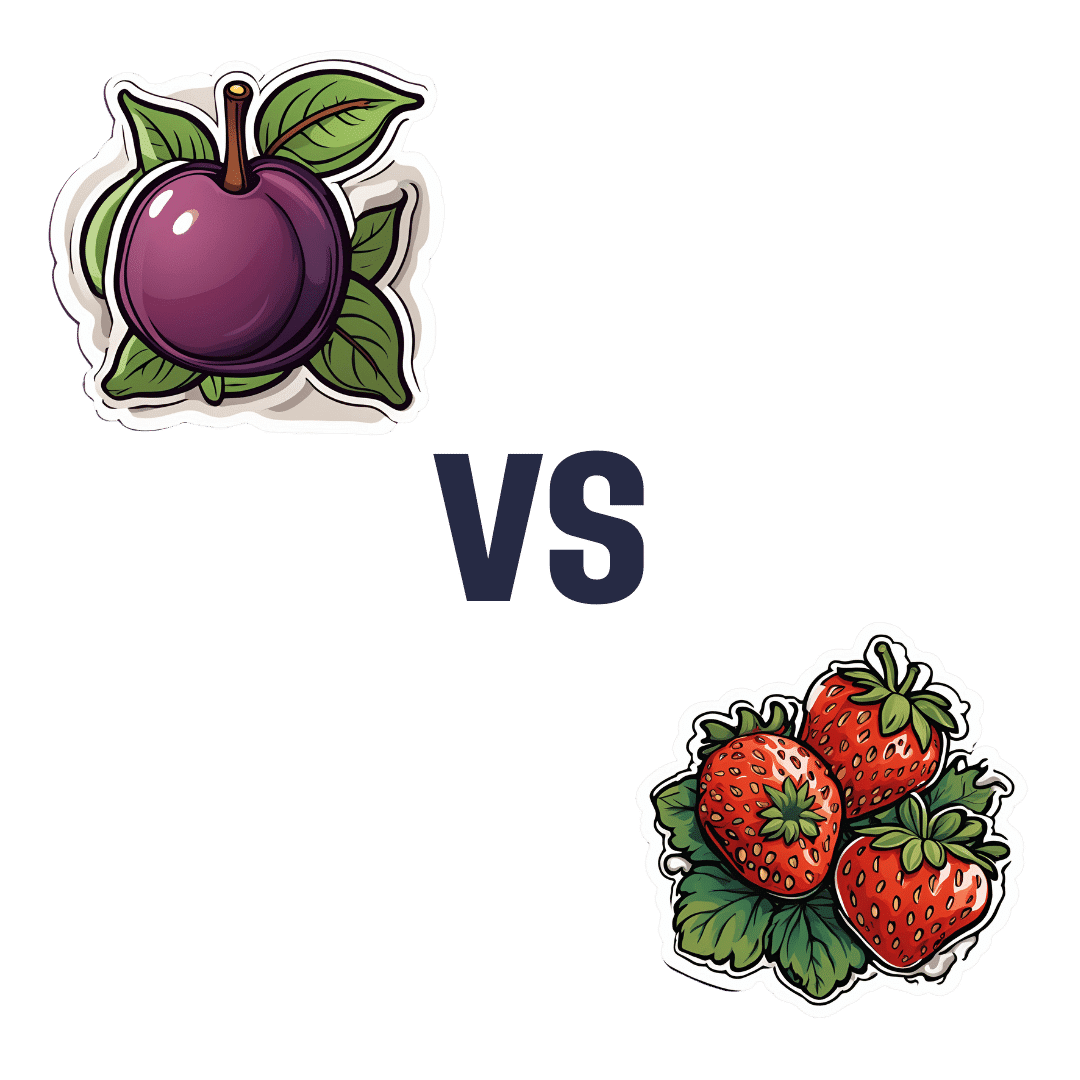
Plums vs Strawberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing plums to strawberries, we picked the strawberries.
Why?
Both are great! Absolutely top-tier fruits. However, even within the top tier, there are distinctions:
In terms of of macros, plums have more carbs while strawberries have more fiber; we’ll take the extra fiber for the win here.
In the category of vitamins, plums have more of vitamins A, B1, B2, and K, while strawberries have more of vitamins B6, B9, C, E, and choline, thus scoring a marginal win for strawberries in this round.
When it comes to minerals, plums have (slightly) more copper, while strawberries have more calcium, iron, magnesium, manganese, phosphorus, selenium, and zinc. One more win for strawberries.
In terms of phytochemicals, plums have a higher total mass of polyphenols, and so win this round, although strawberries scored well too.
Adding up the sections makes for an overall win for strawberries, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Top 8 Fruits That Prevent & Kill Cancer
Enjoy!
Share This Post
-
How To Ease Neck Pain At Home
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Bang is offering exercises to alleviate neck pain, which pain can be a real… Well, if only there were a good phrase for expressing how troublesome pain in that part of the body can be.
To be clear, he’s a doctor of chiropractic, not a medical doctor, but his advice has clearly been helping people alleviate pain, so without further ado, he advises the following things:
- Taking the head and neck slowly and carefully through the full range of motion available
- Contracting the neck muscles while repeating the above exercise, three times each way
- Backing off a little if it hurts at any point, but noting where the limits lie
- Repeating again the range of motion exercise, this time adding gentle resistance
- Holding each end of this for twenty seconds before releasing and doing the other side, three times each way
- Finally, stabilizing the head centrally and pushing into one’s hands, as an isometric strengthening exercise
He demonstrates each part clearly in this short (5:58) video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to know more about chiropractic?
You might like our previous main feature:
Is Chiropractic All It’s Cracked Up To Be?
Take care!
Share This Post
Related Posts
-
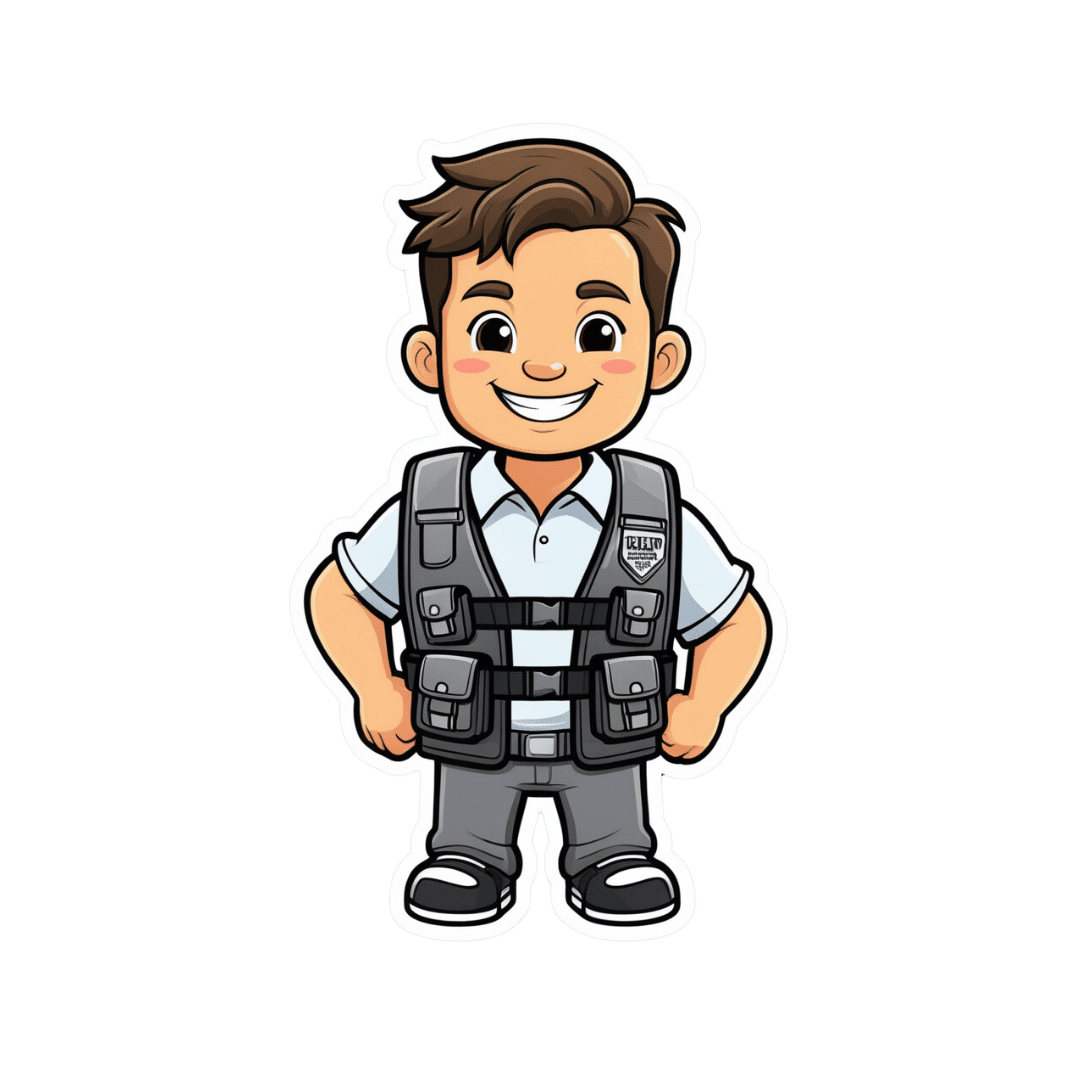
Should I get a weighted vest to boost my fitness? And how heavy should it be?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Exercise training while wearing a weighted vest is undergoing somewhat of a renaissance. Social media posts and trainers are promoting them as a potential strategy for improving fitness and health.
Exercising with additional weight attached to the body is nothing new. This idea has been used with soldiers for many centuries if not millennia – think long hikes with a heavy pack.
The modern weighted vest comes in a range of designs that are more comfortable and can be adjusted in terms of the weight added. But could one be helpful for you?
ZR10/Shutterstock What the research says
One of the earliest research studies, reported in 1993, followed 36 older people wearing weighted vests during a weekly exercise class and at home over a 20-week period. Wear was associated with improvements in bone health, pain and physical function.
Since then, dozens of papers have evaluated the exercise effects of wearing a weighted vest, reporting a range of benefits.
Not surprisingly, exercise with a weighted vest increases physiological stress – or how hard the body has to work – as shown by increased oxygen uptake, heart rate, carbohydrate utilisation and energy expenditure.
Adding weight equal to 10% of body weight is effective. But it doesn’t appear the body works significantly harder when wearing 5% extra weight compared to body weight alone.
Does more load mean greater injury risk?
A small 2021 study suggested additional weights don’t alter the biomechanics of walking or running. These are important considerations for lower-limb injury risk.
The safety considerations of exercising with weighted vests have also been reported in a biomechanical study of treadmill running with added weight of 1% to 10% of body weight.
While physiological demand (indicated by heart rate) was higher with additional weight and the muscular forces greater, running motion was not negatively affected.
To date no research studies have reported increased injuries due to wearing weighted vests for recreational exercise. However a 2018 clinical study on weight loss in people with obesity found back pain in 25% of those wearing such vests. Whether this can be translated to recreational use in people who don’t have obesity is difficult to say. As always, if pain or discomfort is experienced then you should reduce the weight or stop vest training.
Better for weight loss or bone health?
While wearing a weighted vest increases the energy expenditure of aerobic and resistance exercise, research to show it leads to greater fat loss or retaining muscle mass is somewhat inconclusive.
One older study investigated treadmill walking for 30 minutes, three times a week in postmenopausal women with osteoporosis. The researchers found greater fat loss and muscle gain in the participants who wore a weighted vest (at 4–8% body weight). But subsequent research in obese older adults could not show greater fat loss in participants who wore weighted vests for an average of 6.7 hours per day.
There has been considerable interest in the use of weighted vests to improve bone health in older people. One 2003 study reported significant improvements in bone density in a group of older women over 32 weeks of weighted vest walking and strength training compared to a sedentary control group.
But a 2012 study found no difference in bone metabolism between groups of postmenopausal women with osteoporosis walking on a treadmill with or without a weighted vest.
Making progress
As with any exercise, there is a risk of injury if it is not done correctly. But the risk of weighted vest training appears low and can be managed with appropriate exercise progression and technique.
If you are new to training, then the priority should be to simply start exercising and not complicate it with wearing a weighted vest. The use of body weight alone will be sufficient to get you on the path to considerable gains in fitness.
Once you have a good foundation of strength, aerobic fitness and resilience for muscles, joints and bones, using a weighted vest could provide greater loading intensity as well as variation.
It is important to start with a lighter weight (such as 5% bodyweight) and build to no more than 10% body weight for ground impact exercises such as running, jogging or walking.
For resistance training such as squats, push-ups or chin-ups, progression can be achieved by increasing loads and adjusting the number of repetitions for each set to around 10 to 15. So, heavier loads but fewer repetitions, then building up to increase the load over time.
While weighted vests can be used for resistance training, it is probably easier and more convenient to use barbells, dumbbells, kettle bells or weighted bags.
The benefits of added weight can also be achieved by adding repetition or duration. Geert Pieters/Unsplash The bottom line
Weighted vest training is just one tool in an absolute plethora of equipment, techniques and systems. Yes, walking or jogging with around 10% extra body weight increases energy expenditure and intensity. But training for a little bit longer or at a higher intensity can achieve similar results.
There may be benefits for bone health in wearing a weighted vest during ground-based exercise such as walking or jogging. But similar or greater stimulus to bone growth can be achieved by resistance training or even the introduction of impact training such as hopping, skipping or bounding.
Exercising with a weighted vest likely won’t increase your injury risk. But it must be approached intelligently considering fitness level, existing and previous injuries, and appropriate progression for intensity and repetition.
Rob Newton, Professor of Exercise Medicine, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Broccoli vs Cauliflower – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing broccoli to cauliflower, we picked the broccoli.
Why?
This one is quite straightforward. Superficially, they’re very similar:
Both are great cruciferous vegetables with many health benefits to offer. Even for those keen to avoid oxalates, which cruciferous vegetables in general can be high in, these ones are quite low.
However, if you have IBS, you might want to avoid both, for their raffinose content that may cause problems for you.
For pretty much everyone else, unless you have a special reason why it’s not the case for you, both are a good source of abundant vitamins and minerals, and yet…
Anything cauliflower can do, broccoli can do better!
Broccoli contains more of the vitamins they both contain, and more of the minerals they both contain.
Broccoli also beats cauliflower on amino acids (except lysine), and contains a lot more lutein and zeaxanthin, carotenoids important for healthy eyes and brain.
So by all means enjoy both, but if you’re going to pick one, pick broccoli!
Want to know more?
Check out: Brain Food? The Eyes Have It!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
No-Exercise Exercise!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you love to go to the gym?
If so, today’s article might not be for you so much. Or maybe it will, because let’s face it, exercise is fun!
At least… It can be, and should be 😎
So without further ado, here’s a slew of no-exercise exercise ideas; we’re willing to bet that somewhere in the list there’s at least some you haven’t tried before, and probably some you haven’t done in a while but might enjoy making a reprise!
Walking
No surprises here: walking is great. Hopefully you have some green spaces near you, but if you don’t, [almost] any walking is better than no walking. So unless there’s some sort of environmental disaster going on outside, lace up and get stepping.
If you struggle to “walk for walking’s sake” give yourself a little mission. Walk to the shop to buy one item. Walk to the park and find a flower to photograph. Walk to the library and take out a book. Whatever works for you!
See also: The Doctor Who Wants Us To Exercise Less, And Move More
Take the stairs
This one doesn’t need many words, just: make it a habit.
Treat the elevators as though they aren’t there!
See also: How To Really Pick Up (And Keep!) Those Habits
Dance
Dance is amazing! Any kind of dance, whatever suits your tastes. This writer loves salsa and tango, but no matter whether for you it’s zouk or zumba, breakdancing or line dancing, whatever gets you moving is going to be great for you.
If you don’t know how, online tutorials abound, and best of all is to attend local classes if you can, because they’re always a fun social experience too.
Make music
Not something often thought of as an exercise, but it is! Most instruments require that we be standing or siting with good posture, focusing intently on our movements, and often as not, breathing very mindfully too. And yes, it’s great for the brain as well!
Check out: This Is Your Brain on Music: The Science of a Human Obsession – by Dr. Daniel Levitin
Take a stand
If you spend a lot of time at a desk, please consider investing in a standing desk; they can be truly life-changing. Not only is it so much better for your back, hips, neck, and internal organs, but also it burns hundreds more calories than sitting, due to the no-exercise exercise that is keeping your body constantly stabilized while on your feet.
(or, if you’re like this writer: on your foot. I do have two feet, I just spend an inordinate amount of time at my desk standing on one leg at a time; I’m a bit of a flamingo like that)
See also: Deskbound: Standing Up to a Sitting World – by Kelly Starrett and Glen Cordoza
Sit, but…
Sit in a sitting squat! Sometimes called a Slav squat, or an Asian squat, or a resting squat, or various other names:
Click Here If The Embedded Video Doesn’t Load Automatically!
Alternatively, sitting in seiza (the traditional Japanese sitting position) is also excellent, but watch out! While it’s great once your body is accustomed to it, if you haven’t previously sat this way much, you may cut off your own circulation, hurt your knees, and (temporarily) lose feeling in your feet. So if you don’t already sit in seiza often, gradually work up the time period you spend sitting in seiza, so that your vasculature can adapt and improve, which honestly, is a very good thing for your legs and feet to have.
Breathe
Perhaps the absolute most “no-exercise exercise” there is. And yes, of course you are (hopefully) breathing all the time, but how you are breathing matters a lot:
The Inside Job Of Fixing Our Breathing: Exercises That Can Fix Sinus Problems (And More)
Clean
This doesn’t have to mean scrubbing floors like a sailor—even merely giving your house the Marie Kondo treatment counts, because while you’re distracted with all the objects, you’re going to be going back and forth, getting up and down, etc, clocking up lots of exercise that you barely even notice!
PS, check out: The Life-Changing Manga Of Tidying Up – by Marie Kondo
Garden
As with the above, it’s lots of activity that doesn’t necessarily feel like it (assuming you’re doing more pruning and weeding etc, and less digging ditches etc), and as a bonus, there are a stack of mental health benefits to being in a green natural environment and interacting with soil:
Read more: The Antidepressant In Your Garden
Climb
Depending on where you live, this might mean an indoor climbing wall, but give it a go! They have color-coded climbs from beginner to advanced, so don’t worry about being out of your depth.
And the best thing is, the beginner climbs will be as much a workout to a beginner as the advanced climbs will be to an advanced climber, because at the end of the day, you’re still clinging on for dear life, no matter whether it’s a sizeable handhold not far from the ground, or the impression of a fingernail crack in an overhang 100ft in the air.
Video games (but…)
Less in the category of Stardew Valley, and more in the category of Wii Fit.
So, dust off that old controller (or treat yourself to one if you didn’t have one already), and get doing a hundred sports and other physical activities in the comfort of your living room, with a surprisingly addictive gaming system!
Sex!
You probably don’t need instructions here, and if you do, well honestly, we’re running out of space today. But the answer to “does xyz count?” is “did it get your heart racing?” because if so, it counts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: