Bird Flu Is Bad for Poultry and Dairy Cows. It’s Not a Dire Threat for Most of Us — Yet.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Headlines are flying after the Department of Agriculture confirmed that the H5N1 bird flu virus has infected dairy cows around the country. Tests have detected the virus among cattle in nine states, mainly in Texas and New Mexico, and most recently in Colorado, said Nirav Shah, principal deputy director at the Centers for Disease Control and Prevention, at a May 1 event held by the Council on Foreign Relations.
A menagerie of other animals have been infected by H5N1, and at least one person in Texas. But what scientists fear most is if the virus were to spread efficiently from person to person. That hasn’t happened and might not. Shah said the CDC considers the H5N1 outbreak “a low risk to the general public at this time.”
Viruses evolve and outbreaks can shift quickly. “As with any major outbreak, this is moving at the speed of a bullet train,” Shah said. “What we’ll be talking about is a snapshot of that fast-moving train.” What he means is that what’s known about the H5N1 bird flu today will undoubtedly change.
With that in mind, KFF Health News explains what you need to know now.
Q: Who gets the bird flu?
Mainly birds. Over the past few years, however, the H5N1 bird flu virus has increasingly jumped from birds into mammals around the world. The growing list of more than 50 species includes seals, goats, skunks, cats, and wild bush dogs at a zoo in the United Kingdom. At least 24,000 sea lions died in outbreaks of H5N1 bird flu in South America last year.
What makes the current outbreak in cattle unusual is that it’s spreading rapidly from cow to cow, whereas the other cases — except for the sea lion infections — appear limited. Researchers know this because genetic sequences of the H5N1 viruses drawn from cattle this year were nearly identical to one another.
The cattle outbreak is also concerning because the country has been caught off guard. Researchers examining the virus’s genomes suggest it originally spilled over from birds into cows late last year in Texas, and has since spread among many more cows than have been tested. “Our analyses show this has been circulating in cows for four months or so, under our noses,” said Michael Worobey, an evolutionary biologist at the University of Arizona in Tucson.
Q: Is this the start of the next pandemic?
Not yet. But it’s a thought worth considering because a bird flu pandemic would be a nightmare. More than half of people infected by older strains of H5N1 bird flu viruses from 2003 to 2016 died. Even if death rates turn out to be less severe for the H5N1 strain currently circulating in cattle, repercussions could involve loads of sick people and hospitals too overwhelmed to handle other medical emergencies.
Although at least one person has been infected with H5N1 this year, the virus can’t lead to a pandemic in its current state. To achieve that horrible status, a pathogen needs to sicken many people on multiple continents. And to do that, the H5N1 virus would need to infect a ton of people. That won’t happen through occasional spillovers of the virus from farm animals into people. Rather, the virus must acquire mutations for it to spread from person to person, like the seasonal flu, as a respiratory infection transmitted largely through the air as people cough, sneeze, and breathe. As we learned in the depths of covid-19, airborne viruses are hard to stop.
That hasn’t happened yet. However, H5N1 viruses now have plenty of chances to evolve as they replicate within thousands of cows. Like all viruses, they mutate as they replicate, and mutations that improve the virus’s survival are passed to the next generation. And because cows are mammals, the viruses could be getting better at thriving within cells that are closer to ours than birds’.
The evolution of a pandemic-ready bird flu virus could be aided by a sort of superpower possessed by many viruses. Namely, they sometimes swap their genes with other strains in a process called reassortment. In a study published in 2009, Worobey and other researchers traced the origin of the H1N1 “swine flu” pandemic to events in which different viruses causing the swine flu, bird flu, and human flu mixed and matched their genes within pigs that they were simultaneously infecting. Pigs need not be involved this time around, Worobey warned.
Q: Will a pandemic start if a person drinks virus-contaminated milk?
Not yet. Cow’s milk, as well as powdered milk and infant formula, sold in stores is considered safe because the law requires all milk sold commercially to be pasteurized. That process of heating milk at high temperatures kills bacteria, viruses, and other teeny organisms. Tests have identified fragments of H5N1 viruses in milk from grocery stores but confirm that the virus bits are dead and, therefore, harmless.
Unpasteurized “raw” milk, however, has been shown to contain living H5N1 viruses, which is why the FDA and other health authorities strongly advise people not to drink it. Doing so could cause a person to become seriously ill or worse. But even then, a pandemic is unlikely to be sparked because the virus — in its current form — does not spread efficiently from person to person, as the seasonal flu does.
Q: What should be done?
A lot! Because of a lack of surveillance, the U.S. Department of Agriculture and other agencies have allowed the H5N1 bird flu to spread under the radar in cattle. To get a handle on the situation, the USDA recently ordered all lactating dairy cattle to be tested before farmers move them to other states, and the outcomes of the tests to be reported.
But just as restricting covid tests to international travelers in early 2020 allowed the coronavirus to spread undetected, testing only cows that move across state lines would miss plenty of cases.
Such limited testing won’t reveal how the virus is spreading among cattle — information desperately needed so farmers can stop it. A leading hypothesis is that viruses are being transferred from one cow to the next through the machines used to milk them.
To boost testing, Fred Gingrich, executive director of a nonprofit organization for farm veterinarians, the American Association of Bovine Practitioners, said the government should offer funds to cattle farmers who report cases so that they have an incentive to test. Barring that, he said, reporting just adds reputational damage atop financial loss.
“These outbreaks have a significant economic impact,” Gingrich said. “Farmers lose about 20% of their milk production in an outbreak because animals quit eating, produce less milk, and some of that milk is abnormal and then can’t be sold.”
The government has made the H5N1 tests free for farmers, Gingrich added, but they haven’t budgeted money for veterinarians who must sample the cows, transport samples, and file paperwork. “Tests are the least expensive part,” he said.
If testing on farms remains elusive, evolutionary virologists can still learn a lot by analyzing genomic sequences from H5N1 viruses sampled from cattle. The differences between sequences tell a story about where and when the current outbreak began, the path it travels, and whether the viruses are acquiring mutations that pose a threat to people. Yet this vital research has been hampered by the USDA’s slow and incomplete posting of genetic data, Worobey said.
The government should also help poultry farmers prevent H5N1 outbreaks since those kill many birds and pose a constant threat of spillover, said Maurice Pitesky, an avian disease specialist at the University of California-Davis.
Waterfowl like ducks and geese are the usual sources of outbreaks on poultry farms, and researchers can detect their proximity using remote sensing and other technologies. By zeroing in on zones of potential spillover, farmers can target their attention. That can mean routine surveillance to detect early signs of infections in poultry, using water cannons to shoo away migrating flocks, relocating farm animals, or temporarily ushering them into barns. “We should be spending on prevention,” Pitesky said.
Q: OK it’s not a pandemic, but what could happen to people who get this year’s H5N1 bird flu?
No one really knows. Only one person in Texas has been diagnosed with the disease this year, in April. This person worked closely with dairy cows, and had a mild case with an eye infection. The CDC found out about them because of its surveillance process. Clinics are supposed to alert state health departments when they diagnose farmworkers with the flu, using tests that detect influenza viruses, broadly. State health departments then confirm the test, and if it’s positive, they send a person’s sample to a CDC laboratory, where it is checked for the H5N1 virus, specifically. “Thus far we have received 23,” Shah said. “All but one of those was negative.”
State health department officials are also monitoring around 150 people, he said, who have spent time around cattle. They’re checking in with these farmworkers via phone calls, text messages, or in-person visits to see if they develop symptoms. And if that happens, they’ll be tested.
Another way to assess farmworkers would be to check their blood for antibodies against the H5N1 bird flu virus; a positive result would indicate they might have been unknowingly infected. But Shah said health officials are not yet doing this work.
“The fact that we’re four months in and haven’t done this isn’t a good sign,” Worobey said. “I’m not super worried about a pandemic at the moment, but we should start acting like we don’t want it to happen.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Coconut vs Avocado – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing coconut to avocado, we picked the avocado.
Why?
In terms of macros, avocado is lower in carbs and also in net carbs—coconut’s a little higher in fiber, but not enough to make up for the difference in carbs nor, when it comes to glycemic index and insulin index, the impact of coconut’s much higher fat content on insulin responses too. On which note, while coconut’s fats are broadly considered healthy (its impressive saturated fat content is formed of medium-chain triglycerides which, in moderation, are heart-healthy), avocado’s fats are even healthier, being mostly monounsaturated fat with some polyunsaturated (and about 15x less saturated fat). All in all, a fair win for avocado on the macros front, but coconut isn’t bad in moderation.
When it comes to vitamins, avocados are higher in vitamins A, B1, B2, B3, B5, B6, B9, C, E, K, and choline. Most of those differences are by very large margins. Coconuts are not higher in any vitamins. A huge, easy, “perfect score” win for avocados.
In the category of minerals, however, it’s coconut’s turn to sweep with more calcium, copper, iron, magnesium, manganese, phosphorus, zinc, and selenium—though the margins are mostly not nearly as impressive as avocado’s vitamin margins. Speaking of avocados, they do have more potassium than coconuts do, but the margin isn’t very large. A compelling win for coconut’s mineral content.
Adding up the sections, we get to a very credible win for avocados, but coconuts are also very respectable. So, as ever, enjoy both (although we do recommend exercising moderation in the case of coconuts, mainly because of the saturated fat content), and if you’re choosing between them for some purpose, then avocado will generally be the best option.
Want to learn more?
You might like to read:
- Can Saturated Fats Be Healthy? ← defying Betteridge’s Law here!
- Avocado, Coconut & Lime Crumble Pots ← if you do want to enjoy both, here’s a fabulous way to do so in style
Take care!
Share This Post
-
Dodging Dengue In The US
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dengue On The Rise
We wrote recently about dengue outbreaks in the Americas, with Puerto Rico declaring an epidemic. Cases are now being reported in Florida too, and are likely to spread, so it’s good to be prepared, if your climate is of the “warm and humid” kind.
If you want to catch up on the news first, here you go:
- UN health agency cites tenfold increase in reported cases of dengue over the last generation
- Puerto Rico has declared an epidemic following a spike in dengue cases
- Dengue fever confirmed in Florida Keys as US on watch for rise in mosquito illness
Note: dengue is far from unheard of in Florida, but the rising average temperatures in each year mean that each year stands a good chance of seeing more cases than the previous. It’s been climbing since at least 2017, took a dip during the time of COVID restrictions keeping people at home more, and then for the more recent years has been climbing again since.
What actually is it?
Dengue is a viral, mosquito-borne disease, characterized by fever, vomiting, muscle pain, and a rash, in about 1 in 4 cases.
Which can sound like “you’ll know if you have it”, but in fact it’s usually asymptomatic for a week or more after infection, so, watch out!
What next, if those symptoms appear?
The good news is: the fever will usually last less than a week
The bad news is: a day or so after that the fever subsided, the more serious symptoms are likely to start—if they’re going to.
If you’re unlucky enough to be one of the 1 in 20 who get the serious symptoms, then you can expect abdominal cramps, repeat vomiting, bleeding from various orifices (you may not get them all, but all are possible), and (hardly surprising, given the previous items) “extreme fatigue and restlessness”.
If you get those symptoms, then definitely get to an ER as soon as possible, as dengue can become life-threatening within hours of such.
Read more: CDC | Symptoms of Dengue and Testing
While there is not a treatment for dengue per se, the Emergency Room will be better able to manage your symptoms and thus keep you alive long enough for them to pass.
If you’d like much more detail (on symptoms, seriousness, at-risk demographics, and prognosis) than what the CDC offers, then…
Read more: BMJ | Dengue Fever
Ok, so how do we dodge the dengue?
It sounds flippant to say “don’t get bitten”, but that’s it. However, there are tips are not getting bitten:
- Use mosquito-repellent, but it has to contain >20% DEET, so check labels
- Use mosquito nets where possible (doors, windows, etc, and the classic bed-tent net is not a bad idea either)
- Wear clothing that covers your skin, especially during the day—it can be light clothing; it doesn’t need to be a HazMat suit! But it does need to reduce the area of attack to reduce the risk of bites.
- Limit standing water around your home—anything that can hold even a small amount of standing water is a potential mosquito-breeding ground. Yes, even if it’s a crack in your driveway or a potted bromeliad.
Further reading
You might also like to check out:
Stickers and wristbands aren’t a reliable way to prevent mosquito bites. Here’s why
…and in case dengue wasn’t bad enough:
Mosquitoes can spread the flesh-eating Buruli ulcer. Here’s how you can protect yourself
Take care!
Share This Post
-
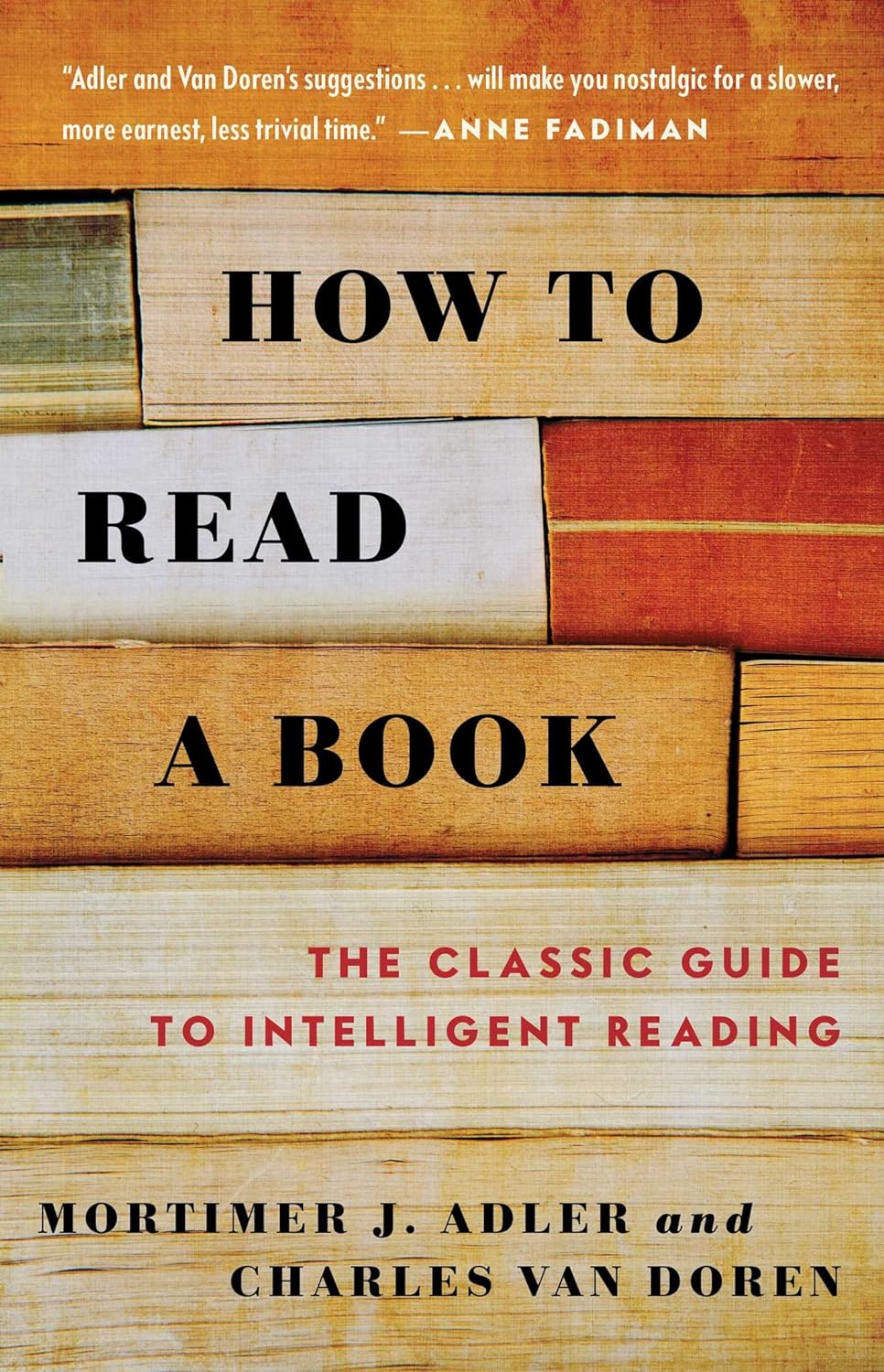
How to Read a Book – by Mortimer J. Adler and Charles Van Doren
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are you a cover-to-cover person, or a dip-in-and-out person?
Mortimer Adler and Charles van Doren have made a science out of getting the most from reading books.
They help you find what you’re looking for (Maybe you want to find a better understanding of PCOS… maybe you want to find the definition of “heuristics”… maybe you want to find a new business strategy… maybe you want to find a romantic escape… maybe you want to find a deeper appreciation of 19th century poetry, maybe you want to find… etc).
They then help you retain what you read, and make sure that you don’t miss a trick.
Whether you read books so often that optimizing this is of huge value for you, or so rarely that when you do, you want to make it count, this book could make a real difference to your reading experience forever after.
Share This Post
Related Posts
-
Pajama Pilates – by Maria Mankin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If The Science Of Pilates was a bit more information than you wanted to get up and running with Pilates at home, then this book offers a much easier way in.
As the name suggests, it’s all about convenience, and making things as easy as possible while enjoying the gradual cumulative gains that come when one practises even just a little every day instead of thinking “well I would, but I have to read all this technical stuff and get changed and clear a space and…”, and thus results in meaningful improvements to mobility and strength over time.
The 40 exercises promised by the subtitle are demonstrate via cute illustrations, of which the cover art is a good representative example. There’s nothing unduly technical here, and yet everything is quite clear. There are also simple practical explanations for each, as well as an initial overview of Pilates as a whole, its principles and necessary knowledge and so forth.
Bottom line: if you’d like to get into Pilates but it has seemed sufficiently taxing that you’ve never quite got started, or if you did then it didn’t stick, then this book can make things easier.
Click here to check out Pajama Pilates, and get ready to pajama Pilates party!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Secret to Mental Health – by George Pransky
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book (and its author) have a sizeable popular following, so it definitely can be said that it has been well-received by many people. The premise in this book is that there is fundamentally nothing wrong with anybody’s brain, and rather everything can be broken down into:
- Mind (the energy and intelligence that animates all life)
- Consciousness (the capacity to be aware of one’s life and experiences)
- Thought (the ability to think, allowing individuals to create their personal experience of reality)
The author explains, over the course of 145 pages, that where anyone with any perceived mental health issue is going wrong is by either lacking self-awareness (Consciousness) or erring by creating an undesirable personal experience of reality (Thought).
In terms of the science of this, frequent references are made to “there is evidence that shows”, “new discoveries about mental health suggest…”, etc, but this claimed evidence is never actually presented, just alluded to. Where many books would have a bibliography, this one has simply a collection of what the author has titled “interesting case studies, conversations, papers, and discussions” (there are no actual case studies or papers; it is just a collection of anecdotes).
The style is… Honestly, in this reviewer’s opinion, barely readable. But, apparently lots of people love it, so your mileage may vary.
We don’t usually delve too far into claimed credentials, but because of the interesting writing style and the bold claims without evidence, we were curious as to where this PhD came from, and apparently it came from a now-shut-down diploma mill that was described by the court as “a complete scam”.
Bottom line: we can’t recommend this one, but we read it so that you don’t have to, and we hope that publishing this review will help reassure you that when we do recommend a book, we mean it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A person in Texas caught bird flu after mixing with dairy cattle. Should we be worried?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The United States’ Centers for Disease Control and Prevention (CDC) has issued a health alert after the first case of H5N1 avian influenza, or bird flu, seemingly spread from a cow to a human.
A farm worker in Texas contracted the virus amid an outbreak in dairy cattle. This is the second human case in the US; a poultry worker tested positive in Colorado in 2022.
The virus strain identified in the Texan farm worker is not readily transmissible between humans and therefore not a pandemic threat. But it’s a significant development nonetheless.
Some background on bird flu
There are two types of avian influenza: highly pathogenic or low pathogenic, based on the level of disease the strain causes in birds. H5N1 is a highly pathogenic avian influenza.
H5N1 first emerged in 1997 in Hong Kong and then China in 2003, spreading through wild bird migration and poultry trading. It has caused periodic epidemics in poultry farms, with occasional human cases.
Influenza A viruses such as H5N1 are further divided into variants, called clades. The unique variant causing the current epidemic is H5N1 clade 2.3.4.4b, which emerged in late 2020 and is now widespread globally, especially in the Americas.
In the past, outbreaks could be controlled by culling of infected birds, and H5N1 would die down for a while. But this has become increasingly difficult due to escalating outbreaks since 2021.
Wild animals are now in the mix
Waterfowl (ducks, swans and geese) are the main global spreaders of avian flu, as they migrate across the world via specific routes that bypass Australia. The main hub for waterfowl to migrate around the world is Quinghai lake in China.
But there’s been an increasing number of infected non-waterfowl birds, such as true thrushes and raptors, which use different flyways. Worryingly, the infection has spread to Antarctica too, which means Australia is now at risk from different bird species which fly here.
H5N1 has escalated in an unprecedented fashion since 2021, and an increasing number of mammals including sea lions, goats, red foxes, coyotes, even domestic dogs and cats have become infected around the world.
Wild animals like red foxes which live in peri-urban areas are a possible new route of spread to farms, domestic pets and humans.
Dairy cows and goats have now become infected with H5N1 in at least 17 farms across seven US states.
What are the symptoms?
Globally, there have been 14 cases of H5N1 clade 2.3.4.4b virus in humans, and 889 H5N1 human cases overall since 2003.
Previous human cases have presented with a severe respiratory illness, but H5N1 2.3.4.4b is causing illness affecting other organs too, like the brain, eyes and liver.
For example, more recent cases have developed neurological complications including seizures, organ failure and stroke. It’s been estimated that around half of people infected with H5N1 will die.
The case in the Texan farm worker appears to be mild. This person presented with conjunctivitis, which is unusual.
Food safety
Contact with sick poultry is a key risk factor for human infection. Likewise, the farm worker in Texas was likely in close contact with the infected cattle.
The CDC advises pasteurised milk and well cooked eggs are safe. However, handling of infected meat or eggs in the process of cooking, or drinking unpasteurised milk, may pose a risk.
Although there’s no H5N1 in Australian poultry or cattle, hygienic food practices are always a good idea, as raw milk or poorly cooked meat, eggs or poultry can be contaminated with microbes such as salmonella and E Coli.
If it’s not a pandemic, why are we worried?
Scientists have feared avian influenza may cause a pandemic since about 2005. Avian flu viruses don’t easily spread in humans. But if an avian virus mutates to spread in humans, it can cause a pandemic.
One concern is if birds were to infect an animal like a pig, this acts as a genetic mixing vessel. In areas where humans and livestock exist in close proximity, for example farms, markets or even in homes with backyard poultry, the probability of bird and human flu strains mixing and mutating to cause a new pandemic strain is higher.
There are a number of potential pathways to a pandemic caused by influenza. Author provided The cows infected in Texas were tested because farmers noticed they were producing less milk. If beef cattle are similarly affected, it may not be as easily identified, and the economic loss to farmers may be a disincentive to test or report infections.
How can we prevent a pandemic?
For now there is no spread of H5N1 between humans, so there’s no immediate risk of a pandemic.
However, we now have unprecedented and persistent infection with H5N1 clade 2.3.4.4b in farms, wild animals and a wider range of wild birds than ever before, creating more chances for H5N1 to mutate and cause a pandemic.
Unlike the previous epidemiology of avian flu, where hot spots were in Asia, the new hot spots (and likely sites of emergence of a pandemic) are in the Americas, Europe or in Africa.
Pandemics grow exponentially, so early warnings for animal and human outbreaks are crucial. We can monitor infections using surveillance tools such as our EPIWATCH platform.
The earlier epidemics can be detected, the better the chance of stamping them out and rapidly developing vaccines.
Although there is a vaccine for birds, it has been largely avoided until recently because it’s only partially effective and can mask outbreaks. But it’s no longer feasible to control an outbreak by culling infected birds, so some countries like France began vaccinating poultry in 2023.
For humans, seasonal flu vaccines may provide a small amount of cross-protection, but for the best protection, vaccines need to be matched exactly to the pandemic strain, and this takes time. The 2009 flu pandemic started in May in Australia, but the vaccines were available in September, after the pandemic peak.
To reduce the risk of a pandemic, we must identify how H5N1 is spreading to so many mammalian species, what new wild bird pathways pose a risk, and monitor for early signs of outbreaks and illness in animals, birds and humans. Economic compensation for farmers is also crucial to ensure we detect all outbreaks and avoid compromising the food supply.
C Raina MacIntyre, Professor of Global Biosecurity, NHMRC L3 Research Fellow, Head, Biosecurity Program, Kirby Institute, UNSW Sydney; Ashley Quigley, Senior Research Associate, Global Biosecurity, UNSW Sydney; Haley Stone, PhD Candidate, Biosecurity Program, Kirby Institute, UNSW Sydney; Matthew Scotch, Associate Dean of Research and Professor of Biomedical Informatics, College of Health Solutions, Arizona State University, and Rebecca Dawson, Research Associate, The Kirby Institute, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: