A Statin-Free Life – by Dr. Aseem Malhotra
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Here at 10almonds, we’ve written before about the complexities of statins, and their different levels of risk/benefit for men and women, respectively. It’s a fascinating topic, and merits more than an article of the size we write here!
So, in the spirit of giving pointers of where to find a lot more information, this book is a fine choice.
Dr. Malhotra, a consultant cardiologist and professor of evidence-based medicine, talks genes and lifestyle, drugs and blood. He takes us on a tour of the very many risk factors for heart disease, and how cholesterol levels may be at best an indicator, but less likely a cause, of heart disease, especially for women. Further and even better, he discusses various more reliable indicators and potential causes, too.
Rather than be all doom and gloom, he does offer guidance on how to reduce each of one’s personal risk factors and—which is important—keep on top of the various relevant measures of heart health (including some less commonly tested ones, like the coronary calcium score).
The style is light reading andyet with a lot of reference to hard science, so it’s really the best of both worlds in that regard.
Bottom line: if you’re considering statins, or are on statins and are reconsidering that choice, then this book will (notwithstanding its own bias in its conclusion) help you make a more-informed decision.
Click here to check out A Statin-Free Life, and make the best choice for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
My dance school is closed for the summer, how can I keep up my fitness?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Once the end-of-year dance concert and term wrap up for the year it is important to take a break. Both physical and mental rest are important and taking a few weeks off can help your body repair and have a mental break from dance.
If your mind and body are in need of an extended break (such as more than a few weeks), then it’s more than OK to take longer off, especially if you are training at a competitive or pre-professional level.
There is benefit in enjoying other aspects of your life outside of dance such as spending time with family, friends and enjoying hobbies.
Tatyana Vyc/Shutterstock A safe, fulfilling dancing life
Creating meaning and value in life outside of dance and expanding sense of self can make it easier to lean into other aspects when experiencing change or difficult times during dance training such as being injured.
Taking an extended break from dance training will, however, mean losing some fitness and physical capacity. When you return to dance your body will take time to return to full capacity again.
Approaches such as being “whipped back into shape” can promote sudden spikes in training load (hours and intensity of training) which can increase the risk of injury. It is advised to gradually and progressively increase training load over time to allow the body to adapt and return to full capacity safely.
A four-to-six week period of gradually progressing training load and introducing jumping has been suggested in dance settings.
For dancers wanting to maintain fitness over the summer holidays, a great place to start is focusing on building a physical foundation.
Exercise like running can help build a physical foundation. Jacek Chabraszewski/Shutterstock Building a physical foundation means focusing on targeted areas of fitness such as full body strength, cardiovascular fitness or stamina (such as skipping, cycling walking, running, swimming), flexibility, and some dance-specific conditioning (for example, calf rises for ballet).
A good physical foundation will mean an improved capacity and fitness level so your body is ready to take on more challenging dance movements and routines once you return to the studio.
Building full body strength at home or at the park
A great place to start is by choosing movements that require your muscles to work to support your own body weight.
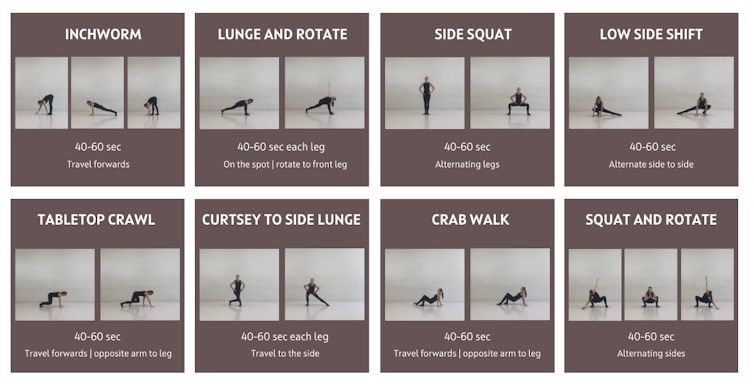
Fundamental movements such as crawling (moving on the floor on hands and feet) and locomotion (travelling movements such as lunging, hopping, sliding) are great for developing body control, arm and leg stability and coordinated movement patterns.
Below is a sequence that can be used as a warm up and even as a workout itself. The ten minute sequence is based on gross motor and fundamental movement patterns. It includes exercises that work through a range of joint movements and in multiple planes (forwards, sideways, rotating).
This fundamental movement sequence can be used as a warm-up or a workout. Joanna Nicholas, CC BY Once feeling comfortable with the above fundamental movements, it is time to introduce body weight resistance exercises.
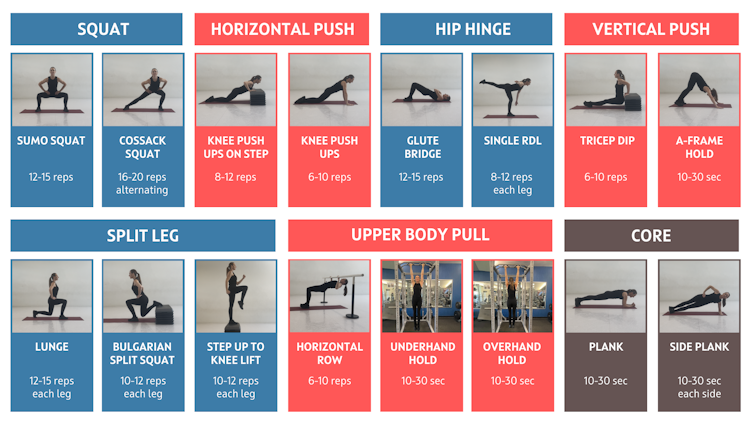
Body weight resistance exercises can be beneficial for developing a strong foundation for dance movements such as jumping, landing, floorwork, partnering and aerial work.
Exercises from the above sequence can be used to form a safe and effective neuromuscular warm up.
Aim to include one exercise from each of the below movement categories (squat, horizontal push etc) to build your own workout.
Aim to complete two to three sets (or rounds) of each exercise with about one minute rest between sets. An alternative is to complete one set of each exercise with minimal rest between, then complete a second or third time.
If training with friends, you could set a timer and do each exercise for up to 50 seconds (instead of counting reps) and take ten seconds to transition to the next exercise.
Depending on your level of strength you may need to do fewer repetitions and build up sets and repetitions overtime. After you have completed the body weight exercises complete a cool down including stretches for the upper and lower body muscles. Be sure to use a sturdy bar (such as an outdoor fitness station) for horizontal row and overhead hold.
Exercises may need to be modified depending on fitness level and physical limitations such as injury.
You can build your own full body strength workout using these movements. Joanna Nicholas, CC BY How often should I train?
A common misconception in dance is that “more is better”. This belief can lead to dancers training long hours on most or all days of the week which can lead to overtraining, plateauing and increased risk of injury.
Our bodies require sufficient time between training sessions to adapt and get stronger and fitter. The time between sessions is when our muscles and tissues repair and training gains are made.
By incorporating adequate recovery (including sleep and downtime) and including rest days throughout the week, our bodies can gain the most benefits from training.
Rest days are important, too. Manop Boonpeng/Shutterstock Muscles can take up to 48–72 hours to recover from most types of strength-based exercises (the more intense the longer they’ll need to recover).
Aerobic activity at low intensity, such as a brisk walk, can be done most days (24-hour recovery) while high stress anaerobic exercise such as high intensity intervals or sprints can take three days or more to recover from.
Aim to spread training sessions out over the week and allow time to recover between sessions.
Below is an example weekly schedule based on incorporating adequate recovery between sessions, and incorporating polarised training where some days are harder and others are easier.
Seek guidance from your healthcare provider and/or an exercise professional prior to undertaking a new exercise program.
Joanna Nicholas, Lecturer in Dance and Performance Science, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Increase in online ADHD diagnoses for kids poses ethical questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In 2020, in the midst of a pandemic, clinical protocols were altered for Ontario health clinics, allowing them to perform more types of care virtually. This included ADHD assessments and ADHD prescriptions for children – services that previously had been restricted to in-person appointments. But while other restrictions on virtual care are back, clinics are still allowed to virtually assess children for ADHD.
This shift has allowed for more and quicker diagnoses – though not covered by provincial insurance (OHIP) – via a host of newly emerging private, for-profit clinics. However, it also has raised significant ethical questions.
It solves an equity issue in terms of rural access to timely assessments, but does it also create new equity issues as a privatized service?
Is it even feasible to diagnose a child for a condition like ADHD without meeting that child in person?
And as rates of ADHD diagnosis continue to rise, should health regulators re-examine the virtual care approach?
Ontario: More prescriptions, less regulation
There are numerous for-profit clinics offering virtual diagnoses and prescriptions for childhood ADHD in Ontario. These include KixCare, which does not offer the option of an in-person assessment. Another clinic, Springboard, makes virtual appointments available within days, charging around $2,600 for assessments, which take three to four hours. The clinic offers coaching and therapy at an additional cost, also not covered by OHIP. Families can choose to continue to visit the clinic virtually during a trial stage with medications, prescribed by a doctor in the clinic who then sends prescribing information back to the child’s primary care provider.
For-profit clinics like these are departing from Canada’s traditional single-payer health care model. By charging patients out-of-pocket fees for services, the clinics are able to generate more revenue because they are working outside of the billing standards for OHIP, standards that set limits on the maximum amount doctors can earn for providing specific services. Instead many services are provided by non-physician providers, who are not limited by OHIP in the same way.
Need for safeguards
ADHD prescriptions rose during the pandemic in Ontario, with women, people of higher income and those aged 20 to 24 receiving the most new diagnoses, according to research published in January 2024 by a team including researchers from the Centre for Addictions and Mental Health and Holland Bloorview Children’s Hospital. There may be numerous reasons for this increase but could the move to virtual care have been a factor?
Ontario psychiatrist Javeed Sukhera, who treats both children and adults in Canada and the U.S., says virtual assessments can work for youth with ADHD, who may receive treatment quicker if they live in remote areas. However, he is concerned that as health care becomes more privatized, it will lead to exploitation and over-diagnosis of certain conditions.
“There have been a lot of profiteers who have tried to capitalize on people’s needs and I think this is very dangerous,” he said. “In some settings, profiteering companies have set up systems to offer ADHD assessments that are almost always substandard. This is different from not-for-profit setups that adhere to quality standards and regulatory mechanisms.”
Sukhera’s concerns recall the case of Cerebral Inc., a New York state-based virtual care company founded in 2020 that marketed on social media platforms including Instagram and TikTok. Cerebral offered online prescriptions for ADHD drugs among other services and boasted more than 200,000 patients. But as Dani Blum reported in the New York Times, Cerebral was accused in 2023 of pressuring doctors on staff to prescribe stimulants and faced an investigation by state prosecutors into whether it violated the U.S. Controlled Substances Act.
“At the start of the pandemic, regulators relaxed rules around medical prescription of controlled substances,” wrote Blum. “Those changes opened the door for companies to prescribe and market drugs without the protocols that can accompany an in-person visit.”
Access increased – but is it equitable?
Virtual care has been a necessity in rural areas in Ontario since well before the pandemic, although ADHD assessments for children were restricted to in-person appointments prior to 2020.
But ADHD assessment clinics that charge families out-of-pocket for services are only accessible to people with higher incomes. Rural families, many of whom are low income, are unable to afford thousands for private assessments, let alone the other services upsold by providers. If the private clinic/virtual care trend continues to grow unchecked, it may also attract doctors away from the public model of care since they can bill more for services. This could further aggravate the gap in care that lower income people already experience.
This could further aggravate the gap in care that lower income people already experience.
Sukhera says some risks could be addressed by instituting OHIP coverage for services at private clinics (similar to private surgical facilities that offer mixed private/public coverage), but also with safeguards to ensure that profits are reinvested back into the health-care system.
“This would be especially useful for folks who do not have the income, the means to pay out of pocket,” he said.
Concerns of misdiagnosis and over-prescription
Some for-profit companies also benefit financially from diagnosing and issuing prescriptions, as has been suggested in the Cerebral case. If it is cheaper for a clinic to do shorter, virtual appointments and they are also motivated to diagnose and prescribe more, then controls need to be put in place to prevent misdiagnosis.
The problem of misdiagnosis may also be related to the nature of ADHD assessments themselves. University of Strathclyde professor Matthew Smith, author of Hyperactive: The Controversial History of ADHD, notes that since the publication of Diagnostic and Statistical Manual of Mental Disorders in 1980, assessment has typically involved a few hours of parents and patients providing their subjective perspectives on how they experience time, tasks and the world around them.
“It’s often a box-ticking exercise, rather than really learning about the context in which these behaviours exist,” Smith said. “The tendency has been to use a list of yes/no questions which – if enough are answered in the affirmative – lead to a diagnosis. When this is done online or via Zoom, there is even less opportunity to understand the context surrounding behaviour.”
Smith cited a 2023 BBC investigation in which reporter Rory Carson booked an in-person ADHD assessment at a clinic and was found not to have the condition, then had a private online assessment – from a provider on her couch in a tracksuit – and was diagnosed with ADHD after just 45 minutes, for a fee of £685.
What do patients want?
If Canadian regulators can effectively tackle the issue of privatization and the risk of misdiagnosis, there is still another hurdle: not every youth is willing to take part in virtual care.
Jennifer Reesman, a therapist and Training Director for Neuropsychology at the Chesapeake Center for ADHD, Learning & Behavioural Health in Maryland, echoed Sukhera’s concerns about substandard care, cautioning that virtual care is not suitable for some of her young clients who had poor experiences with online education and resist online health care. It can be an emotional issue for pediatric patients who are managing their feelings about the pandemic experience.
“We need to respect what their needs are, not just the needs of the provider,” says Reesman.
In 2020, Ontario opted for virtual care based on the capacity of our health system in a pandemic. Today, with a shortage of doctors, we are still in a crisis of capacity. The success of virtual care may rest on how engaged regulators are with equity issues, such as waitlists and access to care for rural dwellers, and how they resolve ethical problems around standards of care.
Children and youth are a distinct category, which is why we had restrictions on virtual ADHD diagnosis prior to the pandemic. A question remains, then: If we could snap our fingers and have the capacity to provide in-person ADHD care for all children, would we? If the answer to that question is yes, then how can we begin to build our capacity?
This article is republished from healthydebate under a Creative Commons license. Read the original article.
Share This Post
-
Long-acting contraceptives seem to be as safe as the pill when it comes to cancer risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many women worry hormonal contraceptives have dangerous side-effects including increased cancer risk. But this perception is often out of proportion with the actual risks.
So, what does the research actually say about cancer risk for contraceptive users?
And is your cancer risk different if, instead of the pill, you use long-acting reversible contraceptives? These include intrauterine devices or IUDs (such as Mirena), implants under the skin (such as Implanon), and injections (such as Depo Provera).
Our new study, conducted by the University of Queensland and QIMR Berghofer Medical Research Institute and published by the Journal of the National Cancer Institute, looked at this question.
We found long-acting contraceptives seem to be as safe as the pill when it comes to cancer risk (which is good news) but not necessarily any safer than the pill.
Peakstock/Shutterstock Some hormonal contraceptives take the form of implants under the skin. WiP-Studio/Shutterstock How does the contraceptive pill affect cancer risk?
The International Agency for Research on Cancer, which compiles evidence on cancer causes, has concluded that oral contraceptives have mixed effects on cancer risk.
Using the oral contraceptive pill:
- slightly increases your risk of breast and cervical cancer in the short term, but
- substantially reduces your risk of cancers of the uterus and ovaries in the longer term.
Our earlier work showed the pill was responsible for preventing far more cancers overall than it contributed to.
In previous research we estimated that in 2010, oral contraceptive pill use prevented over 1,300 cases of endometrial and ovarian cancers in Australian women.
It also prevented almost 500 deaths from these cancers in 2013. This is a reduction of around 25% in the deaths that could have occurred that year if women hadn’t taken the pill.
In contrast, we calculated the pill may have contributed to around 15 deaths from breast cancer in 2013, which is less than 0.5% of all breast cancer deaths in that year.
Previous work showed the pill was responsible for preventing far more cancers overall than it contributed to. Image Point Fr What about long-acting reversible contraceptives and cancer risk?
Long-acting reversible contraceptives – which include intrauterine devices or IUDs, implants under the skin, and injections – release progesterone-like hormones.
These are very effective contraceptives that can last from a few months (injections) up to seven years (intrauterine devices).
Notably, they don’t contain the hormone oestrogen, which may be responsible for some of the side-effects of the pill (including perhaps contributing to a higher risk of breast cancer).
Use of these long-acting contraceptives has doubled over the past decade, while the use of the pill has declined. So it’s important to know whether this change could affect cancer risk for Australian women.
Our new study of more than 1 million Australian women investigated whether long-acting, reversible contraceptives affect risk of invasive cancers. We compared the results to the oral contraceptive pill.
We used de-identified health records for Australian women aged 55 and under in 2002.
Among this group, about 176,000 were diagnosed with cancer between 2004 and 2013 when the oldest women were aged 67. We compared hormonal contraceptive use among these women who got cancer to women without cancer.
We found that long-term users of all types of hormonal contraception had around a 70% lower risk of developing endometrial cancer in the years after use. In other words, the risk of developing endometrial cancer is substantially lower among women who took hormonal contraception compared to those who didn’t.
For ovarian cancer, we saw a 50% reduced risk (compared to those who took no hormonal contraception) for women who were long-term users of the hormone-containing IUD.
The risk reduction was not as marked for the implants or injections, however few long-term users of these products developed these cancers in our study.
As the risk of endometrial and ovarian cancers increases with age, it will be important to look at cancer risk in these women as they get older.
What about breast cancer risk?
Our findings suggest that the risk of breast cancer for current users of long-acting contraceptives is similar to users of the pill.
However, the contraceptive injection was only associated with an increase in breast cancer risk after five years of use and there was no longer a higher risk once women stopped using them.
Our results suggested that the risk of breast cancer also reduces after stopping use of the contraceptive implants.
We will need to follow-up the women for longer to determine whether this is also the case for the IUD.
It is worth emphasising that the breast cancer risk associated with all hormonal contraceptives is very small.
About 30 in every 100,000 women aged 20 to 39 years develop breast cancer each year, and any hormonal contraceptive use would only increase this to around 36 cases per 100,000.
What about other cancers?
Our study did not show any consistent relationships between contraceptive use and other cancers types. However, we only at looked at invasive cancers (meaning those that start at a primary site but have the potential to spread to other parts of the body).
A recent French study found that prolonged use of the contraceptive injection increased the risk of meningioma (a type of benign brain tumour).
However, meningiomas are rare, especially in young women. There are around two cases in every 100,000 in women aged 20–39, so the extra number of cases linked to contraceptive injection use was small.
The French study found the hormonal IUD did not increase meningioma risk (and they did not investigate contraceptive implants).
Benefits and side-effects
There are benefits and side-effects for all medicines, including contraceptives, but it is important to know most very serious side-effects are rare.
A conversation with your doctor about the balance of benefits and side-effects for you is always a good place to start.
Susan Jordan, Professor of Epidemiology, The University of Queensland; Karen Tuesley, Postdoctoral Research Fellow, School of Public Health, The University of Queensland, and Penny Webb, Distinguished Scientist, Gynaecological Cancers Group, QIMR Berghofer Medical Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Acorns vs Chestnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing acorns to chestnuts, we picked the acorns.
Why?
In terms of macros, chestnuts are mostly water, so it’s not surprising that acorns have a lot more carbs, fat, protein, and fiber. Thus, unless you have personal reasons for any of those to be a problem, acorns are the better choice, offering a lot more nutritional value.
In the category of vitamins, acorns lead with a lot more of vitamins A, B2, B3, B5, B6, and B9, while chestnuts have more of vitamins B1 and C. However, that vitamin C is useless to us, because it is destroyed in the cooking process (by boiling or roasting), and both of these nuts can be harmful if consumed raw, so that cooking does need to be done. That leaves acorns with a 6:1 lead.
When it comes to minerals, things are more even; acorns have more copper, magnesium, manganese, and zinc, while chestnuts have more calcium, iron, phosphorus, and potassium. Thus, a 4:4 tie (and yes, the margins of difference are approximately equal too).
We mentioned “both of these nuts can be harmful if consumed raw”, so a note on that: it’s because, while both contain an assortment of beneficial phytochemicals, they also both contain tannins that, if consumed raw, chelate with iron, essentially taking it out of our diet and potentially creating an iron deficiency. Cooking tannins stops this from being an issue, and the same cooking process renders the tannins actively beneficial to the health, for their antioxidant powers.
You may have heard that acorns are poisonous; that’s not strictly speaking true, except insofar as anything could be deemed poisonous in excess (including such things as water, and oxygen). Rather, it’s simply the above-described matter of the uncooked tannins and iron chelation. Even then, you’re unlikely to suffer ill effects unless you consume them raw in a fair quantity. While acorns have fallen from popular favor sufficient that one doesn’t see them in supermarkets, the fact is they’ve been enjoyed as an important traditional part of the diet by various indigenous peoples of N. America for centuries*, and provided they are cooked first, they are a good healthy food for most people.
*(going so far as to cultivate natural oak savannah areas, by burning out young oaks to leave the old ones to flourish without competition, to maximize acorn production, and then store dried acorns in bulk sufficient to cover the next year or so in case of a bad harvest later—so these was not just an incidental food, but very important “our life may depend on this” food. Much like grain in many places—and yes, acorns can be ground into flour and used to make bread etc too)
Do note: they are both still tree nuts though, so if you have a tree nut allergy, these ones aren’t for you.
Otherwise, enjoy both; just cook them first!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Apricots vs Peaches – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apricots to peaches, we picked the apricots.
Why?
Both are great! But there’s a clear winner:
In terms of macros, apricots have more fiber and, which is less important because the numbers are small, more protein. Apricots do also have more carbs, and/but carbs from whole fruit are not a problem for most people (especially because of the fiber), unless undertaking a very carb-controlled diet.
When it comes to vitamins, apricots sweep with more of vitamins A, B1, B2, B5, B6, B9, C, E, & K. Peaches meanwhile boast more vitamin B3, and that only marginally, as well as more choline.
In the category of minerals, apricots sweep again with more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. Peaches are not higher in any minerals.
Finally, if we consider polyphenols, apricots sweep yet again. The flavonols that peaches have, apricots have more of, and apricots have a long list of flavonols that peaches don’t.
Outside of flavonols, there is one (1) phenolic acid that peaches have more of (it’s 3-Caffeoylquinic acid), and it’s only slightly more, and it’s mostly in the skin which isn’t included if you buy your fruit ready-chopped. So in those cases, apricots would have the higher 3-Caffeoylquinic acid content anyway.
All in all, with their higher content of fiber, vitamins, minerals, and polyphenols, apricots easily win the day.
Enjoy both, though! Diversity is healthy!
Want to learn more?
You might like to read:
- Dried Apricots vs Dried Prunes – Which is Healthier?
- Which Sugars Are Healthier, And Which Are Just The Same? ← we know we link this one a lot, but we think it’s important for everyone to know how fruit is good and juice isn’t (and why, less that seem bizarrely arbitrary)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Parenting a perfectionist? Here’s how you can respond
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some children show signs of perfectionism from early on. Young children might become frustrated and rip up their drawing if it’s not quite right. Older children might avoid or refuse to do homework because they’re afraid to make a mistake.
Perfectionism can lead to children feeling overwhelmed, angry and frustrated, or sad and withdrawn.
And yet perfectionism isn’t considered all bad in our society. Being called a “perfectionist” can be a compliment – code for being a great worker or student, someone who strives to do their best and makes sure all jobs are done well.
These seemingly polarised views reflect the complex nature of perfectionism.
Annie Spratt/Unsplash What is perfectionism?
Researchers often separate perfectionism into two parts:
- perfectionistic strivings: being determined to meet goals and achieve highly
- perfectionistic concerns: worry about being able to meet high standards, and self-criticism about performance.
While perfectionistic strivings can be positive and lead to high achievement, perfectionistic concerns can lead to a higher chance of children developing eating disorders or anxiety and depression, and having lower academic achievement.
Perfectionistic concerns can result in lower academic achievement. Jessica Lewis/Unsplash Children and adolescents may experience perfectionism in relation to school work, sport, performance in art or music, or in relation to their own body.
Signs of perfectionistic concerns in children and adolescents may include:
- children being highly critical of themselves
- their reactions to mistakes seeming to be an overreaction
- intense preoccupation and worry over their standards and goals and/or procrastination
- significant change in performance, for example, lower academic results
- irritability and negative emotions, stress and feelings of worthlessness
- social problems with peers and friends, such as bullying and alienating themselves from peers.
A range of genetic, biological and environmental factors influence perfectionism in children. And as a parent, our role is important. While research evidence suggests we can’t successfully increase positive perfectionistic strivings in our children, harsh or controlling parenting can increase negative perfectionistic concerns in children.
Parents who are perfectionistic themselves can also model this to their children.
So, how can we walk the line between supporting our child’s interests and helping them to achieve their potential, without pressuring them and increasing the risk of negative outcomes?
Give them space to grow
A great metaphor is the gardener versus the carpenter described by psychology professor Alison Gopnik.
Instead of trying to build and shape our children by controlling them and their environment (like a carpenter), parents can embrace the spirit of the gardener – providing lots of space for children to grow in their own direction, and nourishing them with love, respect and trust.
Parents don’t need to control their child and their environment. Noah Silliman/Unsplash We can’t control who they become, so it’s better to sit back, enjoy the ride, and look forward to watching the person they grow into.
However, there is still plenty we can do as parents if our child is showing signs of perfectionism. We can role model to our children how to set realistic goals and be flexible when things change or go wrong, help our children manage stress and negative emotions, and create healthy balance in our family daily routine.
Set realistic goals
People with perfectionistic tendencies will often set unattainable goals. We can support the development of flexibility and realistic goal setting by asking curious questions, for example, “what would you need to do to get one small step closer to this goal?” Identifying upper and lower limits for goals is also helpful.
If your child is fixed on a high score at school, for example, set that as the “upper limit” and then support them to identify a “lower limit” they would find acceptable, even if they are less happy with the outcome.
This strategy may take time and practice to widen the gap between the two, but is useful to create flexibility over time.
If a goal is performance-based and the outcome cannot be guaranteed (for example, a sporting competition), encourage your child to set a personal goal they have more control over.
Parents can help children set goals they can achieve. liz99/Unsplash We can also have conversations about perfectionism from early on, and explain that everyone makes mistakes. In fact, it’s great to model this to our children – talking about our own mistakes and feelings, to show them that we ourselves are not perfect.
Talk aloud practices can help children to see that we “walk the walk”. For example, if you burn dinner you could reflect:
I’m disappointed because I put time and effort into that and it didn’t turn out as I expected. But we all make mistakes. I don’t get things right every time.
Manage stress and negative emotions
Some children and adolescents have a natural tendency towards perfectionism. Rather than trying to control their behaviour, we can provide gentle, loving support.
When our child or adolescent becomes frustrated, angry, sad or overwhelmed, we support them best by helping them to name, express and validate all of their emotions.
Parents may fear that acknowledging their child’s negative emotions will make the emotions worse, but the opposite is true.
Creating healthy balance
The building blocks of healthy child development are strong loving family relationships, good nutrition, creative play and plenty of physical activity, sleep and rest.
Perfectionism is associated with rigidity, and thinking that there is only one correct way to succeed. We can instead encourage flexibility and creativity in children.
Children’s brains grow through play. There is strong research evidence showing that creative, child-led play is associated with higher emotion regulation skills, and a range of cognitive skills, including problem-solving, memory, planning, flexibility and decision-making.
Play helps children’s brains grow. Mi Pham/Unsplash Play isn’t just for young children either – there’s evidence that explorative, creative play of any kind also benefits adolescents and adults.
There is also evidence that getting active outdoors in nature can promote children’s coping skills, emotion regulation and cognitive development.
Elizabeth Westrupp, Associate Professor in Psychology, Deakin University; Gabriella King, Associate Research Fellow, Deakin University, and Jade Sheen, Associate Professor, School of Psychology, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: