Beyond Guarding Against Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Age’s Brain-Changes Come Knocking
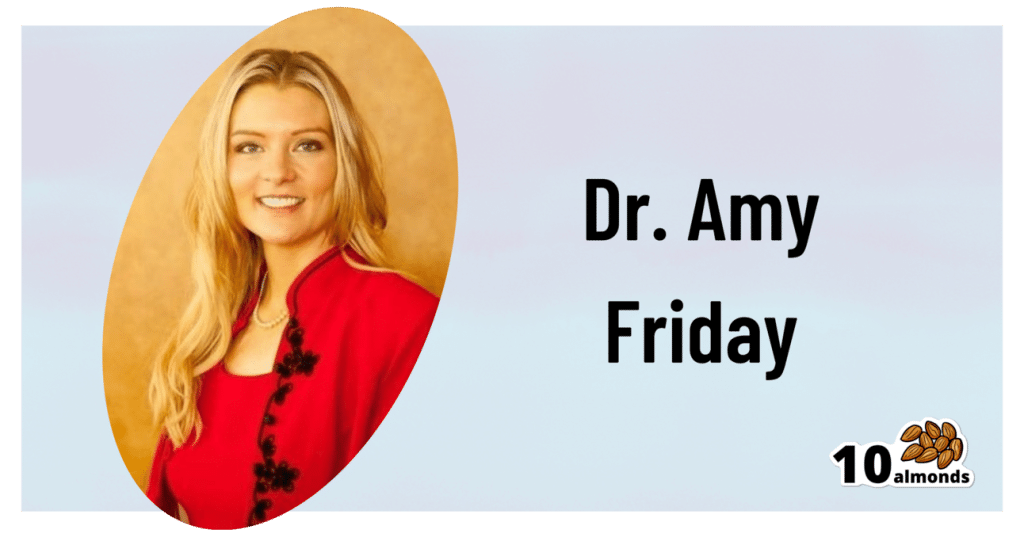
This is Dr. Amy Friday. She’s a psychologist, specializing in geropsychology and neuropsychological assessments.
In other words, she helps people optimize their aging experience, particularly in the context of brain changes as we get older.
What does she want us to know?
First: be not afraid
Ominous first words, but the fact is, there’s a lot to find scary about the prospect of memory loss, dementia, and death.
However, as she points out:
- Death will come for us all sooner or later, barring technology as yet unknown
- Dementia can be avoided, or at least stalled, or at least worked around
- Memory loss, as per the above, can be avoided/stalled/managed
We’ve written a little on these topics too:
…or if the death is not yours:
As for avoiding dementia, the below-linked feature is about Alzheimer’s in particular (which accounts for more than half of all cases of dementia), but the advice goes for most of the other kinds too:
How To Reduce Your Alzheimer’s Risk
And finally, about memory loss specifically:
How To Boost Your Memory Immediately (Without Supplements)
this one is especially about cementing into one’s brain the kinds of memories that people most fear losing with age. People don’t worry about forgetting their PIN codes; they worry about forgetting their cherished memories with loved ones. So, if that’s important to you, do consider checking out this one!
What is that about managing or working around the symptoms?
If we’re missing a limb, we (usually) get a prosthetic, and/or learn how to operate without that limb.
If we’re missing sight or hearing, partially or fully, there are disability aids for those kinds of things too (glasses are a disability aid! Something being very common does not make it not a disability; you literally have less of an ability—in this case, the ability to see), and/or we learn how to operate with our different (or missing) sense.
Dr. Friday makes the case for this being the same with memory loss, dementia, and other age-related symptoms (reduced focus, increased mental fatigue, etc):
❝We are all screwed up. Here’s my flavor … what’s yours? This is a favorite saying of mine, because we ARE all screwed up in one way or another, and when we acknowledge it we can feel closer in our screwed-up-edness.
We are all experiencing “normal aging,” so that tip-of-the-tongue phenomenon that starts in our thirties and slowly gets worse is REAL. But what if you’re having more problems than normal aging? Is it time to throw in the towel and hide? I’m hoping that there is a group of people who say HELL NO to that idea.
Let’s use lessons from research and clinical practice to help all of us work around our weaknesses, and capitalize on our strengths. ❞
Examples of this might include:
- Writing down the things most important to you (a short list of information and/or statements that you feel define you and what matters most to you), so that you can read it later
- Making sure you have support (partner, family, friends, etc) who are on the same page about this topic—and thus will actually support you and advocate for you, instead of arguing about what is in your best interest without consulting you.
- Labelling stuff around the house, so that you get less confused about what is what and where it is
- Having a named go-to advocate that you can call / ask to be called, if you are in trouble somewhere and need help that you can rely on
- Getting a specialized, simpler bank account; hiring an accountant if relevant and practicable.
The thing is, we all want to keep control. Sometimes we can do that! Sometimes we can’t, and if we’re going to lose some aspect of control, it’ll generally go a lot better if we do it on our own terms, so that we ourselves can look out for future-us in our planning.
Want to know more?
You might enjoy her blog, which includes also links to her many videos on the topic, including such items as:
- Neuroplasticity – #1 Way To Increase Brain Health
- Which Diet PREVENTS Alzheimer’s? | Best Brain Health Diet
- Stop Anxiety About Dementia & Do I Have Dementia?
For the rest, see:
This Beautiful Brain | The Science Of Brain Health
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
On This Bright Day – by Dr. Susan Thompson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is principally aimed at those who have struggled with emotional/comfort eating, over-eating, and/or compulsive eating of some kind.
However, its advices go for the “little compulsions” too, the many small unhealthy choices that add up. Thus, this book has value for most if not all of us.
The format is: each day has a little quotation, followed by a short discussion of that, which is then underlined by an affirmation for the day.
The main thrust of the book is to promote mindful eating, and it does this well with daily reminders that are helpful without being preachy.
Bottom line: if you enjoy “daily reader” type books and would like a daily reminder to practice mindful eating, then this book is for you!
Click here to check out On This Bright Day, and enjoy your food mindfully, every day!
Share This Post
-
Having dense breasts is linked to cancer. But advice about breast density can depend on where you live
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Having dense breasts is a clear risk factor for breast cancer. It can also make cancers hard to spot on mammograms.
Yet you might not be aware you have dense breasts, even after mammographic screening.
In Australia, advice for women with dense breasts and their health-care professionals can be inconsistent and confusing.
This is because there’s not currently consensus on whether women who have dense breasts, but no symptoms, benefit from further imaging such as ultrasounds. Concerns include potential cost of these tests and the risk they can produce false positives.
Gorodenkoff/Shutterstock What is breast density?
Breasts are made up of fatty tissue and fibroglandular tissue (including glands that make milk, held together by fibrous tissue).
On a mammogram – an x-ray of the breast – fibroglandular tissue appears white and fatty tissue appears dark. The white areas are referred to as breast density.
Fibroglandular tissue shows up white on a mammogram. Nata Sokhrannova/Shutterstock A higher proportion of fibroglandular tissue means your breasts are dense.
There are four categories to classify breast density:
- A: almost entirely fatty
- B: scattered areas of fibroglandular density
- C: heterogeneously or consistently dense
- D: extremely dense.
Breast density is very common. Around 40% of women aged 40–74 are estimated to have “dense breasts”, meaning they fall in category C or D.
What’s the link to cancer?
Breast density is associated with the risk of breast cancer in two ways.
First, breast density usually decreases with age. But if a woman has high breast density for her age, it increases her likelihood of breast cancer.
One study looked at the risk of breast cancer over the age of 50. It found there was a 6.2% risk for the one-third of women with the lowest density. For the 5% with the highest density, the risk was 14.7%.
Second, breast density “masks” cancers if they develop. Both cancers and breast density appear white on a mammogram, making cancers very hard to see.
Breast cancer screening saves lives through early detection and improved treatment options. But we don’t yet know if telling women about their breast density leads to earlier cancer detection, or lives saved.
In Australia, screening mammography is free for all women* aged 40 and older. This is run through BreastScreen Australia, a joint national, state and territory initiative. Those aged 50-74 are invited to have a mammogram, but it’s available for free without a referral from age 40.
However, the messages Australian women currently receive about breast density – and whether it’s recorded – depends on where they live.
What does the advice say?
In 2023, the Royal Australian and New Zealand College of Radiologists updated its position statement to recommend breast density is recorded during screening and diagnostic tests in Australia and New Zealand.
Meanwhile BreastScreen Australia says it “should not routinely record breast density or provide supplemental testing for women with dense breasts”. However this position statement is from 2020 and is currently under review.
Some state and territory BreastScreen programs, including in Western Australia, South Australia and soon Victoria, notify women if they have dense breasts. Victoria is currently at an early stage of its roll-out.
While the messaging regarding breast density differs by state, none currently recommend further imaging for women with dense breasts without speaking to a doctor about individual risk.
What are the issues?
Providing recommendations for women with dense breasts is difficult.
The European Society of Breast Imaging recommends women with extremely dense breasts aged 50–70 receive an MRI every two to four years, in addition to screening mammography. This is based on a large randomised controlled trial from the Netherlands.
But the Royal Australian and New Zealand College of Radiologists describes this recommendation as “aspirational”, acknowledging cost, staffing and accessibility as challenges.
That is, it is not feasible to provide a supplemental MRI for everyone in the screening population in category D with extremely dense breasts (around 10%).
Further, there is no consensus on appropriate screening recommendations for women in the category C (heterogeneous density).
We need a national approach to breast density reporting in Australia and to do better at identifying who is most likely to benefit from further testing.
BreastScreen Australia is currently undergoing a review of its policy and funding.
One of its goals is to enable a nationally consistent approach to breast screening practices. Hopefully breast density reporting, including funding to support national implementation, will be a priority.
*This includes those recorded female at birth and who are gender diverse.
Jennifer Stone, Principal Research Fellow, School of Population and Global Health, The University of Western Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Worry Trick – by Dr. David Carbonell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Worry is a time-sink that rarely does us any good, and often does us harm. Many books have been written on how to fight anxiety… That’s not what this book’s about.
Dr. David Carbonell, in contrast, encourages the reader to stop trying to avoid/resist anxiety, and instead, lean into it in a way that detoothes it.
He offers various ways of doing this, from scheduling time to worry, to substituting “what if…” with “let’s pretend…”, and guides the reader through exercises to bring about a sort of worry-desensitization.
The style throughout is very much pop-psychology and is very readable.
If the book has a weak point, it’s that it tends to focus on worrying less about unlikely outcomes, rather than tackling worry that occurs relating to outcomes that are likely, or even known in advance. However, some of the techniques will work for such also! That’s when Dr. Carbonell draws from Acceptance and Commitment Therapy (ACT).
Bottom line: if you would like to lose less time and energy to worrying, then this is a fine book for you.
Click here to check out The Worry Trick, and repurpose your energy reserves!
Share This Post
Related Posts
-
Modern Friendship – by Anna Goldfarb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a topic we’ve covered before at 10almonds: Human Connection In An All-Too-Busy World.
Here, however, Goldfarb has an entire book to cover what we had one article to cover, so of course it’s a lot more in-depth.
Importantly, if also covers: what if you seem to be doing everything right, and it’s still not working out? What if you’re already reaching out, suggesting things, doing your part?
Piece by piece, she uncovers what the very many problems are, ranging from availability issues and priorities, to health concerns and financial difficulties, to challenges as diverse as trust issues and exhaustion, and much more.
After all the hard truths about modern friendship, she gets onto equally cheery topics such as why friendships fail, but fear not, solutions are forthcoming too—and indeed, that’s what most of the book is about.
Covering such topics as desire, diligence, and delight, we learn how to not only practise wholehearted friendship, but also, how to matter to others, too. She finishes up with a “14-day friendship cleanse”, which sounds a lot more alarming than it actually is.
The style is interesting, being personal and, well, friendly throughout—but still with scholarly citations as we go along, and actual social science rather than mere conjecture.
Bottom line: if you find that your friendships are facing challenges, this book can help you to get to the bottom of any problems and move forwards (likely doing so together).
Click here to check out Modern Friendship, and learn how to truly nurture and grow your connections!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Gutbliss – by Dr. Robynne Chutkan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed another of (gastroenterologist) Dr. Chutkan’s books, “The Anti-Viral Gut”, but Gutbliss is her most well-known book, and here’s why:
This book goes into a lot more detail than most gut health books. You probably already know to eat fiber and enjoy an occasional probiotic, and chances are good you’ve already at least considered screening for food sensitivities/intolerances/allergies, especially common ones like lactose and gluten.
So, well beyond such, Dr. Chutkan talks about the very many things that affect our gut health, and countless small tweaks we can make to improve things, and the very least not sabotage ourselves. A lot of the advice is of course dietary, but some is other aspects of lifestyle, and a lot of items are things like “do this at this time of day, not that time of day”, or “do this and this, but not together”, and similar such advices that come from a place of deep professional knowledge.
The “10-day plan” promised by the subtitle is of course delivered, and while it may seem a bold claim, do remember that the life cycle of things in your gut is very very short, so 10 days is more than enough time for a complete reset, if doing things correctly.
The style is very accessible pop science, making this very easy to implement.
Bottom line: if you’d like your gut health to be better than it is, this book has a wealth of information to guide you through doing exactly that.
Click here to check out Gutbliss, and enjoy how much healthier you can feel!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
It’s Not You, It’s Your Hormones – by Nicki Williams, DipION, mBANT, CNHC
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So, first a quick note: this book is very similar to the popular bestseller “The Galveston Diet”, not just in content, but all the way down to its formatting. Some Amazon reviewers have even gone so far as to suggest that “It’s Not You, It’s Your Hormones” (2017) brazenly plagiarized “The Galveston Diet” (2023). However, after carefully examining the publication dates, we feel quite confident that this book is not a copy of the one that came out six years after it. As such, we’ve opted for reviewing the original book.
Nicki Williams’ basic principle is that we can manage our hormonal fluctuations, by managing our diet. Specifically, in three main ways:
- Intermittent fasting
- Anti-inflammatory diet
- Eating more protein and healthy fats
Why should these things matter to our hormones? The answer is to remember that our hormones aren’t just the sex hormones. We have hormones for hunger and satedness, hormones for stress and relaxation, hormones for blood sugar regulation, hormones for sleep and wakefulness, and more. These many hormones make up our endocrine system, and affecting one part of it will affect the others.
Will these things magically undo the effects of the menopause? Well, some things yes, other things no. No diet can do the job of HRT. But by tweaking endocrine system inputs, we can tweak endocrine system outputs, and that’s what this book is for.
The style is very accessible and clear, and Williams walks us through the changes we may want to make, to avoid the changes we don’t want.
In the category of criticism, there is some extra support that’s paywalled, in the sense that she wants the reader to buy her personally-branded online plan, and it can feel a bit like she’s holding back in order to upsell to that.
Bottom line: this book is aimed at peri-menopausal and post-menopausal women. It could also definitely help a lot of people with PCOS too, and, when it comes down to it, pretty much anyone with an endocrine system. It’s a well-evidenced, well-established, healthy way of eating regardless of age, sex, or (most) physical conditions.
Click here to check out It’s Not You, It’s Your Hormones, and take control of yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: