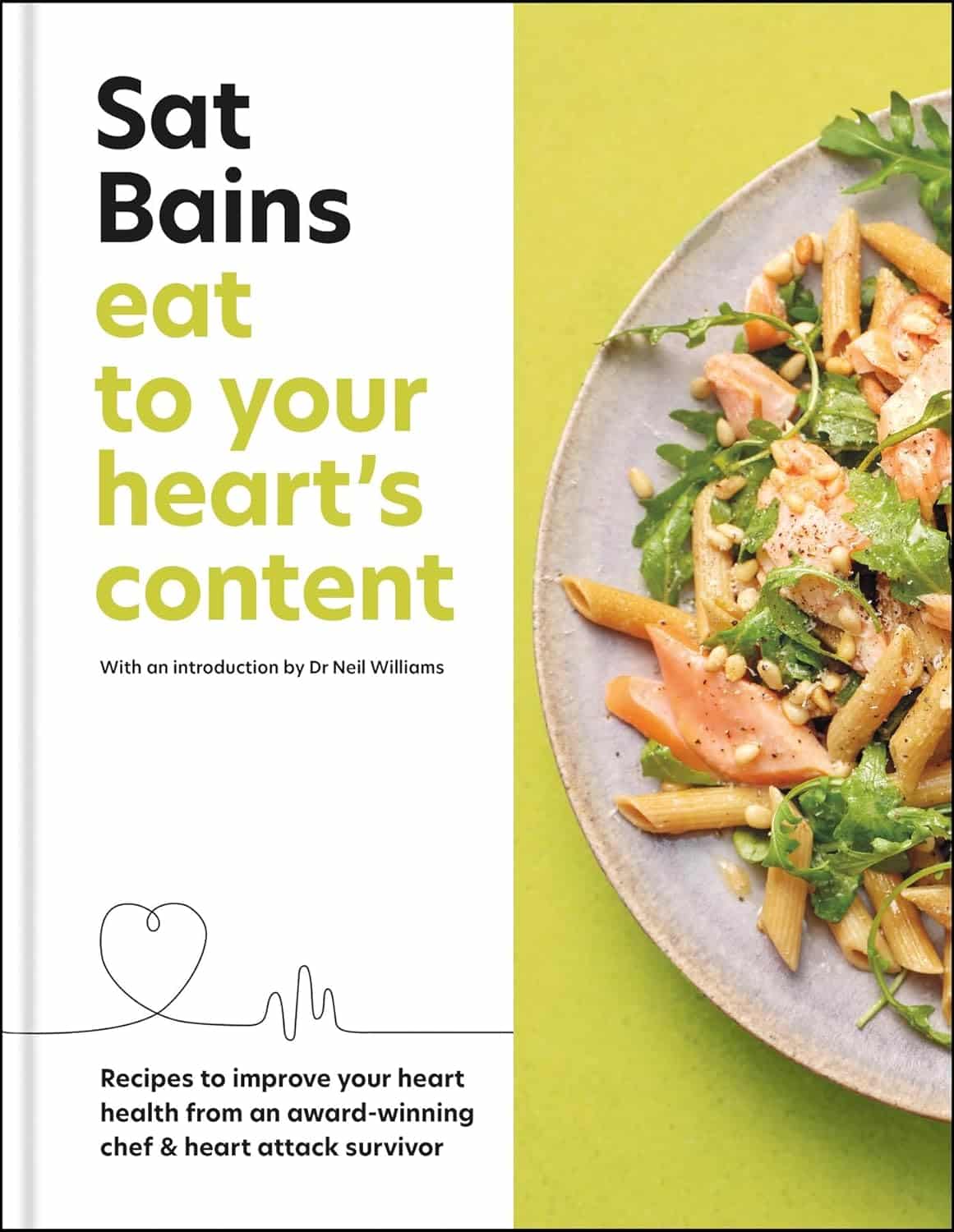
Eat to Your Heart’s Content – by Dr. Sat Bains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Making food heart-healthy and tasty is a challenge that vexes many, but it doesn’t have to be so difficult.
Dr. Sat Bains, a professional chef with multiple Michelin stars to his name, is an expert on “tasty”, and after surviving a heart attack himself, he’s become an expert on “heart-healthy” since then.
The book contains not only the recipes (of which there are 68, by the way), but also large sections of explanation of what makes various ingredients or methods heart-healthy or heart-unhealthy.
There’s science in there too, and these sections were written under the guidance of Dr. Neil Williams, a lecturer in physiology and nutrition.
You may be wondering as to why the author himself has a doctorate too; in fact he has three, none of which are relevant:
- Doctor of Arts
- Doctor of Laws
- Doctor of Hospitality (Honorary)
…but we prefix “Dr.” when people are that and he is that. The expertise we’re getting here though is really his culinary skill and extracurricular heart-healthy learning, plus Dr. Williams’ actual professional health guidance.
Bottom line: if you’d like heart-healthy recipes with restaurant-level glamour, this book is a fine choice.
Click here to check out Eat To Your Heart’s Content, and look after yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Comfortable with Uncertainty – by Pema Chödrön
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is exactly what the subtitle claims it to be: 108 teachings on cultivating fearlessness and compassion. They are short extracts, entire of themselves, taken from Chödrön’s wider work and arranged to offer her insights and advices on this one topic, in one place.
It is worth noting, by the way, that the author is a Buddhist nun, and as such, the principles and practices are Buddhist in origin. If that’s a problem for you, then this book will not be for you. It does not, however, require that the reader be Buddhist to benefit, simply that one has a will to be calm in the face of chaos, and yet not indifferent—rather, to take on the challenges of life with a whole heart.
And about that compassion? This is about alleviating suffering; your own, and the suffering in the world as a whole, increasingly uncertain as this world is. And being brave enough to do that, in a world that is not always gentle.
The style is idiosyncratic, and you will likely love it or hate it. If you love it, then you will find this book at once both soothing and empowering; if not, you will put the book down and pick up a book on CBT or something instead.
Bottom line: this book absolutely does deliver on its title/subtitle promises—provided you, dear reader, internalize it and practise it.
Click here to check out Comfortable with Uncertainty, and get comfortable with uncertainty!
Share This Post
-
12 Questions For Better Brain Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We usually preface our “Expert Insights” pieces with a nice banner that has a stylish tall cutout that allows us to put a photo of the expert in. Today we’re not doing that, because for today’s camera-shy expert, we could only find one photo, and it’s a small, grainy, square headshot that looks like it was taken some decades ago, and would not fit our template at all. You can see it here, though!
In any case, Dr. Linda Selwa is a neurologist and neurophysiologist with nearly 40 years of professional experience.
The right questions to ask
As a neurologist, she found that one of the problems that results in delayed interventions (and thus, lower efficacy of those interventions) is that people don’t know there’s anything to worry about until a degenerative brain condition has degenerated past a certain point. With that in mind, she bids us ask ourselves the following questions, and discuss them with our primary healthcare providers as appropriate:
- Sleep: Are you able to get sufficient sleep to feel rested?
- Affect, mood and mental health: Do you have concerns about your mood, anxiety, or stress?
- Food, diet and supplements: Do you have concerns about getting enough or healthy enough food, or have any questions about supplements or vitamins?
- Exercise: Do you find ways to fit physical exercise into your life?
- Supportive social interactions: Do you have regular contact with close friends or family, and do you have enough support from people?
- Trauma avoidance: Do you wear seatbelts and helmets, and use car seats for children?
- Blood pressure: Have you had problems with high blood pressure at home or at doctor visits, or do you have any concerns about blood pressure treatment or getting a blood pressure cuff at home?
- Risks, genetic and metabolic factors: Do you have trouble controlling blood sugar or cholesterol? Is there a neurological disease that runs in your family?
- Affordability and adherence: Do you have any trouble with the cost of your medicines?
- Infection: Are you up to date on vaccines, and do you have enough information about those vaccines?
- Negative exposures: Do you smoke, drink more than one to two drinks per day, or use non-prescription drugs? Do you drink well water, or live in an area with known air or water pollution?
- Social and structural determinants of health: Do you have concerns about keeping housing, having transportation, having access to care and medical insurance, or being physically or emotionally safe from harm?
You will note that some of these are well-known (to 10almonds readers, at least!) risk factors for cognitive decline, but others are more about systemic and/or environmental considerations, things that don’t directly pertain to brain health, but can have a big impact on it anyway.
About “concerns”: in the case of those questions that ask “do you have concerns about…?”, and you’re not sure, then yes, you do indeed have concerns.
About “trouble”: as for these kinds of health-related questionnaires in general, if a question asks you “do you have trouble with…?” and your answer is something like “no, because I have a special way of dealing with that problem” then the answer for the purposes of the questionnaire is yes, you do indeed have trouble.
Note that you can “have trouble with” something that you simultaneously “have under control”—just as a person can have no trouble at all with something that they leave very much out of control.
Further explanation on each of the questions
If you’re wondering what is meant by any of these, or what counts, or why the question is even being asked, then we recommend you check out Dr. Selwa et al’s recently-published paper, then all is explained in there, in surprisingly easy-to-read fashion:
Emerging Issues In Neurology: The Neurologist’s Role in Promoting Brain Health
If you scroll past the abstract, introduction, and disclaimers, then you’ll be straight into the tables of information about the above 12 factors.
Want to be even more proactive?
Check out:
How To Reduce Your Alzheimer’s Risk
Take care!
Share This Post
-
Walnut, Apricot, & Sage Nut Roast
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s important to have at least one good nut roast recipe in your repertoire. It’s something that’s very good for making a good dish out of odds and ends that are in your house, and done well, it’s not only filling and nutritious, but a tasty treat too. Done badly, everyone knows the results can be unfortunate… Making this the perfect way to show off your skills!
You will need
- 1 cup walnuts
- ½ cup almonds
- ¼ cup whole mixed seeds (chia, pumpkin, & poppy are great)
- ¼ cup ground flax (also called flax meal)
- 1 medium onion, finely chopped
- 1 large carrot, grated
- 4 oz dried apricots, chopped
- 3 oz mushrooms, chopped
- 1 oz dried goji berries
- ½ bulb garlic, crushed
- 2 tbsp fresh sage, chopped
- 1 tbsp nutritional yeast
- 2 tsp dried rosemary
- 2 tsp dried thyme
- 2 tsp black pepper, coarse ground
- 1 tsp yeast extract (even if you don’t like it; trust us; it will work) dissolved in ¼ cup hot water
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃, and line a 2 lb loaf tin with baking paper.
2) Heat some oil in a skillet over a moderate heat, and fry the onion for a few minutes until translucent. Add the garlic, carrot, and mushrooms, cooking for another 5 minutes, stirring well. Set aside to cool a little once done.
3) Process the nuts in a food processor, pulsing until they are well-chopped but not so much that they turn into flour.
4) Combine the nuts, vegetables, and all the other ingredients in a big bowl, and mix thoroughly. If it doesn’t have enough structural integrity to be thick and sticky and somewhat standing up by itself if you shape it, add more ground flax. If it is too dry, add a little water but be sparing.
5) Spoon the mixture into the loaf tin, press down well (or else it will break upon removal), cover with foil and bake for 30 minutes. Remove the foil, and bake for a further 15 minutes, until firm and golden. When done, allow it to rest in the tin for a further 15 minutes, before turning it out.
6) Serve, as part of a roast dinner (roast potatoes, vegetables, gravy, etc).
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You Should Diversify Your Nuts!
- Chia Seeds vs Pumpkin Seeds – Which is Healthier?
- Apricots vs Peaches – Which is Healthier?
- Goji Berries: Which Benefits Do They Really Have?
- Ergothioneine: “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Share This Post
Related Posts
-
Tiramisu Crunch Bites
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s coffee, it’s creamy, it’s nutty, it’s chocolatey, what’s not to love? It has all the well-loved flavors of tiramisu, but this recipe is a simple one, and it’s essentially stuffed dates in a way you’ve never had them before. They’re delectable, decadent, and decidedly good for your health. These things are little nutrient-bombs that’ll keep you reaching for more.
You will need
- Coffee (we will discuss this)
- 150g (5.5oz) mascarpone (if vegan or lactose-intolerant, can be substituted with vegan varieties, or at a pinch, pressed silken tofu)
- 500g (1lb) dates (Medjool are ideal)
- Twice as many almonds as you have dates
- 50g (2oz) dark chocolate (the darkest, bitterest, you can find)
- Edible flower petals if you can source them (some shops sell dried rose petals for this purpose)
Method
(we suggest you read everything at least once before doing anything)
1) Take the mascarpone and whisk (or blend) it with the coffee. What kind of coffee, you ask? Many will use instant coffee (1tbsp granules mixed with enough boiling water to dissolve it), and that is actually healthiest (counterintuitive but true) but if you care for flavor over health, and have the means to make espresso, make it ristretto (so, stop it halfway through filling up an espresso cup), let it cool, and use that. Absolute bonus for flavor (not for health): if you have the means to make Turkish coffee, use an equivalent amount of that (again, cooled).
You will now have coffee-flavoured mascarpone. It’s great for your gut and full of antioxidant polyphenols. Set it aside for the moment.
2) Take the dark chocolate and melt it. Please don’t microwave it or try to do it in a pan directly over the hob; instead, you will need to use a Bain-Marie. If you don’t have one made-for-purpose, you can place a metal or heatproof glass bowl in a saucepan, with something to stop it from touching the floor of the pan. Then boil water in the pan (without letting the water get into the bowl), and melt the chocolate in the bowl—this will allow you to melt it evenly without burning the chocolate.
You will now have melted dark chocolate. It has its own set of polyphenols, and is great for everything from the brain to the gut microbiome.
3) Cut the dates lengthways on one side and remove the stone. Stuff them carefully with the coffee-flavored mascarpone (you can use a teaspoon, or use a piping kit if you have one). Add a couple of almonds to each one. Place them all on a big plate, and drizzle the melted chocolate over them. Add the petals if you have them.
The dates and almonds deliver extra vitamins and minerals in abundance (not to mention, lots of fiber), and also are an amazing combination even just by themselves. With the mascarpone and chocolate added, this winning on new levels. We’re not done yet, though…
4) Chill them in the fridge for about 30 minutes.
Serve!
Learn more
For those interested in some of the science of what we have going on today:
- Make The Heart-Healthiest Coffee ← this is about cafestol content and why instant is heart-healthiest (alas)
- The Bitter Truth About Coffee (Or Is It) ← this is about the health benefits (and some risks, but mostly benefits) of coffee
- Why You Should Diversify Your Nuts ← almonds are a top-tier choice, but other nuts are good too! This recipe could work well with hazelnuts, for example (we wouldn’t call it “tiramisu crunch bites” in that case, though, since the flavor profile would change)
- Which Sugars Are Healthier, And Which Are Just The Same? ← for any worrying “aren’t dates sugary, though?”
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Yoga Nidra Made Easy – by Dr. Uma Dinsmore-Tuli and Nirlipta Tuli
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about yoga before, and about sleep. This one’s different.
It’s about a yogic practice that can be used to promote restful sleep—or just be a non-sleeping exercise that nonetheless promotes relaxation and recuperation.
While yoga nidra is as somatic as it is psychological, its corporeal aspects are all explored in a lying-down-on-one’s-back state. This isn’t a book of stretches and poses and such—those are great, but are simply not needed for this practice.
The authors explain, step-by-step, simply and clearly, how to practice yoga nidra, and get out of it what you want to (there are an assortment of possible outcomes, per your preference; there are options to choose along the way).
A lot of books about yoga, even when written in English, contain a lot of Sanskrit terms. This one doesn’t. And, that difference goes a long way to living up to the title of making this easy, for those of us who regrettably don’t read even transliterated Sanskrit.
Bottom line: if ever you struggle to relax, struggle to sleep, or struggle to find your get-up-and-go, this book provides all you need to engage in this very restorative practice!
Click here to check out Yoga Nidra Made Easy, and learn this restorative tool for yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Turkish Saffron Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Summer is upon us, and we need salad options. Coleslaw’s all well and good, until you’re the 4th person to bring it to the pot luck. Tzatziki’s great—and healthier than a standard coleslaw, being based in yogurt rather than mayonnaise as most Western coleslaws are (Eastern European coleslaws, for example, more often use a vinaigrette), but today our tastebuds are traveling to Turkey for this gut-healthy, phytochemical-rich, delicious dish.
You will need
- 12 oz carrots, cut into very thin batons (alternatively: use a peeler to peel it into super-thin strips)
- 2 oz chopped nuts (pistachios are traditional, almonds are also used sometimes; many other nuts would work too e.g. walnuts, hazelnuts, etc; not peanuts though)
- 2 cups kefir yogurt (if unavailable, substitute any 2 cups plain unsweetened yogurt; comparable plant yogurt is fine if you’re vegan; those healthy bacteria love plant yogurts as much as animal ones)
- 1 bulb garlic, grated
- 1 tsp chili flakes
- 1 pinch saffron, ground, then soaked in 1 tbsp warm water for a few hours
- 2 tbsp olive oil for cooking; ideally Extra Virgin, but at least Virgin
Method
(we suggest you read everything at least once before doing anything)
1) Put the olive oil and carrots into a saucepan and heat gently, stirring. You want to soften the carrots just a little and absorb the olive oil, without actually fully cooking the carrots; this will probably only take 2–3 minutes at most. Take it off the heat and transfer it to a bowl to cool.
When the mixture has cooled…
2) Add the kefir yogurt, garlic, chili flakes, and saffron water into the carrots, mixing thoroughly.
3) Add the chopped nuts as a garnish
(after mixing thoroughly, you will probably see more of the yogurt mixture and less of the carrots; that’s fine and correct))
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- The Many Health Benefits Of Garlic
- Capsaicin For Weight Loss And Against Inflammation
- Why You Should Diversify Your Nuts!
- Saffron For The Brain (& More) ← do not underestimate saffron’s neuroprotective qualities, and many other beneficial properties!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: