The Energy Plan – by James Collins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a lot of conflicting advice out there about how we should maintain our energy levels, for example:
- Eat fewer carbs!
- Eat more carbs!
- Eat slow-release carbs!
- Eat quick-release carbs!
- Practise intermittent fasting!
- Graze constantly throughout the day!
- Forget carbs and focus on fats!
- Actually it’s all about B-vitamins!
…and so on.
What Collins does differently is something much less-often seen:
Here, we’re advised on how to tailor our meals to our actual lifestyle, taking into account the day we actually have each day. For example:
- What will our energy needs be for the day?
- Will our needs be intense, or long, or both, or neither?
- What kind of recovery have we had, or do we need, from previous activities?
- Do we need to replace lost muscle glycogen, or are we looking to trim the fat?
- Are we doing a power-up or just maintenance today?
Rather than bidding us have a five-way spreadsheet and do advanced mathematics for every meal, though, Collins has done the hard work for us. The book explains the various principles in a casual format with a light conversational tone, and gives us general rules to follow.
These rules cover what to do for different times of day… and also, at different points in our life (the metabolic needs of a 13-year-old, 33-year-old, and 83-year-old, are very different!). That latter’s particularly handy, as a lot of books assume an age bracket for the reader, and this one doesn’t.
In short: a great book for anyone who wants to keep their energy levels up (throughout life’s ups and downs in activity) without piling on the pounds or starving oneself.
Click here to check out The Energy Plan on Amazon and fuel your days better!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Osteoporosis Breakthrough – by Dr. Doug Lucas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Osteoporosis” and “break” often don’t go well together, but here they do. So, what’s the breakthrough here?
There isn’t one, honestly. But if we overlook the marketing choices and focus on the book itself, the content here is genuinely good:
The book offers a comprehensive multivector approach to combatting osteoporosis, e.g:
- Diet
- Exercise
- Other lifestyle considerations
- Supplements
- Hormones
- Drugs
The author considers drugs a good and important tool for some people with osteoporosis, but not most. The majority of people, he considers, will do better without drugs—by tackling things more holistically.
The advice here is sound and covers all reasonable angles without getting hung up on the idea of there being a single magical solution for all.
Bottom line: if you’re looking for a book that’s a one-stop-shop for strategies against osteoporosis, this is a good option.
Click here to check out The Osteoporosis Breakthrough, and keep your bones strong!
Share This Post
-
Falling vaccination rates put children at risk of preventable diseases. Governments need a new strategy to boost uptake
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Child vaccination is one of the most cost-effective health interventions. It accounts for 40% of the global reduction in infant deaths since 1974 and has led to big health gains in Australia over the past two decades.
Australia has been a vaccination success story. Ten years after we begun mass vaccination against polio in 1956, it was virtually eliminated. Our child vaccination rates have been among the best in the world.
But after peaking in 2020, child vaccination in Australia is falling. Governments need to implement a comprehensive strategy to boost vaccine uptake, or risk exposing more children to potentially preventable infectious diseases.
Yuri A/Shutterstock Child vaccination has been a triumph
Thirty years ago, Australia’s childhood vaccination rates were dismal. Then, in 1997, governments introduced the National Immunisation Program to vaccinate children against diseases such as diphtheria, tetanus, and measles.
Measures to increase coverage included financial incentives for parents and doctors, a public awareness campaign, and collecting and sharing local data to encourage the least-vaccinated regions to catch up with the rest of the country.
What followed was a public health triumph. In 1995, only 52% of one-year-olds were fully immunised. By 2020, Australia had reached 95% coverage for one-year-olds and five-year-olds. At this level, it’s difficult even for highly infectious diseases, such as measles, to spread in the community, protecting both the vaccinated and unvaccinated.
By 2020, 95% of children were vaccinated. Drazen Zigic/Shutterstock Gaps between regions and communities closed too. In 1999, the Northern Territory’s vaccination rate for one-year-olds was the lowest in the country, lagging the national average by six percentage points. By 2020, that gap had virtually disappeared.
The difference between vaccination rates for First Nations children and other children also narrowed considerably.
It made children healthier. The years of healthy life lost due to vaccine-preventable diseases for children aged four and younger fell by nearly 40% in the decade to 2015.
Some diseases have even been eliminated in Australia.
Our success is slipping away
But that success is at risk. Since 2020, the share of children who are fully vaccinated has fallen every year. For every child vaccine on the National Immunisation Schedule, protection was lower in 2024 than in 2020.
Gaps between parts of Australia are opening back up. Vaccination rates in the highest-coverage parts of Australia are largely stable, but they are falling quickly in areas with lower vaccination.
In 2018, there were only ten communities where more than 10% of one-year-old children were not fully vaccinated. Last year, that number ballooned to 50 communities. That leaves more areas vulnerable to disease and outbreaks.
While Noosa, the Gold Coast Hinterland and Richmond Valley (near Byron Bay) have persistently had some of the country’s lowest vaccination rates, areas such as Manjimup in Western Australia and Tasmania’s South East Coast have recorded big declines since 2018.
Missing out on vaccination isn’t just a problem for children.
One preprint study (which is yet to be peer-reviewed) suggests vaccination during pregnancy may also be declining.
Far too many older Australians are missing out on recommended vaccinations for flu, COVID, pneumococcal and shingles. Vaccination rates in aged care homes for flu and COVID are worryingly low.
What’s going wrong?
Australia isn’t alone. Since the pandemic, child vaccination rates have fallen in many high-income countries, including New Zealand, the United Kingdom and the United States.
Globally, in 2023, measles cases rose by 20%, and just this year, a measles outbreak in rural Texas has put at least 13 children in hospital.
Alarmingly, some regions in Australia have lower measles vaccination than that Texas county.
The timing of trends here and overseas suggests things shifted, or at least accelerated, during the pandemic. Vaccine hesitancy, fuelled by misinformation about COVID vaccines, is a growing threat.
This year, vaccine sceptic Robert F. Kennedy Jr was appointed to run the US health system, and Louisiana’s top health official has reportedly cancelled the promotion of mass vaccination.
In Australia, a recent survey found 6% of parents didn’t think vaccines were safe, and 5% believed they don’t work.
Those concerns are far more common among parents with children who are partially vaccinated or unvaccinated. Among the 2% of parents whose children are unvaccinated, almost half believe vaccines are not safe for their child, and four in ten believe vaccines didn’t work.
Other consequences of the pandemic were a spike in the cost of living, and a health system struggling to meet demand. More than one in ten parents said cost and difficulty getting an appointment were barriers to vaccinating their children.
There’s no single cause of sliding vaccination rates, so there’s no one solution. The best way to reverse these worrying trends is to work on all the key barriers at once – from a lack of awareness, to inconvenience, to lack of trust.
What governments should do
Governments should step up public health campaigns that counter misinformation, boost awareness of immunisation and its benefits, and communicate effectively to low-vaccination groups. The new Australian Centre for Disease Control should lead the charge.
Primary health networks, the regional bodies responsible for improving primary care, should share data on vaccination rates with GPs and pharmacies. These networks should also help make services more accessible to communities who are missing out, such as migrant groups and disadvantaged families.
State and local governments should do the same, sharing data and providing support to make maternal child health services and school-based vaccination programs accessible for all families.
Governments can communicate better about the benefits of vaccination. Yuri A/Shutterstock Governments should also be more ambitious about tackling the growing vaccine divides between different parts of the country. The relevant performance measure in the national vaccination agreement is weak. States must only increase five-year-old vaccination rates in four of the ten areas where it is lowest. That only covers a small fraction of low-vaccination areas, and only the final stage of child vaccination.
Australia needs to set tougher goals, and back them with funding.
Governments should fund tailored interventions in areas with the lowest rates of vaccination. Proven initiatives include training trusted community members as “community champions” to promote vaccinations, and pop-up clinics or home visits for free vaccinations.
At this time of year, childcare centres and schools are back in full swing. But every year, each new intake has less protection than the previous cohort. Governments are developing a new national vaccination strategy and must seize the opportunity to turn that trend around. If it commits to a bold national plan, Australia can get back to setting records for child vaccination.
Peter Breadon, Program Director, Health and Aged Care, Grattan Institute and Wendy Hu, Associate, Health Program, Grattan Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
High Histamine Foods To Avoid (And Low Histamine Foods To Eat Instead)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nour Zibdeh is an Integrative and Functional Dietician, and she helps people overcome food intolerances. Today, it’s about getting rid of the underdiagnosed condition that is histamine intolerance, by first eliminating the triggers, and then not getting stuck on the low-histamine diet
The recommendations
High histamine foods to avoid include:
- Alcohol (all types)
- Fermented foods—normally great for the gut, but bad in this case
- That includes most cheeses and yogurts
- Aged, cured, or otherwise preserved meat
- Some plants, e.g. tomato, spinach, eggplant, banana, avocado. Again, normally all great, but not in this case.
Low histamine foods to eat include:
- Fruits and vegetables not mentioned above
- Minimally processed meat and fish, either fresh from the butcher/fishmonger, or frozen (not from the chilled food section of the supermarket), and eaten the same day they were purchased or defrosted, because otherwise histamine builds up over time (and quite quickly)
- Grains, but she recommends skipping gluten, given the high likelihood of a comorbid gluten intolerance. So instead she recommends for example quinoa, oats, rice, buckwheat, millet, etc.
For more about these (and more examples), as well as how to then phase safely off the low histamine diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
Food intolerances often gang up on a person (i.e., comorbidity is high), so you might also like to read about:
- Gluten: What’s The Truth?
- Fiber For FODMAP-Avoiders
- Foods For Managing Hypothyroidism (incl. Hashimoto’s)
- Crohn’s, Food Intolerances, & More
Take care!
Share This Post
Related Posts
-
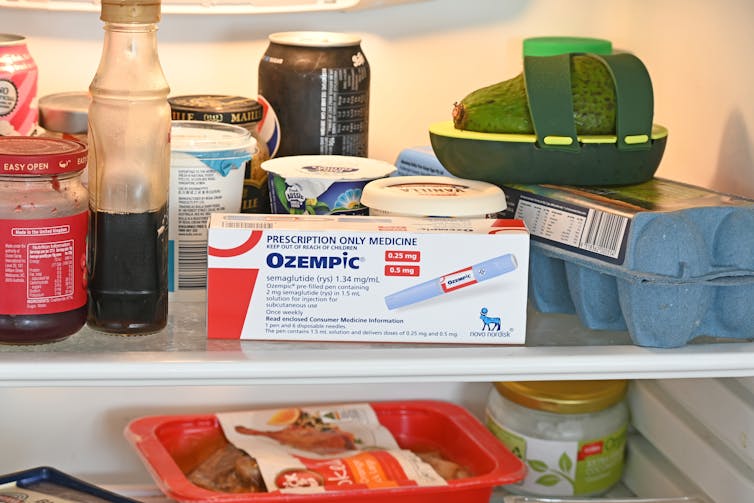
People on Ozempic may have fewer heart attacks, strokes and addictions – but more nausea, vomiting and stomach pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ozempic and Wegovy are increasingly available in Australia and worldwide to treat type 2 diabetes and obesity.
The dramatic effects of these drugs, known as GLP-1s, on weight loss have sparked huge public interest in this new treatment option.
However, the risks and benefits are still being actively studied.
In a new study in Nature Medicine, researchers from the United States reviewed health data from about 2.4 million people who have type 2 diabetes, including around 216,000 people who used a GLP-1 drug, between 2017 and 2023.
The researchers compared a range of health outcomes when GLP-1s were added to a person’s treatment plan, versus managing their diabetes in other ways, often using glucose-lowering medications.
Overall, they found people who used GLP-1s were less likely to experience 42 health conditions or adverse health events – but more likely to face 19 others.
myskin/Shutterstock What conditions were less common?
Cardiometabolic conditions
GLP-1 use was associated with fewer serious cardiovascular and coagulation disorders. This includes deep vein thrombosis, pulmonary embolism, stroke, cardiac arrest, heart failure and myocardial infarction.
Neurological and psychiatric conditions
GLP-1 use was associated with fewer reported substance use disorders or addictions, psychotic disorders and seizures.
Infectious conditions
GLP-1 use was associated with fewer bacterial infections and pneumonia.
What conditions were more common?
Gastrointestinal conditions
Consistent with prior studies, GLP-1 use was associated with gastrointestinal conditions such as nausea, vomiting, gastritis, diverticulitis and abdominal pain.
Other adverse effects
Increased risks were seen for conditions such as low blood pressure, syncope (fainting) and arthritis.
People who took Ozempic were more likely to experience stomach upsets than those who used other type 2 diabetes treatments. Douglas Cliff/Shutterstock How robust is this study?
The study used a large and reputable dataset from the US Department of Veterans Affairs. It’s an observational study, meaning the researchers tracked health outcomes over time without changing anyone’s treatment plan.
A strength of the study is it captures data from more than 2.4 million people across more than six years. This is much longer than what is typically feasible in an intervention study.
Observational studies like this are also thought to be more reflective of the “real world”, because participants aren’t asked to follow instructions to change their behaviour in unnatural or forced ways, as they are in intervention studies.
However, this study cannot say for sure that GLP-1 use was the cause of the change in risk of different health outcomes. Such conclusions can only be confidently made from tightly controlled intervention studies, where researchers actively change or control the treatment or behaviour.
The authors note the data used in this study comes from predominantly older, white men so the findings may not apply to other groups.
Also, the large number of participants means that even very small effects can be detected, but they might not actually make a real difference in overall population health.
Observational studies track outcomes over time, but can’t say what caused the changes. Jacob Lund/Shutterstock Other possible reasons for these links
Beyond the effect of GLP-1 in the body, other factors may explain some of the findings in this study. For example, it’s possible that:
- people who used GLP-1 could be more informed about treatment options and more motivated to manage their own health
- people who used GLP-1 may have received it because their health-care team were motivated to offer the latest treatment options, which could lead to better care in other areas that impact the risk of various health outcomes
- people who used GLP-1 may have been able to do so because they lived in metropolitan centres and could afford the medication, as well as other health-promoting services and products, such as gyms, mental health care, or healthy food delivery services.
Did the authors have any conflicts of interest?
Two of the study’s authors declared they were “uncompensated consultants” for Pfizer, a global pharmaceutical company known for developing a wide range of medicines and vaccines. While Pfizer does not currently make readily available GLP-1s such as Ozempic or Wegovy, they are attempting to develop their own GLP-1s, so may benefit from greater demand for these drugs.
This research was funded by the US Department of Veterans Affairs, a government agency that provides a wide range of services to military veterans.
No other competing interests were reported.
Diabetes vs weight-loss treatments
Overall, this study shows people with type 2 diabetes using GLP-1 medication generally have more positive health outcomes than negative health outcomes.
However, the study didn’t include people without type 2 diabetes. More research is needed to understand the effects of these medications in people without diabetes who are using them for other reasons, including weight loss.
While the findings highlight the therapeutic benefits of GLP-1 medications, they also raise important questions about how to manage the potential risks for those who choose to use this medication.
The findings of this study can help many people, including:
- policymakers looking at ways to make GLP-1 medications more widely available for people with various health conditions
- health professionals who have regular discussions with patients considering GLP-1 use
- individuals considering whether a GLP-1 medication is right for them.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Radishes vs Carrots – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing radishes to carrots, we picked the carrots.
Why?
In terms of macros, carrots have more fiber and carbs; the two root vegetables both have comparable (low) glycemic indices, so we’re saying that the one with more fiber wins, and that’s carrots.
In the category of vitamins, radishes have more of vitamins B9 and C, while carrots have more of vitamins A, B1, B2, B3, B5, B6, E, K, and choline. An easy win for carrots.
When it comes to minerals, radishes have more selenium, while carrots have more calcium, magnesium, manganese, phosphorus, and potassium. Another clear win for carrots.
In terms of polyphenols, radishes do have some, but carrots have more, and thus win this category too.
All in all, enjoy either or both, but carrots deliver the most nutrients by far!
Want to learn more?
You might like to read:
What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Circadian Rhythm: Far More Than Most People Know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Circadian Rhythm: Far More Than Most People Know
This is Dr. Satchidananda (Satchin) Panda, the scientist behind the discovery of the blue-light sensing cell type in the retina, and the many things it affects. But, he’s discovered more…
First, what you probably know (with a little more science)
Dr. Panda discovered that melanopsin, a photopigment, is “the primary candidate for photoreceptor-mediated entrainment”.
To put that in lay terms, it’s the brain’s go-to for knowing approximately what time of day or night it is, according to how much light there is (or isn’t), and how long it has (or hasn’t) been there.
But… the brain’s “go-to” isn’t the only method. By creating mice without melanopsin, he was able to find that they still keep a circadian rhythm, even in complete darkness:
Melanopsin (Opn4) Requirement for Normal Light-Induced Circadian Phase Shifting
In other words, it was a helpful, but not completely necessary, means of keeping a circadian rhythm.
So… What else is going on?
Dr. Panda and his team did a lot of science that is well beyond the scope of this main feature, but to give you an idea:
- With jargon: it explored the mechanisms and transcription translation negative feedback loops that regulate chronobiological processes, such as a histone lysine demathlyase 1a (JARID1a) that enhances Clock-Bmal1 transcription, and then used assorted genomic techniques to develop a model for how JARID1a works to moderate the level of Per transcription by regulating the transition between its repression and activation, and discovered that this heavily centered on hepatic gluconeogenesis and glucose homeostasis, facilitated by the protein cryptochrome regulating the fasting signal that occurs when glucagon binds to a G-protein coupled receptor, triggering CREB activation.
- Without jargon: a special protein tells our body how to respond to eating/fasting at different times of day—and conversely, certain physiological responses triggered by eating/fasting help us know what time of day it is.
- Simplest: our body keeps on its best cycle if we eat at the same time every day
This is important, because our circadian rhythm matters for a lot more than sleeping/waking! Take hormones, for example:
- Obvious hormones: testosterone and estrogen peak in the mornings around 9am, progesterone peaks between 10pm and 2am
- Forgotten hormones: cortisol peaks in the morning around 8:30am, melatonin peaks between 10pm and 2am
- More hormones: ghrelin (hunger hormone) peaks around 10am, leptin (satiety hormone) peaks 20 minutes after eating a certain amount of satiety-triggering food (protein does this most quickly), insulin is heavily tied to carbohydrate intake, but will still peak and trough according to when the body expects food.
What does this mean for us in practical terms?
For a start, it means that intermittent fasting can help guard against metabolic and related diseases (including inflammation, and thus also cancer, diabetes, arthritis, and more) a lot more if we practice it with our circadian rhythm in mind.
So that “8-hour window” for eating, that many intermittent fasting practitioners adhere to, is going to do much, much better if it’s 10am to 6pm, rather than, say, 4pm to midnight.
Additionally, Dr. Panda and his team found that a 12-hour eating window wasn’t sufficient to help significantly.
Some other take-aways:
- For reasons beyond the scope of this article, it’s good to exercise a) early b) before eating, so getting in some exercise between 8.30am and 10am is ideal
- It also means it’s beneficial to “front-load” eating, so a large breakfast at 10am, and smaller meals/snacks afterwards, is best.
- It also means that getting sunlight (even if cloud-covered) around 8.30am helps guard against metabolic disorders a lot, since the light remains the body’s go-to way of knowing the time.
- We realize that sunlight is not available at 8.30am at all latitudes at all times of year. Artificial is next-best.
- It also means sexual desire will typically peak in men in the mornings (per testosterone) and women in the evenings (per progesterone), but this is just an interesting bit of trivia, and not so relevant to metabolic health
What to do next…
Want to stabilize your own circadian rhythm in the best way, and also help Dr. Panda with his research?
His team’s (free!) app, “My Circadian Clock”, can help you track and organize all of the body’s measurable-by-you circadian events, and, if you give permission, will contribute to what will be the largest-yet human study into the topics covered today, to refine the conclusions and learn more about what works best.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: