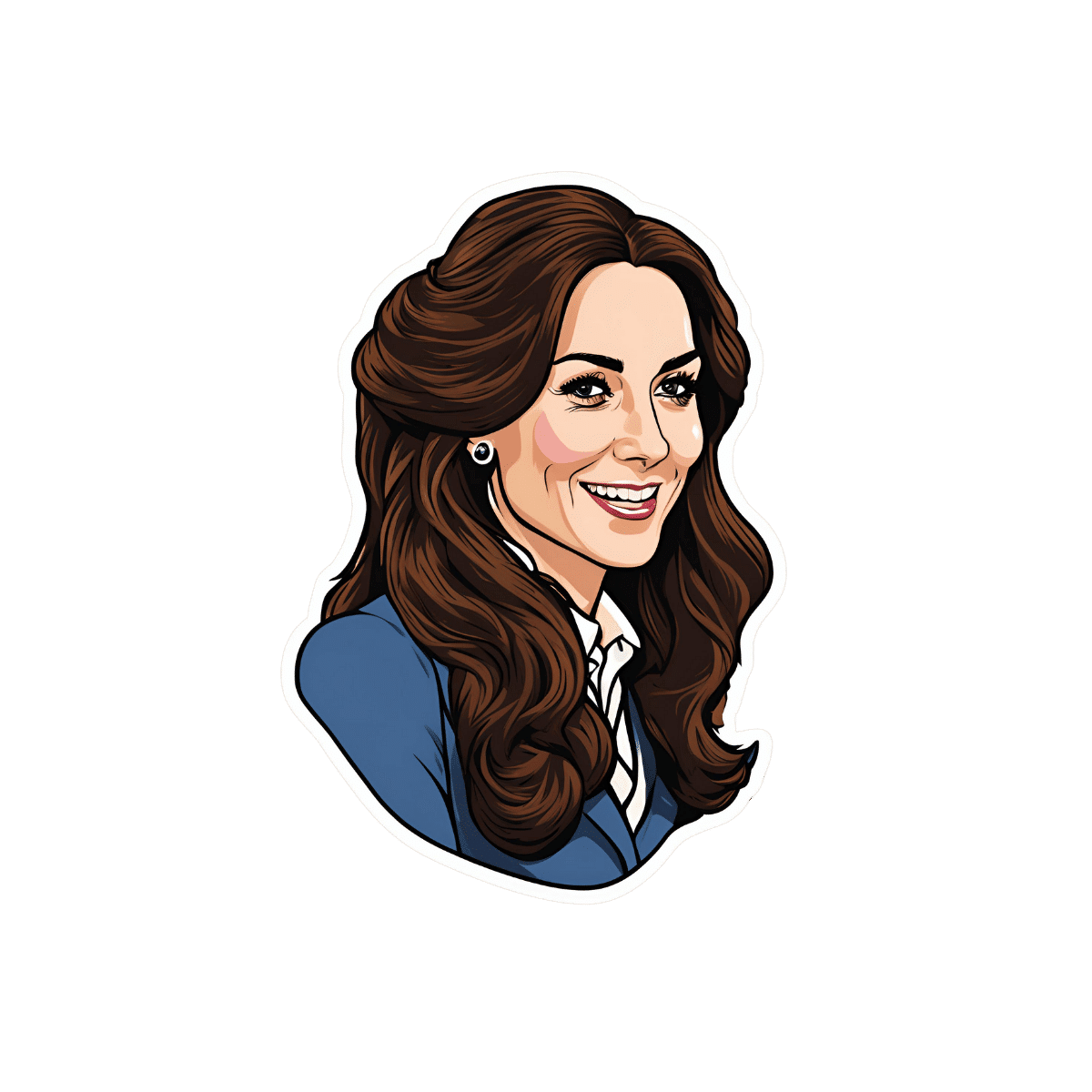
Eat To Beat Disease – by Dr. William W. Li
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all know that in principle, “food is medicine”… Or at least, that it can be. What we don’t always know is exactly what and why and how!
Dr Li outlines it for us in a clear and simple fashion that’s not just prescriptive, but also explanatory.
He starts with an overview of the body’s own systems for keeping itself in good working order, including:
- Angiogenesis
- Regeneration
- Microbiome
- DNA protection
- Immunity
When it comes to the framework of eating to beat disease—per the title—the principles map directly to the systems we just mentioned, thus:
- Starve your disease, feed your health
- (Re)generate your health
- Feed your inner ecosystem
- Direct your genetic fate
- Activate your immune command center
Thereafter, most of the rest of the book is given over to foods and food-related habits to promote all of the above, and how each works.
Lastly, he shares a lot of information about “food doses” because it’s all very well saying “eat cruciferous vegetables” or “eat these nuts”, but how much is enough? For that matter, how much is too much, if applicable? Where lies the difference between “make sure to eat some healthy fats” and “congratulations, you buttered your arteries”?
All this and more, Dr. Li explains for us in a clear and easy-reading fashion.
In short: this book is a great one-shot at reducing all-cause mortality and improving general health with food.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Stop Self-Sabotage – by Dr. Judy Ho
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of books of this genre identify one particular kind of self-sabotage, for example, they might pick one out of:
- Bad habits
- Limiting self-beliefs
- Poor goal-setting
- Procrastination
…etc, slap a quick fix on whatever they chose to focus on, and call it a day. Not so with Dr. Ho!
Here we have a much more comprehensive approach to tackling the problem of unintentional self-sabotage. With a multi-vector method, of which all angles can be improved simultaneously, it becomes much less like “whack-a-mole”… And much more like everything actually getting into order and staying that way.
The main approach here is CBT, but far beyond what most pop-psychology CBT books go for, with more techniques and resources.
On which note…
There are many great exercises that Dr. Ho recommends we do while reading… So you might want to get a nice notebook alongside this book if you don’t already have one! And what is more inspiring of optimism than a new notebook?
Bottom line: this is a great, well-organized guide to pruning the “why am I still doing this to myself?” aspects out of your life for a much more intentional, purposeful, effective way of living.
Click here to check it out on Amazon today, and stop sabotaging yourself!
Share This Post

Older, Faster, Stronger – by Margaret Webb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, now in her 60s, made it her mission in her 50s to become the best runner she could. Before that, she’d been a keen runner previously, but let things slip rather in her 40s. But the book’s not about her 40s, it’s about her 50s and onwards, and other female runners in their 50s, 60s, 70s, 80s, and even 90s.
There’s a lot of this book that’s about people’s individual stories, and those should certainly be enough to prompt almost any reader that “if they can do it, I can”.
A lot, meanwhile, is about health and exercise science, training methods, and what has worked for various later-life athletes, including the author. So, it’s also partway instruction manual, with plenty of reference to science and medical considerations too.
Bottom line: sometimes, life throws us challenges. Sometimes, the best response is “Yeah? Bet” and surprise everyone.
Click here to check out Older, Faster, Stronger, and become all those cool things!
Share This Post

The Worst Way to Wake Up (and What to Do Instead)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not everyone is naturally inclined to be a morning person, but there are things we can do to make things go more easily for our brains!
Cause for alarm?
Dr. Tracey Marks, psychiatrist, explains the impact of our first moments upon awakening, and what that can do to/for us in terms of sleep inertia (i.e. grogginess).
Sleep inertia is worse when waking from deep sleep—and notably, we don’t naturally wake directly from deep sleep unless we are externally aroused (e.g. by an alarm clock).
Dr. Marks suggests the use of more gradual alarms, including those with soft melodies, perhaps birdsong or other similarly gentle things (artificial sunlight alarms are also good), to ease our transition from sleeping to waking. It might take us a few minutes longer to be woken from sleep, but we’re not going to spend the next hour in a bleary-eyed stupor.
For more details on these things and more (including why not to hit “snooze”), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
Related Posts

Can kimchi really help you lose weight? Hold your pickle. The evidence isn’t looking great
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fermented foods have become popular in recent years, partly due to their perceived health benefits.
For instance, there is some evidence eating or drinking fermented foods can improve blood glucose control in people with diabetes. They can lower blood lipid (fats) levels and blood pressure in people with diabetes or obesity. Fermented foods can also improve diarrhoea symptoms.
But can they help you lose weight, as a recent study suggests? Let’s look at the evidence.
Remind me, what are fermented foods?
Fermented foods are ones prepared when microbes (bacteria and/or yeast) ferment (or digest) food components to form new foods. Examples include yoghurt, cheese, kefir, kombucha, wine, beer, sauerkraut and kimchi.
As a result of fermentation, the food becomes acidic, extending its shelf life (food-spoilage microbes are less likely to grow under these conditions). This makes fermentation one of the earliest forms of food processing.
Fermentation also leads to new nutrients being made. Beneficial microbes (probiotics) digest nutrients and components in the food to produce new bioactive components (postbiotics). These postbiotics are thought to contribute to the health benefits of the fermented foods, alongside the health benefits of the bacteria themselves.
What does the evidence say?
A study published last week has provided some preliminary evidence eating kimchi – the popular Korean fermented food – is associated with a lower risk of obesity in some instances. But there were mixed results.
The South Korean study involved 115,726 men and women aged 40-69 who reported how much kimchi they’d eaten over the previous year. The study was funded by the World Institute of Kimchi, which specialises in researching the country’s national dish.
Eating one to three servings of any type of kimchi a day was associated with a lower risk of obesity in men.
Men who ate more than three serves a day of cabbage kimchi (baechu) were less likely to have obesity and abdominal obesity (excess fat deposits around their middle). And women who ate two to three serves a day of baechu were less likely to have obesity and abdominal obesity.
Eating more radish kimchi (kkakdugi) was associated with less abdominal obesity in both men and women.
However, people who ate five or more serves of any type of kimchi weighed more, had a larger waist sizes and were more likely to be obese.
The study had limitations. The authors acknowledged the questionnaire they used may make it difficult to say exactly how much kimchi people actually ate.
The study also relied on people to report past eating habits. This may make it hard for them to accurately recall what they ate.
This study design can also only tell us if something is linked (kimchi and obesity), not if one thing causes another (if kimchi causes weight loss). So it is important to look at experimental studies where researchers make changes to people’s diets then look at the results.
How about evidence from experimental trials?
There have been several experimental studies looking at how much weight people lose after eating various types of fermented foods. Other studies looked at markers or measures of appetite, but not weight loss.
One study showed the stomach of men who drank 1.4 litres of fermented milk during a meal took longer to empty (compared to those who drank the same quantity of whole milk). This is related to feeling fuller for longer, potentially having less appetite for more food.
Another study showed drinking 200 millilitres of kefir (a small glass) reduced participants’ appetite after the meal, but only when the meal contained quickly-digested foods likely to make blood glucose levels rise rapidly. This study did not measure changes in weight.

Kefir, a fermented milk drink, reduced people’s appetite.
Ildi Papp/ShutterstockAnother study looked at Indonesian young women with obesity. Eating tempeh (a fermented soybean product) led to changes in an appetite hormone. But this did not impact their appetite or whether they felt full. Weight was not measured in this study.
A study in South Korea asked people to eat about 70g a day of chungkookjang (fermented soybean). There were improvements in some measures of obesity, including percentage body fat, lean body mass, waist-to-hip ratio and waist circumference in women. However there were no changes in weight for men or women.
A systematic review of all studies that looked at the impact of fermented foods on satiety (feeling full) showed no effect.
What should I do?
The evidence so far is very weak to support or recommend fermented foods for weight loss. These experimental studies have been short in length, and many did not report weight changes.
To date, most of the studies have used different fermented foods, so it is difficult to generalise across them all.
Nevertheless, fermented foods are still useful as part of a healthy, varied and balanced diet, particularly if you enjoy them. They are rich in healthy bacteria, and nutrients.
Are there downsides?
Some fermented foods, such as kimchi and sauerkraut, have added salt. The latest kimchi study said the average amount of kimchi South Koreans eat provides about 490mg of salt a day. For an Australian, this would represent about 50% of the suggested dietary target for optimal health.
Eating too much salt increases your risk of high blood pressure, heart disease and stroke.

Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Kate Middleton is having ‘preventive chemotherapy’ for cancer. What does this mean?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Catherine, Princess of Wales, is undergoing treatment for cancer. In a video thanking followers for their messages of support after her major abdominal surgery, the Princess of Wales explained, “tests after the operation found cancer had been present.”
“My medical team therefore advised that I should undergo a course of preventative chemotherapy and I am now in the early stages of that treatment,” she said in the two-minute video.
No further details have been released about the Princess of Wales’ treatment.
But many have been asking what preventive chemotherapy is and how effective it can be. Here’s what we know about this type of treatment.
It’s not the same as preventing cancer
To prevent cancer developing, lifestyle changes such as diet, exercise and sun protection are recommended.
Tamoxifen, a hormone therapy drug can be used to reduce the risk of cancer for some patients at high risk of breast cancer.
Aspirin can also be used for those at high risk of bowel and other cancers.
How can chemotherapy be used as preventive therapy?
In terms of treating cancer, prevention refers to giving chemotherapy after the cancer has been removed, to prevent the cancer from returning.
If a cancer is localised (limited to a certain part of the body) with no evidence on scans of it spreading to distant sites, local treatments such as surgery or radiotherapy can remove all of the cancer.
If, however, cancer is first detected after it has spread to distant parts of the body at diagnosis, clinicians use treatments such as chemotherapy (anti-cancer drugs), hormones or immunotherapy, which circulate around the body .
The other use for chemotherapy is to add it before or after surgery or radiotherapy, to prevent the primary cancer coming back. The surgery may have cured the cancer. However, in some cases, undetectable microscopic cells may have spread into the bloodstream to distant sites. This will result in the cancer returning, months or years later.
With some cancers, treatment with chemotherapy, given before or after the local surgery or radiotherapy, can kill those cells and prevent the cancer coming back.
If we can’t see these cells, how do we know that giving additional chemotherapy to prevent recurrence is effective? We’ve learnt this from clinical trials. Researchers have compared patients who had surgery only with those whose surgery was followed by additional (or often called adjuvant) chemotherapy. The additional therapy resulted in patients not relapsing and surviving longer.
How effective is preventive therapy?
The effectiveness of preventive therapy depends on the type of cancer and the type of chemotherapy.
Let’s consider the common example of bowel cancer, which is at high risk of returning after surgery because of its size or spread to local lymph glands. The first chemotherapy tested improved survival by 15%. With more intense chemotherapy, the chance of surviving six years is approaching 80%.
Preventive chemotherapy is usually given for three to six months.
How does chemotherapy work?
Many of the chemotherapy drugs stop cancer cells dividing by disrupting the DNA (genetic material) in the centre of the cells. To improve efficacy, drugs which work at different sites in the cell are given in combinations.
Chemotherapy is not selective for cancer cells. It kills any dividing cells.
But cancers consist of a higher proportion of dividing cells than the normal body cells. A greater proportion of the cancer is killed with each course of chemotherapy.
Normal cells can recover between courses, which are usually given three to four weeks apart.
What are the side effects?
The side effects of chemotherapy are usually reversible and are seen in parts of the body where there is normally a high turnover of cells.
The production of blood cells, for example, is temporarily disrupted. When your white blood cell count is low, there is an increased risk of infection.
Cell death in the lining of the gut leads to mouth ulcers, nausea and vomiting and bowel disturbance.
Certain drugs sometimes given during chemotherapy can attack other organs, such as causing numbness in the hands and feet.
There are also generalised symptoms such as fatigue.
Given that preventive chemotherapy given after surgery starts when there is no evidence of any cancer remaining after local surgery, patients can usually resume normal activities within weeks of completing the courses of chemotherapy.

Ian Olver, Adjunct Professsor, School of Psychology, Faculty of Health and Medical Sciences, University of Adelaide
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Are You Taking PIMs?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Getting Off The Overmedication Train
The older we get, the more likely we are to be on more medications. It’s easy to assume that this is because, much like the ailments they treat, we accumulate them over time. And superficially at least, that’s what happens.
And yet, almost half of people over 65 in Canada are taking “potentially inappropriate medications”, or PIMs—in other words, medications that are not needed and perhaps harmful. This categorization includes medications where the iatrogenic harms (side effects, risks) outweigh the benefits, and/or there’s a safer more effective medication available to do the job.
You may be wondering: what does this mean for the US?
Well, we don’t have the figures for the US because we’re working from Canadian research today, but given the differences between the two country’s healthcare systems (mostly socialized in Canada and mostly private in the US), it seems a fair hypothesis that if it’s almost half in Canada, it’s probably more than half in the US. Socialized healthcare systems are generally quite thrifty and seek to spend less on healthcare, while private healthcare systems are generally keen to upsell to new products/services.
The three top categories of PIMs according to the above study:
- Gabapentinoids (anticonvulsants also used to treat neuropathic pain)
- Proton pump inhibitors (PPIs)
- Antipsychotics (especially, to people without psychosis)
…but those are just the top of the list; there are many many more.
The list continues: opioids, anticholinergics, sulfonlyurea, NSAIDs, benzodiazepines and related rugs, and cholinesterase inhibitors. That’s where the Canadian study cuts off (although it also includes “others” just before NSAIDs), but still, you guessed it, there are more (we’re willing to bet statins weigh heavily in the “others” section, for a start).
There are two likely main causes of overmedication:
The side effect train
This is where a patient has a condition and is prescribed drug A, which has some undesired side effects, so the patient is prescribed drug B to treat those. However, that drug also has some unwanted side effects of its own, so the patient is prescribed drug C to treat those. And so on.
For a real-life rundown of how this can play out, check out the case study in:
The Hidden Complexities of Statins and Cardiovascular Disease (CVD)
The convenience factor
No, not convenient for you. Convenient for others. Convenient for the doctor if it gets you out of their office (socialized healthcare) or because it was easy to sell (private healthcare). Convenient for the staff in a hospital or other care facility.
This latter is what happens when, for example, a patient is being too much trouble, so the staff give them promazine “to help them settle down”, notwithstanding that promazine is, besides being a sedative, also an antipsychotic whose common side effects include amenorrhea, arrhythmias, constipation, drowsiness and dizziness, dry mouth, impotence, tiredness, galactorrhoea, gynecomastia, hyperglycemia, insomnia, hypotension, seizures, tremor, vomiting and weight gain.
This kind of thing (and worse) happens more often towards the end of a patient’s life; indeed, sometimes precipitating that end, whether you want it or not:
Mortality, Palliative Care, & Euthanasia
How to avoid it
Good practice is to be “open-mindedly skeptical” about any medication. By this we mean, don’t reject it out of hand, but do ask questions about it.
Ask your prescriber not only what it’s for and what it’ll do, but also what the side effects and risks are, and an important question that many people don’t think to ask, and for which doctors thus don’t often have a well-prepared smooth-selling reply, “what will happen if I don’t take this?”
And look up unbiased neutral information about it, from reliable sources (Drugs.com and The BNF are good reference guides for this—and if it’s important to you, check both, in case of any disagreement, as they function under completely different regulatory bodies, the former being American and the latter being British. So if they both agree, it’s surely accurate, according to best current science).
Also: when you are on a medication, keep a journal of your symptoms, as well as a log of your vitals (heart rate, blood pressure, weight, sleep etc) so you know what the medication seems to be helping or harming, and be sure to have a regular meds review with your doctor to check everything’s still right for you. And don’t be afraid to seek a second opinion if you still have doubts.
Want to know more?
For a more in-depth exploration than we have room for here, check out this book that we reviewed not long back:
To Medicate or Not? That is the Question! – by Dr. Asha Bohannon
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: