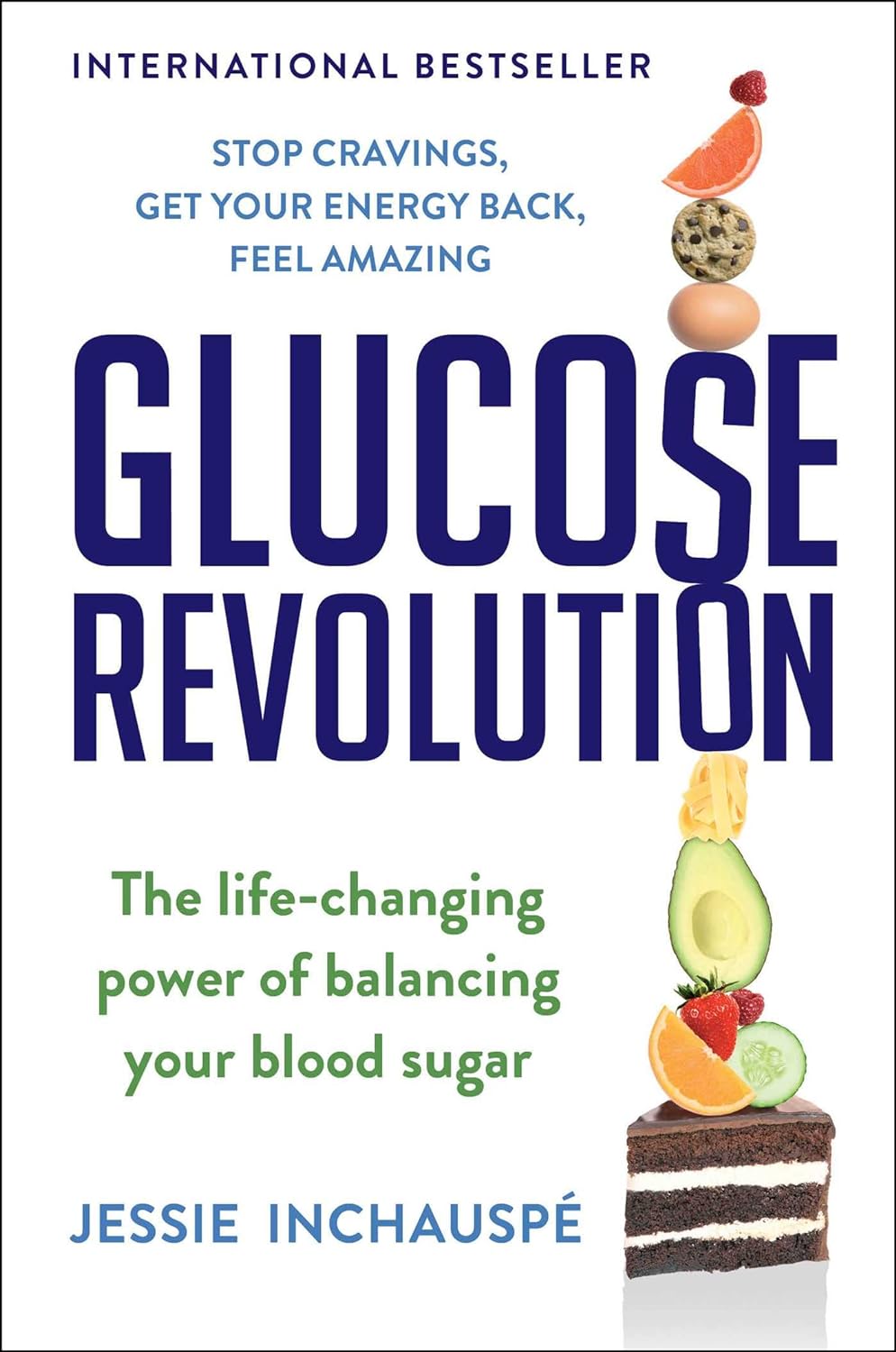
Glucose Revolution – by Jessie Inchauspé
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While we all know that keeping balanced blood sugars is important for all us (be we diabetic, pre-diabetic, or not at all), it can be a mystifying topic!
Beyond a generic “sugar is bad”…
- What does it all mean and how does it all work?
- Should we go low-carb?
- What’s the deal with fruit?
- Carbs or protein for breakfast?
- Is “quick energy” ever a good thing?
- How do starches weigh in again?
It’s all so confusing!
Happily, Jessie Inchauspé has the incredible trifecta of qualifications to help us: she’s a biochemist, a keen cook, and a great educator. What we mean by this latter is:
Instead of dry textbook explanations, or “trust me” hand-waives, she explains biochemistry in a clear, simple, digestible (if you’ll pardon the pun) way with very helpful diagrams what things cause (or flatten) blood sugar spikes and how and why. If you read this book, you will understand, without guesswork or gaps, exactly what is happening on a physical level, and why and how her “10 hacks” work.
Her “10 hacks” are explained so thoroughly that each gets a chapter of its own, but we’ll not keep them a mystery from you meanwhile, they are:
- Eat foods in the right order
- Add a green starter to your meals
- Stop counting calories
- Flatten your breakfast curve
- Have any type of sugar you like—they’re all the same
- Pick dessert over a sweet snack
- Reach for the vinegar before you eat
- After you eat, move
- If you have to snack, go savoury
- Put some clothes on your carbs
She then finishes up with a collection of handy cheat-sheets and some of her own recipes.
Bottom line: this isn’t just a “how-to” book. It gives the how-to, yes, but it also gives such good explanations that you’ll never be confused again by what’s going on in your glucose-related health.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Anxiety Attack vs Panic Attack: Do You Know The Difference?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The terms are sometimes used incorrectly, but have quite different meanings. Dr. Julie Smith, psychologist, explains in this short video:
Important distinctions
Anxiety attacks are not clinically recognized terms and lack a clear definition, often used to describe a build-up of anxiety before anticipated stressful events (e.g. social gatherings, medical appointments, etc, though of course what it is will vary from person to person—not everyone finds the same things stressful, or has the same kinds of anticipations around things).
Panic attacks, in contrast, are sudden surges of intense fear or discomfort that peak within minutes. They are characterized by symptoms including at least 4 of:
- palpitations
- sweating
- shortness of breath
- chest pain
- dizziness
- fear of losing control or dying
There’s a misconception that panic attacks never have identifiable triggers while anxiety attacks always do.
In reality, both can occur with or without a clear cause. Panic attacks can arise from various conditions, including trauma, OCD, or phobias, and don’t necessarily mean you have a panic disorder. They can also occur as a drug response, without any known underlying psychological condition.
You may also notice that that list of symptoms has quite a bit of overlap with the symptoms of a heart attack, which a) does not help people to calm down b) can, on the flipside, cause a heart attack to be misdiagnosed as a panic attack.
In terms of management:
- In the moment: breathing exercises, like extending your exhalation (a common example is the “7-11” method, inhaling for 7 seconds and exhaling for 11 seconds), can calm the body and reduce panic symptoms.
- More generally: to prevent panic attacks from becoming more frequent, avoid avoiding safe environments that triggered an attack, like supermarkets or social gatherings. Gradual exposure helps reduce anxiety over time, while avoidance can worsen it.
If panic attacks persist, Dr. Smith advises to seek help from a doctor or psychologist to understand their root causes and develop effective coping strategies.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
It’s Not A Bloody Trend – by Kat Brown
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one’s not a clinical book, and the author is not a clinician. However, it’s not just a personal account, either. Kat Brown is an award-winning journalist (with ADHD) and has approached this journalistically.
Not just in terms of investigative journalism, either. Rather, also with her knowledge and understanding of the industry, doing for us some meta-journalism and explaining why the press have gone for many misleading headlines.
Which in this case means for example it’s not newsworthy to say that people have gone undiagnosed and untreated for years and that many continue to go unseen; we know this also about such things as endometriosis, adenomyosis, and PCOS. But some more reactionary headlines will always get attention, e.g. “look at these malingering attention-seekers”.
She also digs into the common comorbidities of various conditions, the differences it makes to friendships, families, relationships, work, self-esteem, parenting, and more.
This isn’t a “how to” book, but there’s a lot of value here if a) you have ADHD, and/or b) you spend any amount of time with someone who does.
Bottom line: if you’d like to understand “what all the fuss is about” in one book, this is the one for ADHD.
Share This Post
-
The Power of Self-Care – by Dr. Sunil Kumar
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is mostly not about: bubble baths and scented candles. We say “mostly”, because stress management is an important aspect given worthy treatment in this book, but there is more emphasis on evidence-based interventions and thus Dr. Kumar is readier to prescribe nature walks and meditation, than product-based pampering sessions.
As is made clear in the subtitle “Transforming Heart Health with Lifestyle Medicine”, the focus is on heart health throughout, but as 10almonds readers know, “what’s good for your heart is good for your brain” is a truism that indeed holds true here too.
Dr. Kumar also gives nutritional tweaks to optimize heart health, and includes a selection of heart-healthy recipes, too. And exercise? Yes, customizable exercise plans, even. And a plan for getting sleep into order if perchance it has got a bit out of hand (most people get less sleep than necessary for maintenance of good health), and he even delves into “social prescribing”, that is to say, making sure that one’s social connectedness does not get neglected—without letting it, conversely, take over too much of one’s life (done badly, social connectedness can be a big source of unmanaged stress).
Perhaps the most value of this book comes from its 10-week self-care plan (again, with a focus on heart health), basically taking the reader by the hand for long enough that, after those 10 weeks, habits should be quite well-ingrained.
A strong idea throughout is that the things we take up should be sustainable, because well, a heart is for life, not just for a weekend retreat.
Bottom line: if you’d like to improve your heart health in a way that feels like self-care rather than an undue amount of work, then this is the book for you.
Share This Post
Related Posts
-
What will aged care look like for the next generation? More of the same but higher out-of-pocket costs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aged care financing is a vexed problem for the Australian government. It is already underfunded for the quality the community expects, and costs will increase dramatically. There are also significant concerns about the complexity of the system.
In 2021–22 the federal government spent A$25 billion on aged services for around 1.2 million people aged 65 and over. Around 60% went to residential care (190,000 people) and one-third to home care (one million people).
The final report from the government’s Aged Care Taskforce, which has been reviewing funding options, estimates the number of people who will need services is likely to grow to more than two million over the next 20 years. Costs are therefore likely to more than double.
The taskforce has considered what aged care services are reasonable and necessary and made recommendations to the government about how they can be paid for. This includes getting aged care users to pay for more of their care.
But rather than recommending an alternative financing arrangement that will safeguard Australians’ aged care services into the future, the taskforce largely recommends tidying up existing arrangements and keeping the status quo.
No Medicare-style levy
The taskforce rejected the aged care royal commission’s recommendation to introduce a levy to meet aged care cost increases. A 1% levy, similar to the Medicare levy, could have raised around $8 billion a year.
The taskforce failed to consider the mix of taxation, personal contributions and social insurance which are commonly used to fund aged care systems internationally. The Japanese system, for example, is financed by long-term insurance paid by those aged 40 and over, plus general taxation and a small copayment.
Instead, the taskforce puts forward a simple, pragmatic argument that older people are becoming wealthier through superannuation, there is a cost of living crisis for younger people and therefore older people should be required to pay more of their aged care costs.
Separating care from other services
In deciding what older people should pay more for, the taskforce divided services into care, everyday living and accommodation.
The taskforce thought the most important services were clinical services (including nursing and allied health) and these should be the main responsibility of government funding. Personal care, including showering and dressing were seen as a middle tier that is likely to attract some co-payment, despite these services often being necessary to maintain independence.
The task force recommended the costs for everyday living (such as food and utilities) and accommodation expenses (such as rent) should increasingly be a personal responsibility.
Aged care users will pay more of their share for cooking and cleaning.
Lizelle Lotter/ShutterstockMaking the system fairer
The taskforce thought it was unfair people in residential care were making substantial contributions for their everyday living expenses (about 25%) and those receiving home care weren’t (about 5%). This is, in part, because home care has always had a muddled set of rules about user co-payments.
But the taskforce provided no analysis of accommodation costs (such as utilities and maintenance) people meet at home compared with residential care.
To address the inefficiencies of upfront daily fees for packages, the taskforce recommends means testing co-payments for home care packages and basing them on the actual level of service users receive for everyday support (for food, cleaning, and so on) and to a lesser extent for support to maintain independence.
It is unclear whether clinical and personal care costs and user contributions will be treated the same for residential and home care.
Making residential aged care sustainable
The taskforce was concerned residential care operators were losing $4 per resident day on “hotel” (accommodation services) and everyday living costs.
The taskforce recommends means tested user contributions for room services and everyday living costs be increased.
It also recommends that wealthier older people be given more choice by allowing them to pay more (per resident day) for better amenities. This would allow providers to fully meet the cost of these services.
Effectively, this means daily living charges for residents are too low and inflexible and that fees would go up, although the taskforce was clear that low-income residents should be protected.
Moving from buying to renting rooms
Currently older people who need residential care have a choice of making a refundable up-front payment for their room or to pay rent to offset the loans providers take out to build facilities. Providers raise capital to build aged care facilities through equity or loan financing.
However, the taskforce did not consider the overall efficiency of the private capital market for financing aged care or alternative solutions.
Instead, it recommended capital contributions be streamlined and simplified by phasing out up-front payments and focusing on rental contributions. This echoes the royal commission, which found rent to be a more efficient and less risky method of financing capital for aged care in private capital markets.
It’s likely that in a decade or so, once the new home care arrangements are in place, there will be proportionally fewer older people in residential aged care. Those who do go are likely to be more disabled and have greater care needs. And those with more money will pay more for their accommodation and everyday living arrangements. But they may have more choice too.
Although the federal government has ruled out an aged care levy and changes to assets test on the family home, it has yet to respond to the majority of the recommendations. But given the aged care minister chaired the taskforce, it’s likely to provide a good indication of current thinking.
Hal Swerissen, Emeritus Professor, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Leverage Attachment Theory In Your Relationship
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Leverage Attachment Theory In Your Relationship
Attachment theory has come to be seen in “kids nowadays”’ TikTok circles as almost a sort of astrology, but that’s not what it was intended for, and there’s really nothing esoteric about it.
What it can be, is a (fairly simple, but) powerful tool to understand about our relationships with each other.
To demystify it, let’s start with a little history…
Attachment theory was conceived by developmental psychologist Mary Ainsworth, and popularized as a theory bypsychiatrist John Bowlby. The two would later become research partners.
- Dr. Ainsworth’s initial work focused on children having different attachment styles when it came to their caregivers: secure, avoidant, or anxious.
- Later, she would add a fourth attachment style: disorganized, and then subdivisions, such as anxious-avoidant and dismissive-avoidant.
- Much later, the theory would be extended to attachments in (and between) adults.
What does it all mean?
To understand this, we must first talk about “The Strange Situation”.
“The Strange Situation” was an experiment conducted by Dr. Ainsworth, in which a child would be observed playing, while caregivers and strangers would periodically arrive and leave, recreating a natural environment of most children’s lives. Each child’s different reactions were recorded, especially noting:
- The child’s reaction (if any) to their caregiver’s departure
- The child’s reaction (if any) to the stranger’s presence
- The child’s reaction (if any) to their caregiver’s return
- The child’s behavior on play, specifically, how much or little the child explored and played with new toys
She observed different attachment styles, including:
- Secure: a securely attached child would play freely, using the caregiver as a secure base from which to explore. Will engage with the stranger when the caregiver is also present. May become upset when the caregiver leaves, and happy when they return.
- Avoidant: an avoidantly attached child will not explore much regardless of who is there; will not care much when the caregiver departs or returns.
- Anxious: an anxiously attached child may be clingy before separation, helplessly passive when the caregiver is absent, and difficult to comfort upon the caregiver’s return.
- Disorganized: a disorganizedly attached child may flit between the above types
These attachment styles were generally reflective of the parenting styles of the respective caregivers:
- If a caregiver was reliably present (physically and emotionally), the child would learn to expect that and feel secure about it.
- If a caregiver was absent a lot (physically and/or emotionally), the child would learn to give up on expecting a caregiver to give care.
- If a caregiver was unpredictable a lot in presence (physical and/or emotional), the child would become anxious and/or confused about whether the caregiver would give care.
What does this mean for us as adults?
As we learn when we are children, tends to go for us in life. We can change, but we usually don’t. And while we (usually) no longer rely on caregivers per se as adults, we do rely (or not!) on our partners, friends, and so forth. Let’s look at it in terms of partners:
- A securely attached adult will trust that their partner loves them and will be there for them if necessary. They may miss their partner when absent, but won’t be anxious about it and will look forward to their return.
- An avoidantly attached adult will not assume their partner’s love, and will feel their partner might let them down at any time. To protect themself, they may try to manage their own expectations, and strive always to keep their independence, to make sure that if the worst happens, they’ll still be ok by themself.
- An anxiously attached adult will tend towards clinginess, and try to keep their partner’s attention and commitment by any means necessary.
Which means…
- When both partners have secure attachment styles, most things go swimmingly, and indeed, securely attached partners most often end up with each other.
- A very common pairing, however, is one anxious partner dating one avoidant partner. This happens because the avoidant partner looks like a tower of strength, which the anxious partner needs. The anxious partner’s clinginess can also help the avoidant partner feel better about themself (bearing in mind, the avoidant partner almost certainly grew up feeling deeply unwanted).
- Anxious-anxious pairings happen less because anxiously attached people don’t tend to be attracted to people who are in the same boat.
- Avoidant-avoidant pairings happen least of all, because avoidantly attached people having nothing to bind them together. Iff they even get together in the first place, then later when trouble hits, one will propose breaking up, and the other will say “ok, bye”.
This is fascinating, but is there a practical use for this knowledge?
Yes! Understanding our own attachment styles, and those around us, helps us understand why we/they act a certain way, and realize what relational need is or isn’t being met, and react accordingly.
That sometimes, an anxiously attached person just needs some reassurance:
- “I love you”
- “I miss you”
- “I look forward to seeing you later”
That sometimes, an avoidantly attached person needs exactly the right amount of space:
- Give them too little space, and they will feel their independence slipping, and yearn to break free
- Give them too much space, and oops, they’re gone now
Maybe you’re reading that and thinking “won’t that make their anxious partner anxious?” and yes, yes it will. That’s why the avoidant partner needs to skip back up and remember to do the reassurance.
It helps also when either partner is going to be away (physically or emotionally! This counts the same for if a partner will just be preoccupied for a while), that they parameter that, for example:
- Not: “Don’t worry, I just need some space for now, that’s all” (à la “I am just going outside and may be some time“)
- But: “I need to be undisturbed for a bit, but let’s schedule some me-and-you-time for [specific scheduled time]”.
Want to learn more about addressing attachment issues?
Psychology Today: Ten Ways to Heal Your Attachment Issues
You also might enjoy such articles such as:
- Nurturing secure attachment: building healthy relationships
- Why anxious and avoidant often attracted each other
- How to help an insecurely attached partner feel loved
- How to cope with a dismissive-avoidant partner
Lastly, to end on a light note…
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
WHO Overturns Dogma on Airborne Disease Spread. The CDC Might Not Act on It.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The World Health Organization has issued a report that transforms how the world understands respiratory infections like covid-19, influenza, and measles.
Motivated by grave missteps in the pandemic, the WHO convened about 50 experts in virology, epidemiology, aerosol science, and bioengineering, among other specialties, who spent two years poring through the evidence on how airborne viruses and bacteria spread.
However, the WHO report stops short of prescribing actions that governments, hospitals, and the public should take in response. It remains to be seen how the Centers for Disease Control and Prevention will act on this information in its own guidance for infection control in health care settings.
The WHO concluded that airborne transmission occurs as sick people exhale pathogens that remain suspended in the air, contained in tiny particles of saliva and mucus that are inhaled by others.
While it may seem obvious, and some researchers have pushed for this acknowledgment for more than a decade, an alternative dogma persisted — which kept health authorities from saying that covid was airborne for many months into the pandemic.
Specifically, they relied on a traditional notion that respiratory viruses spread mainly through droplets spewed out of an infected person’s nose or mouth. These droplets infect others by landing directly in their mouth, nose, or eyes — or they get carried into these orifices on droplet-contaminated fingers. Although these routes of transmission still happen, particularly among young children, experts have concluded that many respiratory infections spread as people simply breathe in virus-laden air.
“This is a complete U-turn,” said Julian Tang, a clinical virologist at the University of Leicester in the United Kingdom, who advised the WHO on the report. He also helped the agency create an online tool to assess the risk of airborne transmission indoors.
Peg Seminario, an occupational health and safety specialist in Bethesda, Maryland, welcomed the shift after years of resistance from health authorities. “The dogma that droplets are a major mode of transmission is the ‘flat Earth’ position now,” she said. “Hurray! We are finally recognizing that the world is round.”
The change puts fresh emphasis on the need to improve ventilation indoors and stockpile quality face masks before the next airborne disease explodes. Far from a remote possibility, measles is on the rise this year and the H5N1 bird flu is spreading among cattle in several states. Scientists worry that as the H5N1 virus spends more time in mammals, it could evolve to more easily infect people and spread among them through the air.
Traditional beliefs on droplet transmission help explain why the WHO and the CDC focused so acutely on hand-washing and surface-cleaning at the beginning of the pandemic. Such advice overwhelmed recommendations for N95 masks that filter out most virus-laden particles suspended in the air. Employers denied many health care workers access to N95s, insisting that only those routinely working within feet of covid patients needed them. More than 3,600 health care workers died in the first year of the pandemic, many due to a lack of protection.
However, a committee advising the CDC appears poised to brush aside the updated science when it comes to its pending guidance on health care facilities.
Lisa Brosseau, an aerosol expert and a consultant at the Center for Infectious Disease Research and Policy in Minnesota, warns of a repeat of 2020 if that happens.
“The rubber hits the road when you make decisions on how to protect people,” Brosseau said. “Aerosol scientists may see this report as a big win because they think everything will now follow from the science. But that’s not how this works and there are still major barriers.”
Money is one. If a respiratory disease spreads through inhalation, it means that people can lower their risk of infection indoors through sometimes costly methods to clean the air, such as mechanical ventilation and using air purifiers, and wearing an N95 mask. The CDC has so far been reluctant to press for such measures, as it updates foundational guidelines on curbing airborne infections in hospitals, nursing homes, prisons, and other facilities that provide health care. This year, a committee advising the CDC released a draft guidance that differs significantly from the WHO report.
Whereas the WHO report doesn’t characterize airborne viruses and bacteria as traveling short distances or long, the CDC draft maintains those traditional categories. It prescribes looser-fitting surgical masks rather than N95s for pathogens that “spread predominantly over short distances.” Surgical masks block far fewer airborne virus particles than N95s, which cost roughly 10 times as much.
Researchers and health care workers have been outraged about the committee’s draft, filing letters and petitions to the CDC. They say it gets the science wrong and endangers health. “A separation between short- and long-range distance is totally artificial,” Tang said.
Airborne viruses travel much like cigarette smoke, he explained. The scent will be strongest beside a smoker, but those farther away will inhale more and more smoke if they remain in the room, especially when there’s no ventilation.
Likewise, people open windows when they burn toast so that smoke dissipates before filling the kitchen and setting off an alarm. “You think viruses stop after 3 feet and drop to the ground?” Tang said of the classical notion of distance. “That is absurd.”
The CDC’s advisory committee is comprised primarily of infection control researchers at large hospital systems, while the WHO consulted a diverse group of scientists looking at many different types of studies. For example, one analysis examined the puff clouds expelled by singers, and musicians playing clarinets, French horns, saxophones, and trumpets. Another reviewed 16 investigations into covid outbreaks at restaurants, a gym, a food processing factory, and other venues, finding that insufficient ventilation probably made them worse than they would otherwise be.
In response to the outcry, the CDC returned the draft to its committee for review, asking it to reconsider its advice. Meetings from an expanded working group have since been held privately. But the National Nurses United union obtained notes of the conversations through a public records request to the agency. The records suggest a push for more lax protection. “It may be difficult as far as compliance is concerned to not have surgical masks as an option,” said one unidentified member, according to notes from the committee’s March 14 discussion. Another warned that “supply and compliance would be difficult.”
The nurses’ union, far from echoing such concerns, wrote on its website, “The Work Group has prioritized employer costs and profits (often under the umbrella of ‘feasibility’ and ‘flexibility’) over robust protections.” Jane Thomason, the union’s lead industrial hygienist, said the meeting records suggest the CDC group is working backward, molding its definitions of airborne transmission to fit the outcome it prefers.
Tang expects resistance to the WHO report. “Infection control people who have built their careers on this will object,” he said. “It takes a long time to change people’s way of thinking.”
The CDC declined to comment on how the WHO’s shift might influence its final policies on infection control in health facilities, which might not be completed this year. Creating policies to protect people from inhaling airborne viruses is complicated by the number of factors that influence how they spread indoors, such as ventilation, temperature, and the size of the space.
Adding to the complexity, policymakers must weigh the toll of various ailments, ranging from covid to colds to tuberculosis, against the burden of protection. And tolls often depend on context, such as whether an outbreak happens in a school or a cancer ward.
“What is the level of mortality that people will accept without precautions?” Tang said. “That’s another question.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: