Whole – by Dr. T. Colin Campbell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us have at least a broad idea of what we’re supposed to be eating, what nutrients we should be getting. Many of us look at labels, and try to get our daily dose of this and that and the other.
And what we don’t get from food? There are supplements.
Dr. Campbell thinks we can do better:
Perhaps most critical in this book, where it stands out from others (we may already know, for example, that we should try to eat diverse plants and whole foods) is its treatment of why many supplements aren’t helpful.
We tend to hear “supplements are a waste of money” and sometimes they are, sometimes they aren’t. How to know the difference?
Key: things directly made from whole food sources will tend to be better. Seems reasonable, but… why? The answer lies in what else those foods contain. An apple may contain a small amount of vitamin C, less than a vitamin C tablet, but also contains a whole host of other things—tiny phytonutrients, whose machinations are mostly still mysteries to us—that go with that vitamin C and help it work much better. Lab-made supplements won’t have those.
There’s a lot more to the book… A chunk of which is a damning critique of the US healthcare system (the author argues it would be better named a sicknesscare system). We also learn about getting a good balance of macro- and micronutrients from our diet rather than having to supplement so much.
The style is conversational, while not skimping on the science. The author has had more than 150 papers published in peer-reviewed journals, and is no stranger to the relevant academia. Here, however, he focuses on making things easily comprehensible to the lay reader.
In short: if you’ve ever wondered how you’re doing at getting a good nutritional profile, and how you could do better, this is definitely the book for you.
Click here to check out “Whole” on Amazon today, and level up your daily diet!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
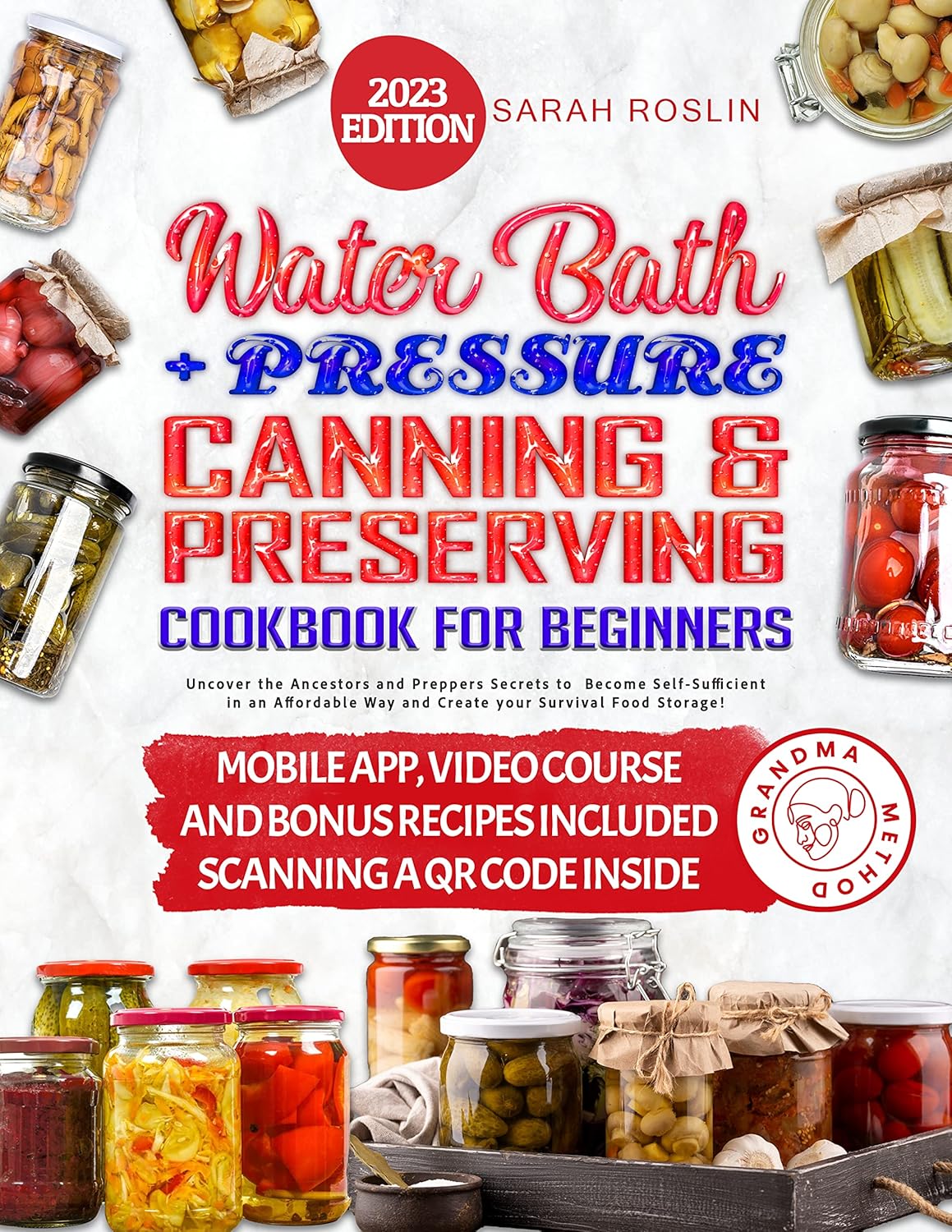
Water Bath + More Cookbook for Beginners – by Sarah Roslin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether you want to be prepared for the next major crisis that shuts down food supply chains, or just learn a new skill, this book provides the tools!
Especially beneficial if you also grow your own vegetables, but even you just buy those… Home-canned food is healthy, contains fewer additives and preservatives, and costs less in the long run.
Roslin teaches an array of methods, including most importantly:
- fermentation and pickling
- water bath canning, and
- pressure canning.
As for what’s inside? She covers not just vegetables, but also fruit, seafood, meat… Basically, anything that can be canned.
The book explains the tools and equipment you will need as well as how to perform it safely—as well as common mistakes to avoid!
Lest we be intimidated by the task of acquiring appropriate equipment, she also walks us through what we’ll need in that regard too!
Last but not least, there’s also a (sizeable) collection of simple, step-by-step recipes, catering to a wide variety of tastes.
Bottom line: a highly valuable resource that we recommend heartily.
Share This Post
-
In This Oklahoma Town, Most Everyone Knows Someone Who’s Been Sued by the Hospital
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
McALESTER, Okla. — It took little more than an hour for Deborah Hackler to dispense with the tall stack of debt collection lawsuits that McAlester Regional Medical Center recently brought to small-claims court in this Oklahoma farm community.
Hackler, a lawyer who sues patients on behalf of the hospital, buzzed through 51 cases, all but a handful uncontested, as is often the case. She bantered with the judge as she secured nearly $40,000 in judgments, plus 10% in fees for herself, according to court records.
It’s a payday the hospital and Hackler have shared frequently over the past three decades, records show. The records indicate McAlester Regional Medical Center and an affiliated clinic have filed close to 5,000 debt collection cases since the early 1990s, most often represented by the father-daughter law firm of Hackler & Hackler.
Some of McAlester’s 18,000 residents have been taken to court multiple times. A deputy at the county jail and her adult son were each sued recently, court records show. New mothers said they compare stories of their legal run-ins with the medical center.
“There’s a lot that’s not right,” Sherry McKee, a dorm monitor at a tribal boarding school outside McAlester, said on the courthouse steps after the hearing. The hospital has sued her three times, most recently over a $3,375 bill for what she said turned out to be vertigo.
In recent years, major health systems in Virginia, North Carolina, and elsewhere have stopped suing patients following news reports about lawsuits. And several states, such as Maryland and New York, have restricted the legal actions hospitals can take against patients.
But with some 100 million people in the U.S. burdened by health care debt, medical collection cases still clog courtrooms across the country, researchers have found. In places like McAlester, a hospital’s debt collection machine can hum away quietly for years, helped along by powerful people in town. An effort to limit hospital lawsuits failed in the Oklahoma Legislature in 2021.
In McAlester, the lawsuits have provided business for some, such as the Adjustment Bureau, a local collection agency run out of a squat concrete building down the street from the courthouse, and for Hackler, a former president of the McAlester Area Chamber of Commerce. But for many patients and their families, the lawsuits can take a devastating toll, sapping wages, emptying retirement accounts, and upending lives.
McKee said she wasn’t sure how long it would take to pay off the recent judgment. Her $3,375 debt exceeds her monthly salary, she said.
“This affects a large number of people in a small community,” said Janet Roloff, an attorney who has spent years assisting low-income clients with legal issues such as evictions in and around McAlester. “The impact is great.”
Settled more than a century ago by fortune seekers who secured land from the Choctaw Nation to mine coal in the nearby hills, McAlester was once a boom town. Vestiges of that era remain, including a mammoth, 140-foot-tall Masonic temple that looms over the city.
Recent times have been tougher for McAlester, now home by one count to 12 marijuana dispensaries and the state’s death row. The downtown is pockmarked by empty storefronts, including the OKLA theater, which has been dark for decades. Nearly 1 in 5 residents in McAlester and the surrounding county live below the federal poverty line.
The hospital, operated by a public trust under the city’s authority, faces its own struggles. Paint is peeling off the front portico, and weeds poke up through the parking lots. The hospital has operated in the red for years, according to independent audit reports available on the state auditor’s website.
“I’m trying to find ways to get the entire community better care and more care,” said Shawn Howard, the hospital’s chief executive. Howard grew up in McAlester and proudly noted he started his career as a receptionist in the hospital’s physical therapy department. “This is my hometown,” he said. “I am not trying to keep people out of getting care.”
The hospital operates a clinic for low-income patients, whose webpage notes it has “limited appointments” at no cost for patients who are approved for aid. But data from the audits shows the hospital offers very little financial assistance, despite its purported mission to serve the community.
In the 2022 fiscal year, it provided just $114,000 in charity care, out of a total operating budget of more than $100 million, hospital records show. Charity care totaling $2 million or $3 million out of a $100 million budget would be more in line with other U.S. hospitals.
While audits show few McAlester patients get financial aid, many get taken to court.
Renee Montgomery, the city treasurer in an adjoining town and mother of a local police officer, said she dipped into savings she’d reserved for her children and grandchildren after the hospital sued her last year for more than $5,500. She’d gone to the emergency room for chest pain.
Dusty Powell, a truck driver, said he lost his pickup and motorcycle when his wages were garnished after the hospital sued him for almost $9,000. He’d gone to the emergency department for what turned out to be gastritis and didn’t have insurance, he said.
“Everyone in this town probably has a story about McAlester Regional,” said another former patient who spoke on the condition she not be named, fearful to publicly criticize the hospital in such a small city. “It’s not even a secret.”
The woman, who works at an Army munitions plant outside town, was sued twice over bills she incurred giving birth. Her sister-in-law has been sued as well.
“It’s a good-old-boy system,” said the woman, who lowered her voice when the mayor walked into the coffee shop where she was meeting with KFF Health News. Now, she said, she avoids the hospital if her children need care.
Nationwide, most people sued in debt collection cases never challenge them, a response experts say reflects widespread misunderstanding of the legal process and anxiety about coming to court.
At the center of the McAlester hospital’s collection efforts for decades has been Hackler & Hackler.
Donald Hackler was city attorney in McAlester for 13 years in the ’70s and ’80s and a longtime member of the local Lions Club and the Scottish Rite Freemasons.
Daughter Deborah Hackler, who joined the family firm 30 years ago, has been a deacon at the First Presbyterian Church of McAlester and served on the board of the local Girl Scouts chapter, according to the McAlester News-Capital newspaper, which named her “Woman of the Year” in 2007. Since 2001, she also has been a municipal judge in McAlester, hearing traffic cases, including some involving people she has sued on behalf of the hospital, municipal and county court records show.
For years, the Hacklers’ debt collection cases were often heard by Judge James Bland, who has retired from the bench and now sits on the hospital board. Bland didn’t respond to an inquiry for interview.
Hackler declined to speak with KFF Health News after her recent court appearance. “I’m not going to visit with you about a current client,” she said before leaving the courthouse.
Howard, the hospital CEO, said he couldn’t discuss the lawsuits either. He said he didn’t know the hospital took its patients to court. “I had to call and ask if we sue people,” he said.
Howard also said he didn’t know Deborah Hackler. “I never heard her name before,” he said.
Despite repeated public records requests from KFF Health News since September, the hospital did not provide detailed information about its financial arrangement with Hackler.
McAlester Mayor John Browne, who appoints the hospital’s board of trustees, said he, too, didn’t know about the lawsuits. “I hadn’t heard anything about them suing,” he said.
At the century-old courthouse in downtown McAlester, it’s not hard to find the lawsuits, though. Every month or two, another batch fills the docket in the small-claims court, now presided over by Judge Brian McLaughlin.
After court recently, McLaughlin, who is not from McAlester, shook his head at the stream of cases and patients who almost never show up to defend themselves, leaving him to issue judgment after judgment in the hospital’s favor.
“All I can do is follow the law,” said McLaughlin. “It doesn’t mean I like it.”
About This Project
“Diagnosis: Debt” is a reporting partnership between KFF Health News and NPR exploring the scale, impact, and causes of medical debt in America.
The series draws on original polling by KFF, court records, federal data on hospital finances, contracts obtained through public records requests, data on international health systems, and a yearlong investigation into the financial assistance and collection policies of more than 500 hospitals across the country.
Additional research was conducted by the Urban Institute, which analyzed credit bureau and other demographic data on poverty, race, and health status for KFF Health News to explore where medical debt is concentrated in the U.S. and what factors are associated with high debt levels.
The JPMorgan Chase Institute analyzed records from a sampling of Chase credit card holders to look at how customers’ balances may be affected by major medical expenses. And the CED Project, a Denver nonprofit, worked with KFF Health News on a survey of its clients to explore links between medical debt and housing instability.
KFF Health News journalists worked with KFF public opinion researchers to design and analyze the “KFF Health Care Debt Survey.” The survey was conducted Feb. 25 through March 20, 2022, online and via telephone, in English and Spanish, among a nationally representative sample of 2,375 U.S. adults, including 1,292 adults with current health care debt and 382 adults who had health care debt in the past five years. The margin of sampling error is plus or minus 3 percentage points for the full sample and 3 percentage points for those with current debt. For results based on subgroups, the margin of sampling error may be higher.
Reporters from KFF Health News and NPR also conducted hundreds of interviews with patients across the country; spoke with physicians, health industry leaders, consumer advocates, debt lawyers, and researchers; and reviewed scores of studies and surveys about medical debt.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Ham Substitute in Bean Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I am interested in what I can substitute for ham in bean soup?
Well, that depends on what the ham was like! You can certainly buy ready-made vegan lardons (i.e. small bacon/ham bits, often in tiny cubes or similar) in any reasonably-sized supermarket. Being processed, they’re not amazing for the health, but are still an improvement on pork.
Alternatively, you can make your own seitan! Again, seitan is really not a health food, but again, it’s still relatively less bad than pork (unless you are allergic to gluten, in which case, definitely skip this one).
Alternatively alternatively, in a soup that already contains beans (so the protein element is already covered), you could just skip the ham as an added ingredient, and instead bring the extra flavor by means of a little salt, a little yeast extract (if you don’t like yeast extract, don’t worry, it won’t taste like it if you just use a teaspoon in a big pot, or half a teaspoon in a smaller pot), and a little smoked paprika. If you want to go healthier, you can swap out the salt for MSG, which enhances flavor in a similar fashion while containing less sodium.
Wondering about the health aspects of MSG? Check out our main feature on this, from last month:
Share This Post
Related Posts
-
Should You Soak Your Nuts?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝hi. how many almonds should one eat per day? do they need to be soaked? thank you.❞
Within reason, however many you like! Given that protein is an appetite suppressant, you’ll probably find it’s not too many.
Dr. Michael Greger, of “How Not To Die” fame, suggests aiming for 30g of nuts per day. Since almonds typically weigh about 1g each, that means 30 if it’s all almonds.
And if you’re wondering about 10 almonds? The name’s a deliberate reference to an old internet hoax about 10 almonds being the equivalent of an aspirin for treating a headache. It’s a reminder to be open-mindedly skeptical about information circulating wildly, and look into the real, evidence-based, science of things.
- Sometimes, the science validates claims, and we’re excited to share that!
- Sometimes, the science just shoots claims down, and it’s important to acknowledge when that happens too.
On which note, about soaking…
Short version: soaking can improve the absorption of some nutrients, but not much more than simply chewing thoroughly. See:
- A review of the impact of processing on nutrient bioaccessibility and digestion of almonds
- Mastication of almonds: effects of lipid bioaccessibility, appetite, and hormone response
Soaking does reduce certain “antinutrients” (compounds that block absorption of other nutrients), such as phytic acid. However, even a 24-hour soak reduces them only by about 5%:
If you don’t want to take 24-hours to get a 5% benefit, there’s good news! A 12-hour soak can result in 4% less phytic acid in chopped (but not whole) almonds:
The Effect of Soaking Almonds and Hazelnuts on Phytate and Mineral Concentrations
Lest that potentially underwhelming benefit leave a bitter taste in your mouth, one good thing about soaking almonds (if you don’t like bitter tastes, anyway) is that it will reduce their bitterness:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Avoid Knee Surgery With This Proven Strategy (Over-50s Specialist Physio)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A diagnosis of knee arthritis can be very worrying, but it doesn’t necessarily mean a knee replacement surgery is inevitable. Here’s how to keep your knee better, for longer (and potentially, for life):
Flexing your good health
You know we wouldn’t let that “proven” go by unchallenged if it weren’t, so what’s the evidence for it? Research (papers linked in the video description) showed 70% of patients (so, not 100%, but 70% is good odds and a lot better than the alternative) with mild to moderate knee arthritis avoided surgery after following a specific protocol—the one we’re about to describe.
The key strategy is to focus on strengthening the quadriceps muscles for joint protection, as strong quads correlate with reduced pain. However, a full range of motion in the knee is essential for optimal quad function, so that needs attention too, and in fact is foundational (can’t strengthen a quadriceps that doesn’t have a range of motion available to it):
Steps to follow:
- Improve knee extension:
- Passive knee extension exercise: gently press your knee down while lying flat, to increase straightening.
- Weighted heel props: use light weights to encourage gradual knee straightening.
- Enhance knee flexion:
- Use a towel to gently pull the knee towards the body to improve bending range.
Regular practice (multiple times daily) leads to improved knee function and pain relief. Exercises should be performed gently and without pain, aiming for consistent, gradual progress.And of course, if you do experience pain, it is recommend to consult with a local physiotherapist for more personalized guidance.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Treat Your Own Knee – by Robin McKenzie
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Improve knee extension:
-
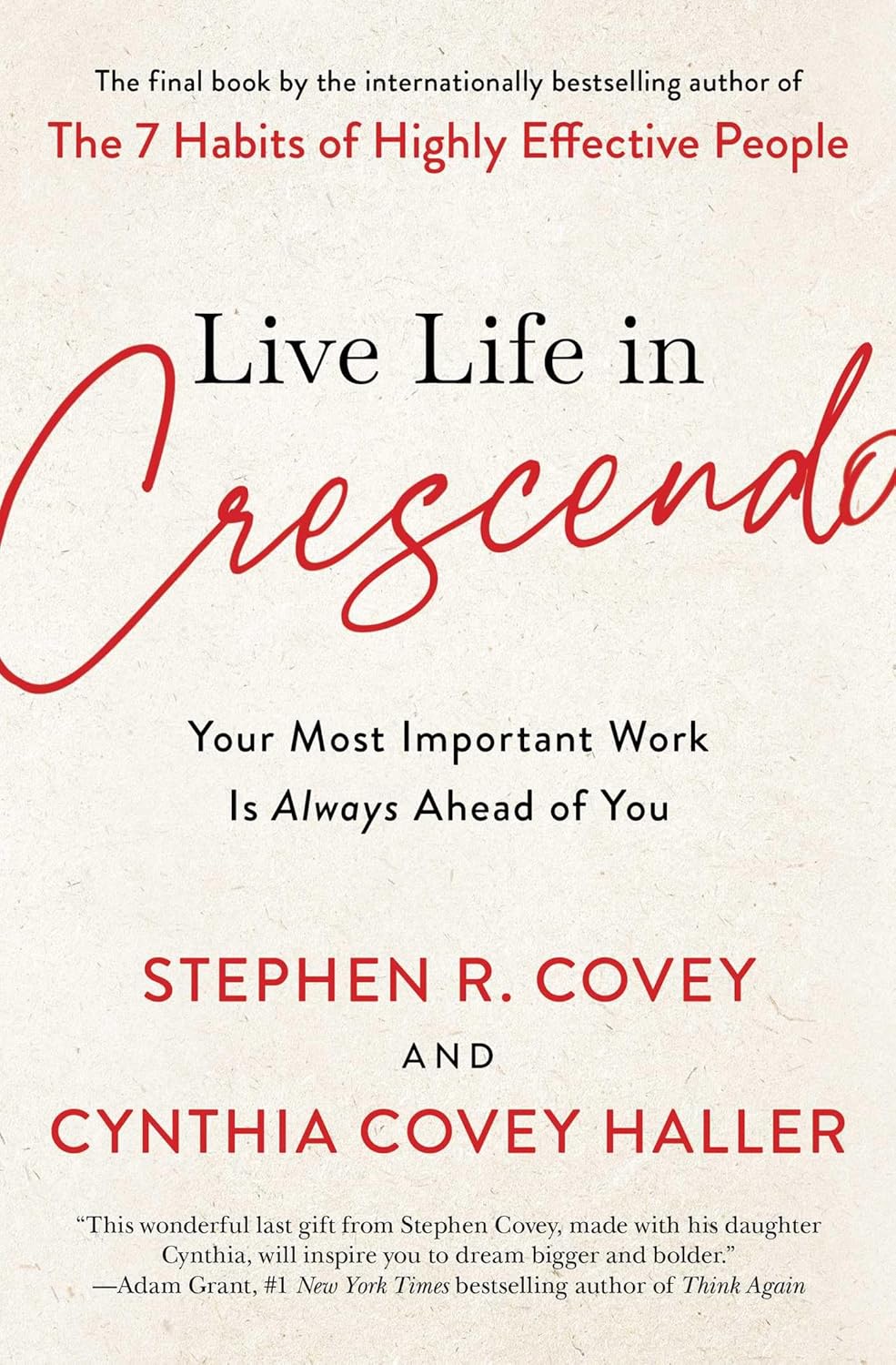
Live Life in Crescendo – by Stephen Covey and Cynthia Covey-Haller
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Stephen Covey is of course best known for his “7 Habits of Highly Effective People“, while the dozen books he wrote afterwards, not including this one, did not get the same acclaim.
Not including this one, because this one was published posthumously and, notwithstanding the order of the names on the cover, in all likelihood his daughter wrote most of.
And yet! The very spirit of this book is in defiance of 7 Habits being his “early career” magnum opus. We say “early career”, because he was 57 already when that was published, but it was one of his earlier books.
In this work the authors lay out the case for how “your most important work is always ahead of you“, and that it is perfectly possible to “live life in crescendo“, and keep on giving whatever it is that we want to give to the world.
We also learn, mostly through storytelling, of how people are infinitely more important than things, and that it is there that we should put our investments. And that while adversity may not make us stronger, it just means we may need to change our approach, to continue to be productive in whatever way is meaningful to us.
Bottom line: if ever you wonder how your future could live up to your past (in a good way), this is the book to get you thinking.
Click here to check out Live Life in Crescendo, and figure out what your next great work will be!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: