Getting COMFY – by Jordan Gross
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to see how good “morning people” seem to have it; it’s harder, it seems, to become one.
And, if we’re forced by circumstance to be the morning person we’re not? We all-too-easily find ourselves greeting each coming day without the joy that, in an ideal world, we might.
So, is it possible to learn this power? Jordan Gross has it mapped out for it us…
The “COMFY” of the title is indeed an acronym, and it stands for:
- Calm
- Openness
- Movement
- Funny
- You
There’s a chapter explaining each in detail, and they’re bookended with other chapters explaining more about the whys and the hows.
As you might expect, the key to a good morning starts the night before, but there’s also a formula to follow. Of course, you can change it up, mix and match if you like… but this book provides a base framework to build from, which is something that can make a huge difference!
Bottom line: it’s a highly enjoyable book to read, and also provides genuine powerful help to bring us the brighter happier mornings we deserve—the set-up to the perfect day!
Click here to check out “Getting COMFY” and perk up your mornings—you deserve it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Peas vs Broad Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peas to broad beans, we picked the peas.
Why?
Both are great of course, but…
Looking at the macros to start with, peas have more protein and more fiber. The differences aren’t huge, but they are clear.
In terms of vitamins, peas have more of vitamins A, B1, B2, B3, B5, B6, B9, E, K, and choline (some with very large margins, some with small), while broad beans contain a little more vitamin C (the margin is quite narrow though).
When it comes to minerals, peas have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while broad beans have more sodium. So this category wasn’t close.
Adding up the win from each of the categories makes for a clear triple-win for peas.
Easy-peasy!
Want to learn more?
You might like to read:
Take care!
Share This Post
-
Overdosing on Chemo: A Common Gene Test Could Save Hundreds of Lives Each Year
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One January morning in 2021, Carol Rosen took a standard treatment for metastatic breast cancer. Three gruesome weeks later, she died in excruciating pain from the very drug meant to prolong her life.
Rosen, a 70-year-old retired schoolteacher, passed her final days in anguish, enduring severe diarrhea and nausea and terrible sores in her mouth that kept her from eating, drinking, and, eventually, speaking. Skin peeled off her body. Her kidneys and liver failed. “Your body burns from the inside out,” said Rosen’s daughter, Lindsay Murray, of Andover, Massachusetts.
Rosen was one of more than 275,000 cancer patients in the United States who are infused each year with fluorouracil, known as 5-FU, or, as in Rosen’s case, take a nearly identical drug in pill form called capecitabine. These common types of chemotherapy are no picnic for anyone, but for patients who are deficient in an enzyme that metabolizes the drugs, they can be torturous or deadly.
Those patients essentially overdose because the drugs stay in the body for hours rather than being quickly metabolized and excreted. The drugs kill an estimated 1 in 1,000 patients who take them — hundreds each year — and severely sicken or hospitalize 1 in 50. Doctors can test for the deficiency and get results within a week — and then either switch drugs or lower the dosage if patients have a genetic variant that carries risk.
Yet a recent survey found that only 3% of U.S. oncologists routinely order the tests before dosing patients with 5-FU or capecitabine. That’s because the most widely followed U.S. cancer treatment guidelines — issued by the National Comprehensive Cancer Network — don’t recommend preemptive testing.
The FDA added new warnings about the lethal risks of 5-FU to the drug’s label on March 21 following queries from KFF Health News about its policy. However, it did not require doctors to administer the test before prescribing the chemotherapy.
The agency, whose plan to expand its oversight of laboratory testing was the subject of a House hearing, also March 21, has said it could not endorse the 5-FU toxicity tests because it’s never reviewed them.
But the FDA at present does not review most diagnostic tests, said Daniel Hertz, an associate professor at the University of Michigan College of Pharmacy. For years, with other doctors and pharmacists, he has petitioned the FDA to put a black box warning on the drug’s label urging prescribers to test for the deficiency.
“FDA has responsibility to assure that drugs are used safely and effectively,” he said. The failure to warn, he said, “is an abdication of their responsibility.”
The update is “a small step in the right direction, but not the sea change we need,” he said.
Europe Ahead on Safety
British and European Union drug authorities have recommended the testing since 2020. A small but growing number of U.S. hospital systems, professional groups, and health advocates, including the American Cancer Society, also endorse routine testing. Most U.S. insurers, private and public, will cover the tests, which Medicare reimburses for $175, although tests may cost more depending on how many variants they screen for.
In its latest guidelines on colon cancer, the Cancer Network panel noted that not everyone with a risky gene variant gets sick from the drug, and that lower dosing for patients carrying such a variant could rob them of a cure or remission. Many doctors on the panel, including the University of Colorado oncologist Wells Messersmith, have said they have never witnessed a 5-FU death.
In European hospitals, the practice is to start patients with a half- or quarter-dose of 5-FU if tests show a patient is a poor metabolizer, then raise the dose if the patient responds well to the drug. Advocates for the approach say American oncology leaders are dragging their feet unnecessarily, and harming people in the process.
“I think it’s the intransigence of people sitting on these panels, the mindset of ‘We are oncologists, drugs are our tools, we don’t want to go looking for reasons not to use our tools,’” said Gabriel Brooks, an oncologist and researcher at the Dartmouth Cancer Center.
Oncologists are accustomed to chemotherapy’s toxicity and tend to have a “no pain, no gain” attitude, he said. 5-FU has been in use since the 1950s.
Yet “anybody who’s had a patient die like this will want to test everyone,” said Robert Diasio of the Mayo Clinic, who helped carry out major studies of the genetic deficiency in 1988.
Oncologists often deploy genetic tests to match tumors in cancer patients with the expensive drugs used to shrink them. But the same can’t always be said for gene tests aimed at improving safety, said Mark Fleury, policy director at the American Cancer Society’s Cancer Action Network.
When a test can show whether a new drug is appropriate, “there are a lot more forces aligned to ensure that testing is done,” he said. “The same stakeholders and forces are not involved” with a generic like 5-FU, first approved in 1962, and costing roughly $17 for a month’s treatment.
Oncology is not the only area in medicine in which scientific advances, many of them taxpayer-funded, lag in implementation. For instance, few cardiologists test patients before they go on Plavix, a brand name for the anti-blood-clotting agent clopidogrel, although it doesn’t prevent blood clots as it’s supposed to in a quarter of the 4 million Americans prescribed it each year. In 2021, the state of Hawaii won an $834 million judgment from drugmakers it accused of falsely advertising the drug as safe and effective for Native Hawaiians, more than half of whom lack the main enzyme to process clopidogrel.
The fluoropyrimidine enzyme deficiency numbers are smaller — and people with the deficiency aren’t at severe risk if they use topical cream forms of the drug for skin cancers. Yet even a single miserable, medically caused death was meaningful to the Dana-Farber Cancer Institute, where Carol Rosen was among more than 1,000 patients treated with fluoropyrimidine in 2021.
Her daughter was grief-stricken and furious after Rosen’s death. “I wanted to sue the hospital. I wanted to sue the oncologist,” Murray said. “But I realized that wasn’t what my mom would want.”
Instead, she wrote Dana-Farber’s chief quality officer, Joe Jacobson, urging routine testing. He responded the same day, and the hospital quickly adopted a testing system that now covers more than 90% of prospective fluoropyrimidine patients. About 50 patients with risky variants were detected in the first 10 months, Jacobson said.
Dana-Farber uses a Mayo Clinic test that searches for eight potentially dangerous variants of the relevant gene. Veterans Affairs hospitals use a 11-variant test, while most others check for only four variants.
Different Tests May Be Needed for Different Ancestries
The more variants a test screens for, the better the chance of finding rarer gene forms in ethnically diverse populations. For example, different variants are responsible for the worst deficiencies in people of African and European ancestry, respectively. There are tests that scan for hundreds of variants that might slow metabolism of the drug, but they take longer and cost more.
These are bitter facts for Scott Kapoor, a Toronto-area emergency room physician whose brother, Anil Kapoor, died in February 2023 of 5-FU poisoning.
Anil Kapoor was a well-known urologist and surgeon, an outgoing speaker, researcher, clinician, and irreverent friend whose funeral drew hundreds. His death at age 58, only weeks after he was diagnosed with stage 4 colon cancer, stunned and infuriated his family.
In Ontario, where Kapoor was treated, the health system had just begun testing for four gene variants discovered in studies of mostly European populations. Anil Kapoor and his siblings, the Canadian-born children of Indian immigrants, carry a gene form that’s apparently associated with South Asian ancestry.
Scott Kapoor supports broader testing for the defect — only about half of Toronto’s inhabitants are of European descent — and argues that an antidote to fluoropyrimidine poisoning, approved by the FDA in 2015, should be on hand. However, it works only for a few days after ingestion of the drug and definitive symptoms often take longer to emerge.
Most importantly, he said, patients must be aware of the risk. “You tell them, ‘I am going to give you a drug with a 1 in 1,000 chance of killing you. You can take this test. Most patients would be, ‘I want to get that test and I’ll pay for it,’ or they’d just say, ‘Cut the dose in half.’”
Alan Venook, the University of California-San Francisco oncologist who co-chairs the panel that sets guidelines for colorectal cancers at the National Comprehensive Cancer Network, has led resistance to mandatory testing because the answers provided by the test, in his view, are often murky and could lead to undertreatment.
“If one patient is not cured, then you giveth and you taketh away,” he said. “Maybe you took it away by not giving adequate treatment.”
Instead of testing and potentially cutting a first dose of curative therapy, “I err on the latter, acknowledging they will get sick,” he said. About 25 years ago, one of his patients died of 5-FU toxicity and “I regret that dearly,” he said. “But unhelpful information may lead us in the wrong direction.”
In September, seven months after his brother’s death, Kapoor was boarding a cruise ship on the Tyrrhenian Sea near Rome when he happened to meet a woman whose husband, Atlanta municipal judge Gary Markwell, had died the year before after taking a single 5-FU dose at age 77.
“I was like … that’s exactly what happened to my brother.”
Murray senses momentum toward mandatory testing. In 2022, the Oregon Health & Science University paid $1 million to settle a suit after an overdose death.
“What’s going to break that barrier is the lawsuits, and the big institutions like Dana-Farber who are implementing programs and seeing them succeed,” she said. “I think providers are going to feel kind of bullied into a corner. They’re going to continue to hear from families and they are going to have to do something about it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Honey vs Maple Syrup – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing honey to maple syrup, we picked the honey.
Why?
It was very close, as both have small advantages:
• Honey has some medicinal properties (and depending on type, may contain an antihistamine)
• Maple syrup is a good source of manganese, as well as low-but-present amounts of other mineralsHowever, you wouldn’t want to eat enough maple syrup to rely on it as a source of those minerals, and honey has the lower GI (average 46 vs 54; for comparison, refined sugar is 65), which works well as a tie-breaker.
(If GI’s very important to you, though, the easy winner here would be agave syrup if we let it compete, with its GI of 15)
Read more:
• Can Honey Relieve Allergies?
• From Apples to Bees, and High-Fructose C’sShare This Post
Related Posts
-
The “Yes I Can” Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes, we are given to ask ourselves: “Can I produce a healthy and tasty salad out of what I have in?” and today we show how, with a well-stocked pantry, the answer is “yes I can”, regardless of what is (or isn’t) in the fridge.
You will need
- 1 can cannellini beans, drained
- 1 can sardines (if vegetarian/vegan, substitute ½ can chickpeas, drained)
- 1 can mandarin segments
- 1 handful pitted black olives, from a jar (or from a can, if you want to keep the “yes I can” theme going)
- ½ red onion, thinly sliced (this can be from frozen, defrosted—sliced/chopped onion is always a good thing to have in your freezer, by the way; your writer here always has 1–6 lbs of chopped onions in hers, divided into 1lb bags)
- 1 oz lemon juice
- 1 tbsp chopped parsley (this can be freeze-dried, but fresh is good if you have it)
- 1 tbsp extra virgin olive oil
- 1 tbsp chia seeds
- 1 tsp miso paste
- 1 tsp honey (omit if you don’t care for sweetness; substitute with agave nectar if you do like sweetness but don’t want to use honey specifically)
- 1 tsp red chili flakes
Method
(we suggest you read everything at least once before doing anything)
1) Combine the onion and the lemon juice in a small bowl, massaging gently
2) Mix (in another bowl) the miso paste with the chili flakes, chia seeds, honey, olive oil, and the spare juice from the can of mandarin segments, and whisk it to make a dressing.
3) Add the cannellini beans, sardines (break them into bite-size chunks), mandarin segments, olives, and parsley, tossing them thoroughly (but gently) in the dressing.
4) Top with the sliced onion, discarding the excess lemon juice, and serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Three Daily Servings of Beans?
- We Are Such Stuff As Fish Are Made Of
- Chia: The Tiniest Seeds With The Most Value
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Getting antivirals for COVID too often depends on where you live and how wealthy you are
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Medical experts recommend antivirals for people aged 70 and older who get COVID, and for other groups at risk of severe illness and hospitalisation from COVID.
But many older Australians have missed out on antivirals after getting sick with COVID. It is yet another way the health system is failing the most vulnerable.
CGN089/Shutterstock Who missed out?
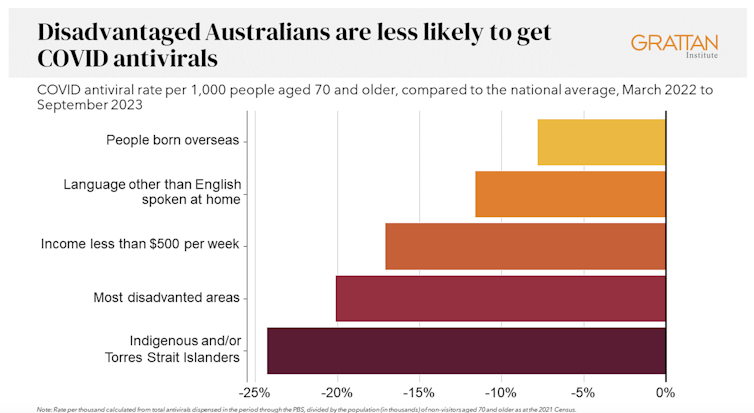
We analysed COVID antiviral uptake between March 2022 and September 2023. We found some groups were more likely to miss out on antivirals including Indigenous people, people from disadvantaged areas, and people from culturally and linguistically diverse backgrounds.
Some of the differences will be due to different rates of infection. But across this 18-month period, many older Australians were infected at least once, and rates of infection were higher in some disadvantaged communities.
How stark are the differences?
Compared to the national average, Indigenous Australians were nearly 25% less likely to get antivirals, older people living in disadvantaged areas were 20% less likely to get them, and people with a culturally or linguistically diverse background were 13% less likely to get a script.
People in remote areas were 37% less likely to get antivirals than people living in major cities. People in outer regional areas were 25% less likely.
Dispensing rates by group. Grattan Institute Even within the same city, the differences are stark. In Sydney, people older than 70 in the affluent eastern suburbs (including Vaucluse, Point Piper and Bondi) were nearly twice as likely to have had an antiviral as those in Fairfield, in Sydney’s south-west.
Older people in leafy inner-eastern Melbourne (including Canterbury, Hawthorn and Kew) were 1.8 times more likely to have had an antiviral as those in Brimbank (which includes Sunshine) in the city’s west.
Why are people missing out?
COVID antivirals should be taken when symptoms first appear. While awareness of COVID antivirals is generally strong, people often don’t realise they would benefit from the medication. They wait until symptoms get worse and it is too late.
Frequent GP visits make a big difference. Our analysis found people 70 and older who see a GP more frequently were much more likely to be dispensed a COVID antiviral.
Regular visits give an opportunity for preventive care and patient education. For example, GPs can provide high-risk patients with “COVID treatment plans” as a reminder to get tested and seek treatment as soon as they are unwell.
Difficulty seeing a GP could help explain low antiviral use in rural areas. Compared to people in major cities, people in small rural towns have about 35% fewer GPs, see their GP about half as often, and are 30% more likely to report waiting too long for an appointment.
Just like for vaccination, a GP’s focus on antivirals probably matters, as does providing care that is accessible to people from different cultural backgrounds.
Care should go those who need it
Since the period we looked at, evidence has emerged that raises doubts about how effective antivirals are, particularly for people at lower risk of severe illness. That means getting vaccinated is more important than getting antivirals.
But all Australians who are eligible for antivirals should have the same chance of getting them.
These drugs have cost more than A$1.7 billion, with the vast majority of that money coming from the federal government. While dispensing rates have fallen, more than 30,000 packs of COVID antivirals were dispensed in August, costing about $35 million.
Such a huge investment shouldn’t be leaving so many people behind. Getting treatment shouldn’t depend on your income, cultural background or where you live. Instead, care should go to those who need it the most.
Getting antivirals shouldn’t depend on who your GP is. National Cancer Institute/Unsplash People born overseas have been 40% more likely to die from COVID than those born here. Indigenous Australians have been 60% more likely to die from COVID than non-Indigenous people. And the most disadvantaged people have been 2.8 times more likely to die from COVID than those in the wealthiest areas.
All those at-risk groups have been more likely to miss out on antivirals.
It’s not just a problem with antivirals. The same groups are also disproportionately missing out on COVID vaccination, compounding their risk of severe illness. The pattern is repeated for other important preventive health care, such as cancer screening.
A 3-step plan to meet patients’ needs
The federal government should do three things to close these gaps in preventive care.
First, the government should make Primary Health Networks (PHNs) responsible for reducing them. PHNs, the regional bodies responsible for improving primary care, should share data with GPs and step in to boost uptake in communities that are missing out.
Second, the government should extend its MyMedicare reforms. MyMedicare gives general practices flexible funding to care for patients who live in residential aged care or who visit hospital frequently. That approach should be expanded to all patients, with more funding for poorer and sicker patients. That will give GP clinics time to advise patients about preventive health, including COVID vaccines and antivirals, before they get sick.
Third, team-based pharmacist prescribing should be introduced. Then pharmacists could quickly dispense antivirals for patients if they have a prior agreement with the patient’s GP. It’s an approach that would also work for medications for chronic diseases, such as cardiovascular disease.
COVID antivirals, unlike vaccines, have been keeping up with new variants without the need for updates. If a new and more harmful variant emerges, or when a new pandemic hits, governments should have these systems in place to make sure everyone who needs treatment can get it fast.
In the meantime, fairer access to care will help close the big and persistent gaps in health between different groups of Australians.
Peter Breadon, Program Director, Health and Aged Care, Grattan Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Shedding Some Obesity Myths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s shed some obesity myths!
There are a lot of myths and misconceptions surrounding obesity… And then there are also reactive opposite myths and misconceptions, which can sometimes be just as harmful!
To tackle them all would take a book, but in classic 10almonds style, we’re going to put a spotlight on some of the ones that might make the biggest difference:
True or False: Obesity is genetically pre-determined
False… With caveats.
Some interesting results have been found from twin studies and adoption studies, showing that genes definitely play some role, but lifestyle is—for most people—the biggest factor:
- The body-mass index of twins who have been reared apart
- An adoption study of human obesity
- Using a sibling-adoption design to parse genetic and environmental influences on children’s body mass index
In short: genes predispose; they don’t predetermine. But that predisposition alone can make quite a big difference, if it in turn leads to different lifestyle factors.
But upon seeing those papers centering BMI, let’s consider…
True or False: BMI is a good, accurate measure of health in the context of bodyweight
False… Unless you’re a very large group of thin white men of moderate height, which was the demographic the system was built around.
Bonus information: it was never intended to be used to measure the weight-related health of any individual (not even an individual thin white man of moderate height), but rather, as a tool to look at large-scale demographic trends.
Basically, as a system, it’s being used in a way it was never made for, and the results of that misappropriation of an epidemiological tool for individual health are predictably unhelpful.
To do a deep-dive into all the flaws of the BMI system, which are many, we’d need to devote a whole main feature just to that.
Update: we have now done so!
Here it is: When BMI Doesn’t Measure Up
True or False: Obesity does not meaningfully impact more general health
False… In more ways than one (but there are caveats)
Obesity is highly correlated with increased risk of all-cause mortality, and weight loss, correspondingly, correlates with a reduced risk. See for example:
So what are the caveats?
Let’s put it this way: owning a horse is highly correlated with increased healthy longevity. And while owning a horse may come with some exercise and relaxation (both of which are good for the health), it’s probably mostly not the horse itself that conveys the health benefits… it’s that someone who has the resources to look after a horse, probably has the resources to look after their own health too.
So sometimes there can be a reason for a correlation (it’s not a coincidence!) but the causative factor is partially (or in some cases, entirely) something else.
So how could this play out with obesity?
There’s a lot of discrimination in healthcare settings, unfortunately! In this case, it often happens that a thin person goes in with a medical problem and gets treated for that, while a fat person can go in with the same medical problem and be told “you should try losing some weight”.
Top tip if this happens to you… Ask: “what would you advise/prescribe to a thin person with my same symptoms?”
Other things may be more systemic, for example:
When a thin person goes to get their blood pressure taken, and that goes smoothly, while a fat person goes to get their blood pressure taken, and there’s not a blood pressure cuff to fit them, is the problem the size of the person or the size of the cuff? It all depends on perspective, in a world built around thin people.
That’s a trivial-seeming example, but the same principle has far-reaching (and harmful) implications in healthcare in general, e.g:
- Surgeons being untrained (and/or unwilling) to operate on fat people
- Getting a one-size-fits-all dose that was calculated using average weight, and now doesn’t work
- MRI machines are famously claustrophobia-inducing for thin people; now try not fitting in it in the first place
…and so forth. So oftentimes, obesity will be correlated with a poor healthcare outcome, where the problem is not actually the obesity itself, but rather the system having been set up with thin people in mind.
It would be like saying “Having O- blood type results in higher risks when receiving blood transfusions”, while omitting to add “…because we didn’t stock O- blood”.
True or False: to reduce obesity, just eat less and move more!
False… Mostly.
Moving more is almost always good for most people. When it comes to diet, quality is much more important than quantity. But these factors alone are only part of the picture!
But beyond diet and exercise, there are many other implicated factors in weight gain, weight maintenance, and weight loss, including but not limited to:
- Disrupted sleep
- Chronic stress
- Chronic pain
- Hormonal imbalances
- Physical disabilities that preclude a lot of exercise
- Mental health issues that add (and compound) extra levels of challenge
- Medications that throw all kinds of spanners into the works with their side effects
…and even just those first two things, diet and exercise, are not always so correlated to weight as one might think—studies have found that the difference for exercise especially is often marginal:
Read: Widespread misconceptions about obesity ← academic article in the Journal of the College of Family Physicians of Canada
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: