The push for Medicare to cover weight-loss drugs: An explainer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The largest U.S. insurer, Medicare, does not cover weight-loss drugs, making it tougher for older people to get access to promising new medications.
If you cover stories about drug costs in the U.S., it’s important to understand why Medicare’s Part D pharmacy program, which covers people aged 65 and older and people with certain disabilities, doesn’t cover weight-loss drugs today. It’s also important to consider what would happen if Medicare did start covering weight loss drugs. This explainer will give you a brief overview of the issues and then summarize some recent publications the benefits and costs of drugs like semaglutide and tirzepatide.
First, what are these new and newsy weight loss drugs?
Semaglutide is a medication used for both the treatment of type 2 diabetes and for long-term weight management in adults with obesity. It debuted in the United States in 2017 as an injectable diabetes drug called Ozempic, manufactured by Novo Nordisk. It’s part of a class of drugs that mimics the action of glucagon, a substance that the human body makes to aid digestion.
Glucagon-like peptide-1 (GLP-1) drugs like semaglutide help prompt the body to release insulin. But they also cause a minor delay in the pace of digestion, helping people feel sated after eating.
That second effect turned Ozempic into a widely used weight-loss drug, even before the Food and Drug Administration (FDA) gave its okay for this use. Doctors in the United States can prescribe medicines for uses beyond those approved by the FDA. This is known as off-label use.
In writing about her own experience in using the medicine to help her shed 40 pounds, Washington Post columnist Ruth Marcus in June noted that Novo Nordisk mentioned the potential for weight loss in its “ubiquitous cable ads (‘Oh-oh-oh, Ozempic!’)”
The American Society of Health-System Pharmacists has reported shortages of semaglutide due to demand, leaving some people with diabetes struggling to find supply of the medicine.
Novo Nordisk won Food and Drug Administration (FDA) approval in 2021 to market semaglutide as an injectable weight loss drug under the name Wegovy, but with a different dosing regimen than Ozempic. Rival Eli Lilly first won FDA approval of its similar GLP-1 diabetes drug, tirzepatide, in the United States in 2022 and sells it under the brand name Mounjaro.
In November of 2023, Eli Lilly won FDA approval to sell tirzepatide as a weight-loss drug, soon-to-be marketed under the brand name Zepbound. The company said it will set a monthly list price for a month’s supply of the drug at $1,059.87, which the company described as 20% discount to the cost of rival Novo Nordisk’s Wegovy. Wegovy has a list price of $1,349.02, according to the Novo Nordisk website.
Even when their insurance plans officially cover costs for weight loss drugs, consumers may face barriers in seeking that coverage for these drugs. Commercial health plans have in place prior authorization requirements to try to limit coverage of new weight-loss shots to those who qualify for these treatments. The Wegovy shot, for example, is intended for people whose weight reaches a certain benchmark for obesity or who are overweight and have a condition related to excess weight, such as diabetes, high blood pressure or high cholesterol.
State Medicaid programs, meanwhile, have taken approaches that vary by state. For example, the most populous U.S. state, California, provides some coverage to new weight-loss injections through its Medicaid program, but many others, including Texas, the No. 2 state in terms of population, do not, according to an online tool that Novo Nordisk created to help people check on coverage.
Medicare does cover semaglutide for treatment of diabetes, and the insurer reported $3 billion in 2021 spending on the drug under Medicare Part D. Congress last year gave Medicare new tools that might help it try to lower the cost of semaglutide.
Medicare is in the midst of implementing new authority it gained through the Inflation Reduction Act (IRA) of 2022 to negotiate with companies about the cost of certain medicines.
This legislation gave Medicare, for the first time, tools to directly negotiate with pharmaceutical companies on the cost of some medicines. Congress tailored this program to spare drug makers from negotiations for the first few years they put new medicines on the market, allowing them to recoup investment in these products.
Why doesn’t Medicare cover weight-loss drugs?
Congress created the Medicare Part D pharmacy program in 2003 to address a gap in coverage that had existed since the creation of Medicare in 1965. The program long covered the costs of drugs administered by doctors and those given in hospitals, but not the kinds of medicines people took on their own, like Wegovy shots.
In 2003, there seemed to be good reasons to leave weight-loss drugs out of the benefit, write Inmaculada Hernandez of the University of California, San Diego, and coauthors in their September 2023 editorial in the Journal of General Internal Medicine, “Medicare Part D Coverage of Anti-obesity Medications: a Call for Forward-Looking Policy Reform.”
When members of Congress worked on the Part D benefit, the drugs available on the market were known to have limited effectiveness and unpleasant side effects. And those members of Congress were aware of how a drug combination called fen-phen, once touted as a weight-loss miracle medicine, turned out in rare cases to cause fatal heart valve damage. In 1997, American Home Products, which later became Wyeth, took its fen-phen product off the market.
But today GLP-1 drugs like semaglutide appear to offer significant benefits, with far less risk and milder side effects, write Hernandez and coauthors.
“Other than budget impact, it is hard to find a reason to justify the historical statutory exclusion of weight loss drugs from coverage other than the stigma of the condition itself,” they write.
What’s happening today that could lead Medicare to start covering weight loss drugs?
Novo Nordisk and Eli Lilly both have hired lobbyists to try to persuade lawmakers to reverse this stance, according to Senate records. Pro tip: You can use the Senate’s lobbying disclosure database to track this and other issues. Type in the name of the company of interest and then read through the forms.
Some members of Congress already have been trying for years to strike the Medicare Part D restriction on weight-loss drugs. Over the past decade, senators Tom Carper (D-DE) and Bill Cassidy, MD, (R-LA) have repeatedly introduced bills that would do that. They introduced the current version, the Treat and Reduce Obesity Act of 2023, in July. It has the support of 10 other Republican senators and seven Democratic ones, as of Dec. 19. The companion House measure has the support of 41 Democrats and 23 Republicans in that chamber, which has 435 seats.
The influential nonprofit Institute for Clinical and Economic Review conducts in-depth analyses of drugs and medical treatments in the United States. ICER last year recommended passage of a law allowing Medicare Part D to cover weight-loss medications. ICER also called for broader coverage of weight-loss medications in state Medicaid programs. Insurers, including Medicare, consider ICER’s analyses in deciding whether to cover treatments.
While offering these calls for broader coverage as part of a broad assessment of obesity management, ICER also urged companies to reduce the costs of weight-loss medicines.
Most people with obesity can’t achieve sustained weight loss through diet and exercise alone, said David Rind, ICER’s chief medical officer in an August 2022 statement. The development of newer obesity treatments represents the achievement of a long-standing goal of medical research, but prices of these new products must be reasonable to allow broad access to them, he noted.
After an extensive process of reviewing studies, engaging in public debate and processing feedback, ICER concluded that semaglutide for weight loss should have an annual cost of $7,500 to $9,800, based on its potential benefits.
What does academic research say about the benefits and the potential costs of new obesity drugs?
Here are a couple of studies to consider when covering the ongoing story of weight-loss drug costs:
Medicare Part D Coverage of Antiobesity Medications — Challenges and Uncertainty Ahead
Khrysta Baig, Stacie B. Dusetzina, David D. Kim and Ashley A. Leech. New England Journal of Medicine, March 2023
In this Perspective piece, researchers at Vanderbilt University create a series of estimates about how much Medicare may have to spend annually on weight-loss drugs if the program eventually covers these drugs.
These include a high estimate — $268 billion — based on an extreme calculation, one reflecting the potential cost if virtually all people on Medicare who have obesity used semaglutide. In an announcement of the study on the Vanderbilt website, lead author Khrysta Baig described this as a “purely hypothetical scenario,” but one that “ underscores that at current prices, these medications cannot be the only way – or even the main way – we address obesity as a society.”
In a more conservative estimate, Bhaig and coauthors consider a case where only about 10% of those eligible for obesity treatment opted for semaglutide, which would result in $27 billion in new costs.
(To put these numbers in context, consider that the federal government now spends about $145 billion a year on the entire Part D program.)
It’s likely that all people enrolled in Part D would have to pay higher monthly premiums if Medicare were to cover weight-loss injections, Baig and coauthors write.
Baig and coauthors note that the recent ICER review of weight-loss drugs focused on patients younger than the Medicare population. The balance of benefits and risks associated with weight-loss drugs may be less favorable for older people than the younger ones, making it necessary to study further how these drugs work for people aged 65 and older, they write. For example, research has shown older adults with a high blood sugar level called prediabetes are less likely to develop diabetes than younger adults with this condition.
SELECTing Treatments for Cardiovascular Disease — Obesity in the Spotlight
Amit Khera and Tiffany M. Powell-Wiley. New England Journal of Medicine, Dec. 14, 2023
Semaglutide and Cardiovascular Outcomes in Patients Without Diabetes
A Michael Lincoff, et. al. New England Journal of Medicine, Dec. 14, 2023.
An editorial accompanies the publication of a semaglutide study that drew a lot of coverage in the media. The Semaglutide and Cardiovascular Outcomes in Obesity without Diabetes (SELECT) study was a randomized controlled trial, conducted by Novo Nordisk, which looked at rates of cardiovascular events in people who already had known heart risk and were overweight, but not diabetic. Patients were randomly assigned to receive a once-weekly dose of semaglutide (Wegovy) or a placebo.
In the study, the authors report that of the 8,803 patients who took Wegovy in the trial, 569 (6.5%) had a heart attack or another cardiovascular event, compared with 701 of the 8801 patients (8.0%) in the placebo group. The mean duration of exposure to semaglutide or placebo in the study was 34.2 months.
The study also reports a mean 9.4% reduction in body weight among patients taking Wegovy, while those on placebo had a mean loss of 0.88%.
The findings suggest Wegovy may be a welcome new treatment option for many people who have coronary disease and are overweight, but are not diabetic, write Khera and Powell-Wiley in their editorial.
But the duo, both of whom focus on disease prevention in their research, also call for more focus on the prevention and root causes of obesity and on the use of proven treatment approaches other than medication.
“Socioeconomic, environmental, and psychosocial factors contribute to incident obesity, and therefore equity-focused obesity prevention and treatment efforts must target multiple levels,” they write. “For instance, public policy targeting built environment features that limit healthy behaviors can be coupled with clinical care interventions that provide for social needs and access to treatments like semaglutide.”
Additional information:
The nonprofit KFF, formerly known as the Kaiser Family Foundation, has done recent reports looking at the potential for expanded coverage of semaglutide:
Medicaid Utilization and Spending on New Drugs Used for Weight Loss, Sept. 8, 2023
What Could New Anti-Obesity Drugs Mean for Medicare? May 18, 2023
And KFF held an Aug. 4 webinar, New Weight Loss Drugs Raise Issues of Coverage, Cost, Access and Equity, for which the recording is posted here.
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Feel Great, Lose Weight – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all know that losing weight sustainably tends to be harder than simply losing weight. We know that weight loss needs to come with lifestyle change. But how to get there?
One of the biggest problems that we might face while trying to lose weight is that our “metabolic thermostat” has got stuck at the wrong place. Trying to move it just makes our bodies think we are starving, and everything gets even worse. We can’t even “mind over matter” our way through it with willpower, because our bodies will do impressive things on a cellular level in an attempt to save us… Things that are as extraordinary as they are extraordinarily unhelpful.
Dr. Rangan Chatterjee is here to help us cut through that.
In this book, he covers how our metabolic thermostat got stuck in the wrong place, and how to gently tease it back into a better position.
Some advices won’t be big surprises—go for a whole foods diet, avoiding processed food, for example. Probably not a shocker.
Others are counterintuitive, but he explains how they work—exercising less while moving more, for instance. Sounds crazy, but we assure you there’s a metabolic explanation for it that’s beyond the scope of this review. And there’s plenty more where that came from, too.
Bottom line: if your weight has been either slowly rising, or else very stable but at a higher point than you’d like, Dr. Chatterjee can help you move the bar back to where you want it—and keep it there.
Share This Post
-
Do we need animal products to be healthy?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do we need animal products to be healthy?
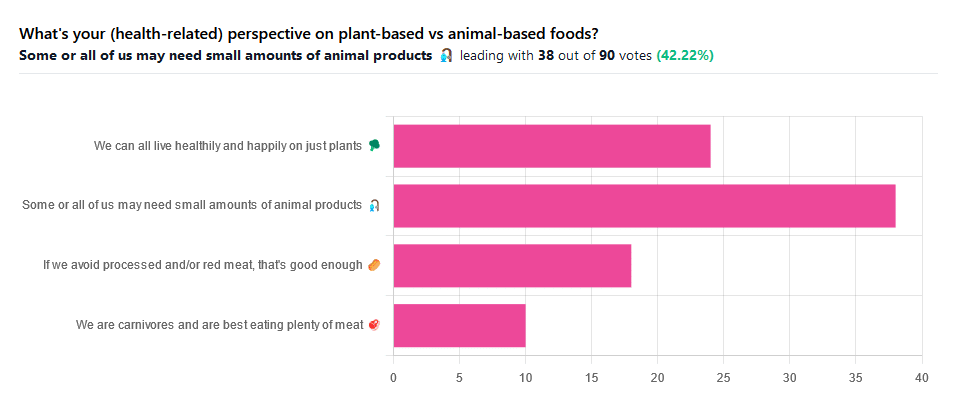
We asked you for your (health-related) perspective on plant-based vs anima-based foods, and got the above-pictured spread of answers.
“Some or all of us may need small amounts of animal products” came out on top with more votes than the two more meat-eatery options combined, and the second most popular option was the hard-line “We can all live healthily and happily on just plants”.
Based on these answers, it seems our readership has quite a lot of vegans, vegetarians, and perhaps “flexitarians” who just have a little of animal products here and there.
Perhaps we should have seen this coming; the newsletter is “10almonds”, not “10 rashers of bacon”, after all.
But what does the science say?
We are carnivores and are best eating plenty of meat: True or False?
False. Let’s just rip the band-aid off for this one.
In terms of our anatomy and physiology, we are neither carnivores nor herbivores:
- We have a mid-length digestive tract (unlike carnivores and herbivores who have short and long ones, respectively)
- We have a mouthful of an assortment of teeth; molars and premolars for getting through plants from hard nuts to tough fibrous tubers, and we have incisors for cutting into flesh and (vestigial, but they’re there) canines that really serve us no purpose now but would have been a vicious bite when they were bigger, like some other modern-day primates.
- If we look at our closest living relatives, the other great apes, they are mostly frugivores (fruit-eaters) who supplement their fruity diet with a small quantity of insects and sometimes other small animals—of which they’ll often eat only the fatty organ meat and discard the rest.
And then, there’s the health risks associated with meat. We’ll not linger on this as we’ve talked about it before, but for example:
- Processed Meat Consumption and the Risk of Cancer: A Critical Evaluation of the Constraints of Current Evidence from Epidemiological Studies
- Red Meat Consumption (Heme Iron Intake) and Risk for Diabetes and Comorbidities?
- Health Risks Associated with Meat Consumption: A Review of Epidemiological Studies
- Associations of Processed Meat, Unprocessed Red Meat, Poultry, or Fish Intake With Incident Cardiovascular Disease and All-Cause Mortality
- Meat consumption: Which are the current global risks? A review of recent (2010-2020) evidences
If we avoid processed and/or red meat, that’s good enough: True or False?
True… Ish.
Really this one depends on one’s criteria for “good enough”. The above-linked studies, and plenty more like them, give the following broad picture:
- Red and/or processed meats are unequivocally terrible for the health in general
- Other mammalian meats, such as from pigs, are really not much better
- Poultry, on the other hand, the science is less clear on; the results are mixed, and thus so are the conclusions. The results are often barely statistically significant. In other words, when it comes to poultry, in the matter of health, the general consensus is that you can take it or leave it and will be fine. Some studies have found firmly for or against it, but the consensus is a collective scientific shrug.
- Fish, meanwhile, has almost universally been found to be healthful in moderation. You may have other reasons for wanting to avoid it (ethics, environmentalism, personal taste) but those things are beyond the scope of this article.
Some or all of us may need small amounts of animal products: True or False?
True! With nuances.
Let’s divide this into “some” and “all”. Firstly, some people may have health conditions and/or other mitigating circumstances that make an entirely plant-based diet untenable.
We’re going light on quotations from subscriber comments today because otherwise this article will get a bit long, but here’s a great example that’s worth quoting, from a subscriber who voted for this option:
❝I have a rare genetic disease called hereditary fructose intolerance. It means I lack the enzyme, Aldolase B, to process fructose. Eating fruits and veggies thus gives me severe hypoglycemia. I also have anemia caused by two autoimmune diseases, so I have to eat meat for the iron it supplies. I also supplement with iron pills but the pills alone can’t fix the problem entirely.❞
And, there’s the thing. Popular vegan talking-points are very good at saying “if you have this problem, this will address it; if you have that problem, that will address it”, etc. For every health-related objection to a fully plant-based diet there’s a refutation… Individually.
But actual real-world health doesn’t work like that; co-morbidities are very common, and in some cases, like our subscriber above, one problem undermines the solution to another. Add a third problem and by now you really just have to do what you need to do to survive.
For this reason, even the Vegan Society’s definition of veganism includes the clause “so far as is possible and practicable”.
Now, as for the rest of us “all”.
What if we’re really healthy and are living in optimal circumstances (easy access to a wide variety of choice of food), can we live healthily and happily just on plants?
No—on a technicality.
Vegans famously need to supplement vitamin B12, which is not found in plants. Ironically, much of the B12 in animal products comes from the animals themselves being given supplements, but that’s another matter. However, B12 can also be enjoyed from yeast. Popular options include the use of yeast extract (e.g. Marmite) and/or nutritional yeast in cooking.
Yeast is a single-celled microorganism that’s taxonomically classified as a fungus, even though in many ways it behaves like an animal (which series of words may conjure an amusing image, but we mean, biologically speaking).
However, it’s also not technically a plant, hence the “No—on a technicality”
Bottom line:
By nature, humans are quite versatile generalists when it comes to diet:
- Most of us can live healthily and happily on just plants if we so choose.
- Some people cannot, and will require varying kinds (and quantities) of animal products.
- As for red and/or processed meats, we’re not the boss of you, but from a health perspective, the science is clear: unless you have a circumstance that really necessitates it, just don’t.
- Same goes for pork, which isn’t red and may not be processed, but metabolically it’s associated with the same problems.
- The jury is out on poultry, but it strongly appears to be optional, healthwise, without making much of a difference either way
- Fish is roundly considered healthful in moderation. Enjoy it if you want, don’t if you don’t.
Share This Post
-
Is fluoride really linked to lower IQ, as a recent study suggested? Here’s why you shouldn’t worry
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fluoride is a common natural element found in water, soil, rocks and food. For the past several decades, fluoride has also been a cornerstone of dentistry and public health, owing to its ability to protect against tooth decay.
Water fluoridation is a population-based program where a precise, small amount of fluoride is added to public drinking water systems. Water fluoridation began in Australia in the 1950s. Today more than 90% of Australia’s population has access to fluoridated tap water.
But a recently published review found higher fluoride exposure is linked to lower intelligence quotient (IQ) in children. So how can we interpret the results?
Much of the data analysed in this review is poor quality. Overall, the findings don’t give us reason to be concerned about the fluoride levels in our water supplies.
TinnaPong/Shutterstock Not a new controversy
Tooth decay (also known as caries or cavities) can have negative effects on dental health, overall health and quality of life. Fluoride strengthens our teeth, making them more resistant to decay. There is scientific consensus water fluoridation is a safe, effective and equitable way to improve oral health.
Nonetheless, water fluoridation has historically been somewhat controversial.
A potential link between fluoride and IQ (and cognitive function more broadly) has been a contentious topic for more than a decade. This started with reports from studies in China and India.
But it’s important to note these studies were limited by poor methodology, and water in these countries had high levels of natural fluoride when the studies were conducted – many times higher than the levels recommended for water fluoridation programs. Also, the studies did not control for other contaminants in the water supply.
Recent reviews focusing on the level of fluoride used in water fluoridation have concluded fluoride is not linked to lower IQ.
Despite this, some have continued to raise concerns. The United States National Toxicology Program conducted a review of the potential link. However, this review did not pass the quality assessment by the US National Academies of Sciences, Engineering and Medicine due to significant limitations in the conduct of the review.
The authors followed through with their study and published it as an independent publication in the journal JAMA Paediatrics last week. This is the study which has been generating media attention in recent days.
What the study did
This study was a systematic review and meta-analysis, where the researchers evaluated 74 studies from different parts of the world.
A total of 52 studies were rated as having a high risk of bias, and 64 were cross-sectional studies, which often can’t provide evidence of causal relationship.
Most of the studies were conducted in developing countries, such as China (45), India (12), Iran (4), Mexico (4) and Pakistan (2). Only a few studies were conducted in developed countries with established public water systems, where regular monitoring and treatment of drinking water ensures it’s free from contaminants.
The vast majority of studies were conducted in populations with high to very high levels of natural fluoride and without water fluoridation programs, where fluoride levels are controlled within recommended levels.
The study concluded there was an inverse association between fluoride levels and IQ in children. This means those children who had a higher intake of fluoride had lower IQ scores than their counterparts.
Water fluoridation programs reduce the occurrence of cavities. Drazen Zigic/Shutterstock Limitations to consider
While this review combined many studies, there are several limitations that cast serious doubt over its conclusion. Scientists immediately raised concerns about the quality of the review, including in a linked editorial published in JAMA.
The low quality of the majority of included studies is a major concern, rendering the quality of the review equally low. Importantly, most studies were not relevant to the recommended levels of fluoride in water fluoridation programs.
Several included studies from countries with controlled public water systems (Canada, New Zealand, Taiwan) showed no negative effects. Other recent studies from comparable populations (such as Spain and Denmark) also have not shown any negative effect of fluoride on IQ, but they were not included in the meta-analysis.
For context, the review found there was no significant association with IQ when fluoride was measured at less than 1.5mg per litre in water. In Australia, the recommended levels of fluoride in public water supplies range from 0.6 to 1.1 mg/L.
Also, the primary outcome, IQ score, is difficult to collect. Most included studies varied widely on the methods used to collect IQ data and did not specify their focus on ensuring reliable and consistent IQ data. Though this is a challenge in most research on this topic, the significant variations between studies in this review raise further doubts about the combined results.
No cause for alarm
Although no Australian studies were included in the review, Australia has its own studies investigating a potential link between fluoride exposure in early childhood and child development.
I’ve been involved in population-based longitudinal studies investigating a link between fluoride and child behavioural development and executive functioning and between fluoride and IQ. The IQ data in the second study were collected by qualified, trained psychologists – and calibrated against a senior psychologist – to ensure quality and consistency. Both studies have provided strong evidence fluoride exposure in Australia does not negatively impact child development.
This new review is not a reason to be concerned about fluoride levels in Australia and other developed countries with water fluoridation programs. Fluoride remains important in maintaining the public’s dental health, particularly that of more vulnerable groups.
That said, high and uncontrolled levels of fluoride in water supplies in less developed countries warrant attention. There are programs underway in a range of countries to reduce natural fluoride to the recommended level.
Loc Do, Professor of Dental Public Health, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
An Underrated Tool Against Alzheimer’s
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia in general, and Alzheimer’s in particular, affects a lot of people, and probably even more than the stats show, because some (estimated to be: about half) will go undiagnosed and thus unreported:
Alzheimer’s: The Bad News And The Good
At 10almonds, we often talk about brain health, whether from a nutrition standpoint or other lifestyle factors. For nutrition, by the way, check out:
Today we’ll be looking at some new science for an underrated tool:
Bilingualism as protective factor
It’s well-known that bilingualism offers brain benefits, but most people would be hard-pressed to name what, specifically, those brain benefits are.
As doctors Kristina Coulter and Natalie Phillips found in a recent study, one of the measurable benefits may be a defense against generalized (i.e. not necessarily language-related) memory loss Alzheimer’s disease.
Specifically,
❝We used surface-based morphometry methods to measure cortical thickness and volume of language-related and AD-related brain regions. We did not observe evidence of brain reserve in language-related regions.
However, reduced hippocampal volume was observed for monolingual, but not bilingual, older adults with AD. Thus, bilingualism is hypothesized to contribute to reserve in the form of brain maintenance in the context of AD.❞
Read in full: Bilinguals show evidence of brain maintenance in Alzheimer’s disease
This is important, because while language is processed in various parts of the brain beyond the scope of this article, the hippocampi* are where memory is stored.
*usually mentioned in the singular as “hippocampus”, but you have one on each side, unless some terrible accident or incident befell you.
What this means in practical terms: these results suggest that being bilingual means we will retain more of our capacity for memory, even if we get Alzheimer’s disease, than people who are monolingual.
Furthermore, while we’re talking practicality:
❝…our subsample may be characterized as mostly late bilinguals (i.e., learning an L2 after age 5), having moderate self-reported L2 ability, and relatively few participants reporting daily L2 use (33 out of 119)❞
(L2 = second language)
This is important, because it means you don’t have to have grown up speaking multiple languages, you don’t even have to speak it well, and you don’t have to be using your second language(s) on a daily basis, to enjoy benefits. Merely having them in your head appears to be sufficient to trigger the brain to go “oh, we need to boost and maintain the hippocampal volume”.
We would hypothesize that using second language(s) regularly and/or speaking second language(s) well offers additional protection, and the data would support this if it weren’t for the fact that the sample sizes for daily and high-level speakers are a bit small to draw conclusions.
But the important part is: simply knowing another language, including if you literally just learned it later in life, is already protective of hippocampal volume in the context of Alzheimer’s disease.
Here’s a pop-science article about the study, that goes into it in more detail than we have room to here:
Bilingualism linked to greater brain resilience in older adults
Want to learn a new language?
Here are some options where you can get going right away:
If you are thinking “sounds good, but learning a language is too much work”, then that is why we included that third option there. It’s specifically for one language, and that language is Esperanto, arguably the world’s easiest language and specifically designed to be super quick and easy to get good at. Also, it’s free!
Do, kial ne lerni novan lingvon rapide kaj facile? 😉
Want to know more?
For ways to reduce your overall Alzheimer’s risk according to science, check out:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Montana Eyes $30M Revamp of Mental Health, Developmental Disability Facilities
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
HELENA, Mont. — As part of a proposed revamping of the state’s behavioral health system, Republican Gov. Greg Gianforte’s administration is looking into moving a facility for people with developmental disabilities, beefing up renovations at the Montana State Hospital, and creating a Helena unit of that psychiatric hospital.
The changes, backers say, would fill gaps in services and help people better prepare for life outside of the locked, secure setting of the two state facilities before they reenter their own communities.
“I think part of the theme is responsibly moving people in and out of the state facilities so that we create capacity and have people in the appropriate places,” state Sen. Dave Fern (D-Whitefish) said of the proposed capital projects during a recent interview.
Fern served on the Behavioral Health System for Future Generations Commission, a panel created by a 2023 law to suggest how to spend $300 million to revamp the system. The law set aside the $300 million for improving state services for people with mental illness, substance abuse disorders, and developmental disabilities.
Gianforte’s proposed budget for the next two years would spend about $100 million of that fund on 10 other recommendations from the commission. The capital projects are separate ideas for using up to $32.5 million of the $75 million earmarked within the $300 million pool of funds for building new infrastructure or remodeling existing buildings.
The state Department of Public Health and Human Services and consultants for the behavioral health commission presented commission members with areas for capital investments in October. In December, the commission authorized state health department director Charlie Brereton to recommend the following projects to Gianforte:
- Move the 12-bed Intensive Behavior Center for people with developmental disabilities out of Boulder, possibly to either Helena or Butte, at an estimated cost of up to $13.3 million.
- Establish a “step-down” facility of about 16 beds, possibly on the campus of Shodair Children’s Hospital in Helena, to serve adults who have been committed to the Montana State Hospital but no longer need the hospital’s intensive psychiatric services.
- Invest $19.2 million to upgrade the Montana State Hospital’s infrastructure and buildings at Warm Springs, on top of nearly $16 million appropriated in 2023 for renovations already underway there in an effort to regain federal certification of the facility.
The state Architecture & Engineering Division is reviewing the health department’s cost estimates and developing a timeline for the projects so the information can be sent to the governor. Gianforte ultimately must approve the projects.
Health department officials have said they plan to take the proposals to legislative committees as needed. “With Commission recommendation and approval from the governor, the Department believes that it has the authority to proceed with capital project expenditures but must secure additional authority from the Legislature to fund operations into future biennia,” said department spokesperson Jon Ebelt.
The department outlined its facility plans to the legislature’s health and human services budget subcommittee on Jan. 22 as part of a larger presentation on the commission’s work and the 10 noncapital proposals in the governor’s budget. Time limits prevented in-depth discussion and public comment on the facility-related ideas.
One change the commission didn’t consider: moving the Montana State Hospital to a more populated area from its rural and relatively remote location near Anaconda, in southwestern Montana, in an attempt to alleviate staffing shortages.
“The administration is committed to continuing to invest in MSH as it exists today,” Brereton told the commission in October, referring to the Montana State Hospital.
The hospital provides treatment to people with mental illness who have been committed to the state’s custody through a civil or criminal proceeding. It’s been beset by problems, including the loss of federal Medicaid and Medicare funding due to decertification by the federal government in April 2022, staffing issues that have led to high use of expensive traveling health care providers, and turnover in leadership.
State Sen. Chris Pope (D-Bozeman) was vice chair of a separate committee that met between the 2023 and 2025 legislative sessions and monitored progress toward a 2023 legislative mandate to transition patients with dementia out of the state hospital. He agreed in a recent interview that improving — not moving — MSH is a top priority for the system right now.
“Right now, we have an institution that is failing and needs to be brought back into the modern age, where it is located right now,” he said after ticking off a list of challenges facing the hospital.
State Sen. John Esp (R-Big Timber) also noted at the October commission meeting that moving the hospital was likely to run into resistance in any community considered for a new facility.
Fern, the Whitefish senator, questioned in October whether similar concerns might exist for moving the Intensive Behavior Center out of Boulder. For more than 130 years, the town 30 miles south of Helena has been home, in one form or another, to a state facility for people with developmental disabilities. But Brereton said he believes relocation could succeed with community and stakeholder involvement.
The 12-bed center in Boulder serves people who have been committed by a court because their behaviors pose an immediate risk of serious harm to themselves or others. It’s the last residential building for people with developmental disabilities on the campus of the former Montana Developmental Center, which the legislature voted in 2015 to close.
Drew Smith, a consultant with the firm Alvarez & Marsal, told the commission in October that moving the facility from the town of 1,300 to a bigger city such as Helena or Butte would provide access to a larger labor pool, possibly allow a more homelike setting for residents, and open more opportunities for residents to interact with the community and develop skills for returning to their own communities.
Ideally, Brereton said, the center would be colocated with a new facility included in the governor’s proposed budget, for crisis stabilization services to people with developmental disabilities who are experiencing significant behavioral health issues.
Meanwhile, the proposed subacute facility with up to 16 beds for state hospital patients would provide a still secure but less structured setting for people who no longer need intensive treatment at Warm Springs but aren’t yet ready to be discharged from the hospital’s care. Brereton told the commission in October the facility would essentially serve as a less restrictive “extension” of the state hospital. He also said the agency would like to contract with a company to staff the subacute facility.
Health department officials don’t expect the new facility to involve any construction costs. Brereton has said the agency believes an existing building on the Shodair campus would be a good spot for it.
The state began leasing the building Nov. 1 for use by about 20 state hospital patients displaced by the current remodeling at Warm Springs — a different purpose than the proposed subacute facility.
Shodair CEO Craig Aasved said Shodair hasn’t committed to having the state permanently use the building as the step-down facility envisioned by the agency and the commission.
But Brereton said the option is attractive to the health department now that the building has been set up and licensed to serve adults.
“It seems like a natural place to start,” he told the commission in December, “and we don’t mind that it’s in our backyard here in Helena.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
WHO Overturns Dogma on Airborne Disease Spread. The CDC Might Not Act on It.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The World Health Organization has issued a report that transforms how the world understands respiratory infections like covid-19, influenza, and measles.
Motivated by grave missteps in the pandemic, the WHO convened about 50 experts in virology, epidemiology, aerosol science, and bioengineering, among other specialties, who spent two years poring through the evidence on how airborne viruses and bacteria spread.
However, the WHO report stops short of prescribing actions that governments, hospitals, and the public should take in response. It remains to be seen how the Centers for Disease Control and Prevention will act on this information in its own guidance for infection control in health care settings.
The WHO concluded that airborne transmission occurs as sick people exhale pathogens that remain suspended in the air, contained in tiny particles of saliva and mucus that are inhaled by others.
While it may seem obvious, and some researchers have pushed for this acknowledgment for more than a decade, an alternative dogma persisted — which kept health authorities from saying that covid was airborne for many months into the pandemic.
Specifically, they relied on a traditional notion that respiratory viruses spread mainly through droplets spewed out of an infected person’s nose or mouth. These droplets infect others by landing directly in their mouth, nose, or eyes — or they get carried into these orifices on droplet-contaminated fingers. Although these routes of transmission still happen, particularly among young children, experts have concluded that many respiratory infections spread as people simply breathe in virus-laden air.
“This is a complete U-turn,” said Julian Tang, a clinical virologist at the University of Leicester in the United Kingdom, who advised the WHO on the report. He also helped the agency create an online tool to assess the risk of airborne transmission indoors.
Peg Seminario, an occupational health and safety specialist in Bethesda, Maryland, welcomed the shift after years of resistance from health authorities. “The dogma that droplets are a major mode of transmission is the ‘flat Earth’ position now,” she said. “Hurray! We are finally recognizing that the world is round.”
The change puts fresh emphasis on the need to improve ventilation indoors and stockpile quality face masks before the next airborne disease explodes. Far from a remote possibility, measles is on the rise this year and the H5N1 bird flu is spreading among cattle in several states. Scientists worry that as the H5N1 virus spends more time in mammals, it could evolve to more easily infect people and spread among them through the air.
Traditional beliefs on droplet transmission help explain why the WHO and the CDC focused so acutely on hand-washing and surface-cleaning at the beginning of the pandemic. Such advice overwhelmed recommendations for N95 masks that filter out most virus-laden particles suspended in the air. Employers denied many health care workers access to N95s, insisting that only those routinely working within feet of covid patients needed them. More than 3,600 health care workers died in the first year of the pandemic, many due to a lack of protection.
However, a committee advising the CDC appears poised to brush aside the updated science when it comes to its pending guidance on health care facilities.
Lisa Brosseau, an aerosol expert and a consultant at the Center for Infectious Disease Research and Policy in Minnesota, warns of a repeat of 2020 if that happens.
“The rubber hits the road when you make decisions on how to protect people,” Brosseau said. “Aerosol scientists may see this report as a big win because they think everything will now follow from the science. But that’s not how this works and there are still major barriers.”
Money is one. If a respiratory disease spreads through inhalation, it means that people can lower their risk of infection indoors through sometimes costly methods to clean the air, such as mechanical ventilation and using air purifiers, and wearing an N95 mask. The CDC has so far been reluctant to press for such measures, as it updates foundational guidelines on curbing airborne infections in hospitals, nursing homes, prisons, and other facilities that provide health care. This year, a committee advising the CDC released a draft guidance that differs significantly from the WHO report.
Whereas the WHO report doesn’t characterize airborne viruses and bacteria as traveling short distances or long, the CDC draft maintains those traditional categories. It prescribes looser-fitting surgical masks rather than N95s for pathogens that “spread predominantly over short distances.” Surgical masks block far fewer airborne virus particles than N95s, which cost roughly 10 times as much.
Researchers and health care workers have been outraged about the committee’s draft, filing letters and petitions to the CDC. They say it gets the science wrong and endangers health. “A separation between short- and long-range distance is totally artificial,” Tang said.
Airborne viruses travel much like cigarette smoke, he explained. The scent will be strongest beside a smoker, but those farther away will inhale more and more smoke if they remain in the room, especially when there’s no ventilation.
Likewise, people open windows when they burn toast so that smoke dissipates before filling the kitchen and setting off an alarm. “You think viruses stop after 3 feet and drop to the ground?” Tang said of the classical notion of distance. “That is absurd.”
The CDC’s advisory committee is comprised primarily of infection control researchers at large hospital systems, while the WHO consulted a diverse group of scientists looking at many different types of studies. For example, one analysis examined the puff clouds expelled by singers, and musicians playing clarinets, French horns, saxophones, and trumpets. Another reviewed 16 investigations into covid outbreaks at restaurants, a gym, a food processing factory, and other venues, finding that insufficient ventilation probably made them worse than they would otherwise be.
In response to the outcry, the CDC returned the draft to its committee for review, asking it to reconsider its advice. Meetings from an expanded working group have since been held privately. But the National Nurses United union obtained notes of the conversations through a public records request to the agency. The records suggest a push for more lax protection. “It may be difficult as far as compliance is concerned to not have surgical masks as an option,” said one unidentified member, according to notes from the committee’s March 14 discussion. Another warned that “supply and compliance would be difficult.”
The nurses’ union, far from echoing such concerns, wrote on its website, “The Work Group has prioritized employer costs and profits (often under the umbrella of ‘feasibility’ and ‘flexibility’) over robust protections.” Jane Thomason, the union’s lead industrial hygienist, said the meeting records suggest the CDC group is working backward, molding its definitions of airborne transmission to fit the outcome it prefers.
Tang expects resistance to the WHO report. “Infection control people who have built their careers on this will object,” he said. “It takes a long time to change people’s way of thinking.”
The CDC declined to comment on how the WHO’s shift might influence its final policies on infection control in health facilities, which might not be completed this year. Creating policies to protect people from inhaling airborne viruses is complicated by the number of factors that influence how they spread indoors, such as ventilation, temperature, and the size of the space.
Adding to the complexity, policymakers must weigh the toll of various ailments, ranging from covid to colds to tuberculosis, against the burden of protection. And tolls often depend on context, such as whether an outbreak happens in a school or a cancer ward.
“What is the level of mortality that people will accept without precautions?” Tang said. “That’s another question.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: