6 Kinds Of Drinks That Hasten Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. William Li, most well-known for his diabetes expertise (remember that there are clear associations between diabetes and dementia), discusses drinks you might want to skip:
Here’s to your good health
The 6 kinds of drink are:
- Alcohol which is bad for pretty much everything and this is no exception. Can cause a deficiency of thiamine, brain-shrinking, neuroinflammation, oxidative stress, and resultant neuron damage.
- Soda / diet soda, the former of which is bad for the diabetes-dementia connection, and the latter of which is also usually (depends on the sweetener) harmful to the gut and thus the gut-brain connection.
- Fruit juices, especially if processed, as the high sugar and zero or nearly-zero fiber can lead to insulin resistance, affecting the brain’s energy processing. In particular, fruit juice drinks sweetened with high-fructose corn syrup (HFCS) can accumulated as fat in the brain (due to how the body processes fructose in the absence of fiber to slow it down), impacting cognition.
- Energy drinks, being basically the same as soda / diet soda, just now with added caffeine too.
- [Caffeinated] late-night coffee, can (shocking nobody) disrupt sleep, and chronic sleep deprivation contributes to the build-up of harmful brain plaques.
- Sports drinks, which (unless you’re super-sure about everything on the label; there are some good sports drinks out there) often contain HFCS in the US, along with various other additives that may not always be great for you. Also, the sodium content of electrolyte drinks are fine if you genuinely are actively sweating it out, but otherwise, can lead to high blood pressure, which is itself a dementia risk factor.
Better options include:
- decaffeinated coffee (or coffee enjoyed in the early afternoon)
- green tea
- turmeric-based drinks
Dr. Li mentions turmeric milk drinks, but unfermented dairy is generally inflammatory, so better to make it kefir (fermented milk drink) or plant-based. Or just have a turmeric tea; that works too.
Dr. Li also mentions berry smoothies, which are not nearly as bad as fruit juice, but still not as good as eating whole berries.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Body Scrubs: Benefits, Risks, and Guidance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I was wondering whether I should be using a body scrub in the shower, rather than just soap. What should guide me in the choice of a body scrub, and are there any risks to be aware of?❞
Body scrubs are great for giving skin a healthy glow, but are best used sparingly—over-exfoliation leads to the opposite effect (unhappy skin, premature skin aging, etc).
As for contents:
- microplastics are now banned in most places, but you might want to check any products (and their containers!) are BPA-free, pthalate free, etc.
- fragrances in body scrubs are usually a bad idea, and many essential oils have been shown to be endocrine-disruptors, which you do not want:
About the microplastics, harmful artificial chemicals in general, and what constitutes “etc”:
About the fragrances’ (including “natural” essential oils’) endocrine-disrupting shenanigans:
Endocrine-disrupting chemicals: an Endocrine Society scientific statement
So, what might you want to use instead?
If you’re feeling adventurous, you might like to try treating yourself to a pineapple-based mask instead (a muslin cloth soaked in pineapple juice will work just fine; please don’t waterboard yourself though), as the bromelain enzymes (found very generously in pineapple juice) break down dead cells without the need for scrubbing.
Another option is a homemade salt- or sugar-scrub. Put your salt or sugar into a jar, add enough warm water to cover it, leave it for about a day, adding more water if it seems in danger of drying out, until it recrystallizes with a high water content keeping it malleable to the touch; congratulations, you now have a very simple scrub. This should still not be used more than, say, once per week, though.
Last but not least, you might consider investing in a konjac sponge; they gently remove dead skin without damaging living skin. Here’s an example product on Amazon, for your convenience
For more on gentle-yet-effective skincare, you might like to read:
Clean: The New Science of Skin and the Beauty of Doing Less
Enjoy!
Share This Post
-
Women are less likely to receive CPR than men. Training on manikins with breasts could help
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If someone’s heart suddenly stops beating, they may only have minutes to live. Doing CPR (cardiopulmonary resusciation) can increase their chances of survival. CPR makes sure blood keeps pumping, providing oxygen to the brain and vital organs until specialist treatment arrives.
But research shows bystanders are less likely to intervene to perform CPR when that person is a woman. A recent Australian study analysed 4,491 cardiac arrests between 2017–19 and found bystanders were more likely to give CPR to men (74%) than women (65%).
Could this partly be because CPR training dummies (known as manikins) don’t have breasts? Our new research looked at manikins available worldwide to train people in performing CPR and found 95% are flat-chested.
Anatomically, breasts don’t change CPR technique. But they may influence whether people attempt it – and hesitation in these crucial moments could mean the difference between life and death.
Pixel-Shot/Shutterstock Heart health disparities
Cardiovascular diseases – including heart disease, stroke and cardiac arrest – are the leading cause of death for women across the world.
But if a woman has a cardiac arrest outside hospital (meaning her heart stops pumping properly), she is 10% less likely to receive CPR than a man. Women are also less likely to survive CPR and more likely to have brain damage following cardiac arrests.
Bystanders are less likely to intervene if a woman needs CPR, compared to a man. doublelee/Shutterstock These are just some of many unequal health outcomes women experience, along with transgender and non-binary people. Compared to men, their symptoms are more likely to be dismissed or misdiagnosed, or it may take longer for them to receive a diagnosis.
Bystander reluctance
There is also increasing evidence women are less likely to receive CPR compared to men.
This may be partly due to bystander concerns they’ll be accused of sexual harassment, worry they might cause damage (in some cases based on a perception women are more “frail”) and discomfort about touching a woman’s breast.
Bystanders may also have trouble recognising a woman is experiencing a cardiac arrest.
Even in simulations of scenarios, researchers have found those who intervened were less likely to remove a woman’s clothing to prepare for resuscitation, compared to men. And women were less likely to receive CPR or defibrillation (an electric charge to restart the heart) – even when the training was an online game that didn’t involve touching anyone.
There is evidence that how people act in resuscitation training scenarios mirrors what they do in real emergencies. This means it’s vital to train people to recognise a cardiac arrest and be prepared to intervene, across genders and body types.
Skewed to male bodies
Most CPR training resources feature male bodies, or don’t specify a sex. If the bodies don’t have breasts, it implies a male default.
For example, a 2022 study looking at CPR training across North, Central and South America, found most manikins available were white (88%), male (94%) and lean (99%).
It’s extremely rare for a manikin to have breasts or a larger body. M Isolation photo/Shutterstock These studies reflect what we see in our own work, training other health practitioners to do CPR. We have noticed all the manikins available to for training are flat-chested. One of us (Rebecca) found it difficult to find any training manikins with breasts.
A single manikin with breasts
Our new research investigated what CPR manikins are available and how diverse they are. We identified 20 CPR manikins on the global market in 2023. Manikins are usually a torso with a head and no arms.
Of the 20 available, five (25%) were sold as “female” – but only one of these had breasts. That means 95% of available CPR training manikins were flat-chested.
We also looked at other features of diversity, including skin tone and larger bodies. We found 65% had more than one skin tone available, but just one was a larger size body. More research is needed on how these aspects affect bystanders in giving CPR.
Breasts don’t change CPR technique
CPR technique doesn’t change when someone has breasts. The barriers are cultural. And while you might feel uncomfortable, starting CPR as soon as possible could save a life.
Signs someone might need CPR include not breathing properly or at all, or not responding to you.
To perform effective CPR, you should:
- put the heel of your hand on the middle of their chest
- put your other hand on the top of the first hand, and interlock fingers (keep your arms straight)
- press down hard, to a depth of about 5cm before releasing
- push the chest at a rate of 100-120 beats per minute (you can sing a song) in your head to help keep time!)
https://www.youtube.com/embed/Plse2FOkV4Q?wmode=transparent&start=94 An example of how to do CPR – with a flat-chested manikin.
What about a defibrillator?
You don’t need to remove someone’s bra to perform CPR. But you may need to if a defibrillator is required.
A defibrillator is a device that applies an electric charge to restore the heartbeat. A bra with an underwire could cause a slight burn to the skin when the debrillator’s pads apply the electric charge. But if you can’t remove the bra, don’t let it delay care.
What should change?
Our research highlights the need for a range of CPR training manikins with breasts, as well as different body sizes.
Training resources need to better prepare people to intervene and perform CPR on people with breasts. We also need greater education about women’s risk of getting and dying from heart-related diseases.
Jessica Stokes-Parish, Assistant Professor in Medicine, Bond University and Rebecca A. Szabo, Honorary Senior Lecturer in Critical Care and Obstetrics, Gynaecology and Newborn Health, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
14 Powerful Strategies To Prevent Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia risk starts climbing very steeply after the age of 65, but it’s not entirely predetermined. Dr. Brad Stanfield, a primary care physician, has insights:
The strategies
We’ll not keep them a mystery; they are:
- Cognitive stimulation: which means genuinely challenging mental activities using a variety of mental faculties. This will usually mean that anything that is just “same old, same old” all the time will stop giving benefits after a short while once it becomes rote, and you’ll need something harder and/or different.
- Hearing health: being unable to participate in conversations increases dementia risk; hearing aids can help.
- Eyesight health: similar to the above; regular eye tests are good, and the use of glasses where appropriate.
- Depression management: midlife depression is linked to later life dementia, likely in large part due to social isolation and a lack of stimulation, but either way, treating depression earlier reduces later dementia risk.
- Exercising regularly: what’s good for the heart is good for the brain; the brain is a hungry organ and the blood is what feeds it (and removes things that shouldn’t be there)
- Head injury avoidance: even mild head injuries can cause problems down the road. Protecting one’s head in sports, and even while casually cycling, is important.
- Smoking cessation: just don’t smoke; if you smoke, make it a top priority to quit unless you are given direct strong medical advice to the contrary (there are cases, few and far between, whereby quitting smoking genuinely needs to be deferred until after something else is dealt with first, but they are a lot rarer than a lot of people who are simply afraid of quitting would like to believe)
- Cholesterol management: again, healthy blood means a healthy brain, and that goes for triglycerides too.
- Weight management: obesity, especially waist to hip ratio (indicating visceral abdominal fat specifically) is associated with many woes, including dementia.
- Diabetes management: once again, healthy blood means a healthy brain, and that goes for blood sugar management too.
- Blood pressure management: guess what, healthy blood still means a healthy brain, and that goes for blood pressure too.
- Alcohol reduction/cessation: alcohol is bad for pretty much everything, and for most people who drink, quitting is probably the top thing to do after quitting smoking.
- Social engagement: while we all may have our different preferences on a scale of introversion to extroversion, we are fundamentally a social species and thrive best with social contact, even if it’s just a few people.
- Air pollution reduction: avoiding pollutants, and filtering the air we breathe where pollutants are otherwise unavoidable, makes a measurable difference to brain health outcomes.
For more information on all of these (except the last two, which really he only mentions in passing), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Reduce Your Alzheimer’s Risk ← our own main feature on the topic
Take care!
Share This Post
Related Posts
-
Avoid Knee Surgery With This Proven Strategy (Over-50s Specialist Physio)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A diagnosis of knee arthritis can be very worrying, but it doesn’t necessarily mean a knee replacement surgery is inevitable. Here’s how to keep your knee better, for longer (and potentially, for life):
Flexing your good health
You know we wouldn’t let that “proven” go by unchallenged if it weren’t, so what’s the evidence for it? Research (papers linked in the video description) showed 70% of patients (so, not 100%, but 70% is good odds and a lot better than the alternative) with mild to moderate knee arthritis avoided surgery after following a specific protocol—the one we’re about to describe.
The key strategy is to focus on strengthening the quadriceps muscles for joint protection, as strong quads correlate with reduced pain. However, a full range of motion in the knee is essential for optimal quad function, so that needs attention too, and in fact is foundational (can’t strengthen a quadriceps that doesn’t have a range of motion available to it):
Steps to follow:
- Improve knee extension:
- Passive knee extension exercise: gently press your knee down while lying flat, to increase straightening.
- Weighted heel props: use light weights to encourage gradual knee straightening.
- Enhance knee flexion:
- Use a towel to gently pull the knee towards the body to improve bending range.
Regular practice (multiple times daily) leads to improved knee function and pain relief. Exercises should be performed gently and without pain, aiming for consistent, gradual progress.And of course, if you do experience pain, it is recommend to consult with a local physiotherapist for more personalized guidance.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Treat Your Own Knee – by Robin McKenzie
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Improve knee extension:
-
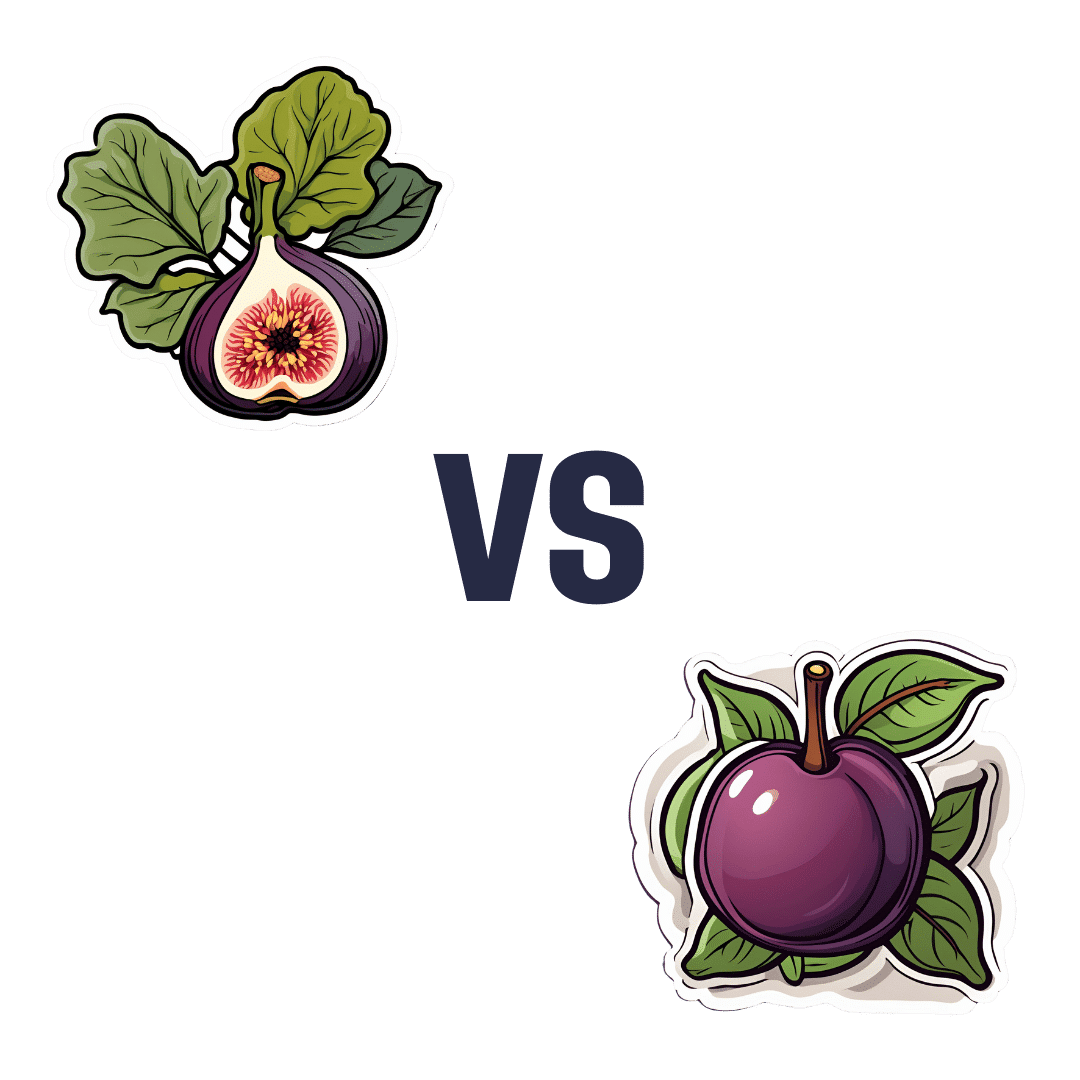
Figs vs Plums – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing figs to plums, we picked the figs.
Why?
In terms of macros, figs have more protein, carbs, and fiber; the glycemic index is about equal so we’ll call this category either a tie, or a nominal win for figs (as the “more food per food” option).
In the category of vitamins, figs have more of vitamins B1, B2, B3, B5, B6, B7, B9, and choline, while plums have more of vitamins A, C, E, and K. We may subjectively prefer one set of vitamins or the other (depending on the rest of our diet, for example), but by the numbers, this is a 7:4 victory for figs.
When it comes to minerals, figs have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while plums are not higher in any minerals. An easy win for figs here.
Of course, enjoy either or both, but if you’re going to pick one for nutritional density, we say it’s figs, as illustrated scientifically below:
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Avoid Carer Burnout (Without Dropping Care)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Avoid Carer Burnout
Sometimes in life we find ourselves in a caregiving role.
Maybe we chose it. For example, by becoming a professional carer, or even just by being a parent.
Oftentimes we didn’t. Sometimes because our own parents now need care from us, or because a partner becomes disabled.
Philosophical note: an argument could be made for that latter also having been a pre-emptive choice; we probably at some point said words to the effect of “in sickness and in health”, hopefully with free will, and hopefully meant it. And of course, sometimes we enter into a relationship with someone who is already disabled.
But, we are not a philosophy publication, and will henceforth keep to the practicalities.
First: are you the right person?
Sometimes, a caregiving role might fall upon you unasked-for, and it’s worth considering whether you are really up for it. Are you in a position to be that caregiver? Do you want to be that caregiver?
It may be that you do, and would actively fight off anyone or anything that tried to stop you. If so, great, now you only need to make sure that you are actually in a position to provide the care in question.
It may be that you do want to, but your circumstances don’t allow you to do as good a job of it as you’d like, or it means you have to drop other responsibilities, or you need extra help. We’ll cover these things later.
It may be that you don’t want to, but you feel obliged, or “have to”. If that’s the case, it will be better for everyone if you acknowledge that, and find someone else to do it. Nobody wants to feel a burden, and nobody wants someone providing care to be resentful of that. The result of such is two people being miserable; that’s not good for anyone. Better to give the job to someone who actually wants to (a professional, if necessary).
So, be honest (first with yourself, then with whoever may be necessary) about your own preferences and situation, and take steps to ensure you’re only in a caregiving role that you have the means and the will to provide.
Second: are you out of your depth?
Some people have had a life that’s prepared them for being a carer. Maybe they worked in the caring profession, maybe they have always been the family caregiver for one reason or another.
Yet, even if that describes you… Sometimes someone’s care needs may be beyond your abilities. After all, not all care needs are equal, and someone’s condition can (and more often than not, will) deteriorate.
So, learn. Learn about the person’s condition(s), medications, medical equipment, etc. If you can, take courses and such. The more you invest in your own development in this regard, the more easily you will handle the care, and the less it will take out of you.
And, don’t be afraid to ask for help. Maybe the person knows their condition better than you, and certainly there’s a good chance they know their care needs best. And certainly, there are always professionals that can be contacted to ask for advice.
Sometimes, a team effort may be required, and there’s no shame in that either. Whether it means enlisting help from family/friends or professionals, sometimes “many hands make light work”.
Check out: Caregiver Action Network: Organizations Near Me
A very good resource-hub for help, advice, & community
Third: put your own oxygen mask on first
Like the advice to put on one’s own oxygen mask first before helping others (in the event of a cabin depressurization in an airplane), the rationale is the same here. You can’t help others if you are running on empty yourself.
As a carer, sometimes you may have to put someone else’s needs above yours, both in general and in the moment. But, you do have needs too, and cannot neglect them (for long).
One sleepless night looking after someone else is… a small sacrifice for a loved one, perhaps. But several in a row starts to become unsustainable.
Sometimes it will be necessary to do the best you can, and accept that you cannot do everything all the time.
There’s a saying amongst engineers that applies here too: “if you don’t schedule time for maintenance, your equipment will schedule it for you”.
In other words: if you don’t give your body rest, your body will break down and oblige you to rest. Please be aware this goes for mental effort too; your brain is just another organ.
So, plan ahead, schedule breaks, find someone to take over, set up your cared-for-person with the resources to care for themself as well as possible (do this anyway, of course—independence is generally good so far as it’s possible), and make the time/effort to get you what you need for you. Sleep, distraction, a change of scenery, whatever it may be.
Lastly: what if it’s you?
If you’re reading this and you’re the person who has the higher care needs, then firstly:all strength to you. You have the hardest job here; let’s not forget that.
About that independence: well-intentioned people may forget that, so don’t be afraid to remind them when “I would prefer to do that myself”. Maintaining independence is generally good for the health, even if sometimes it is more work for all concerned than someone else doing it for you. The goal, after all, is your wellbeing, so this shouldn’t be cast aside lightly.
On the flipside: you don’t have to be strong all the time; nobody should.
Being disabled can also be quite isolating (this is probably not a revelation to you), so if you can find community with other people with the same or similar condition(s), even if it’s just online, that can go a very, very long way to making things easier. Both practically, in terms of sharing tips, and psychologically, in terms of just not feeling alone.
See also: How To Beat Loneliness & Isolation
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: