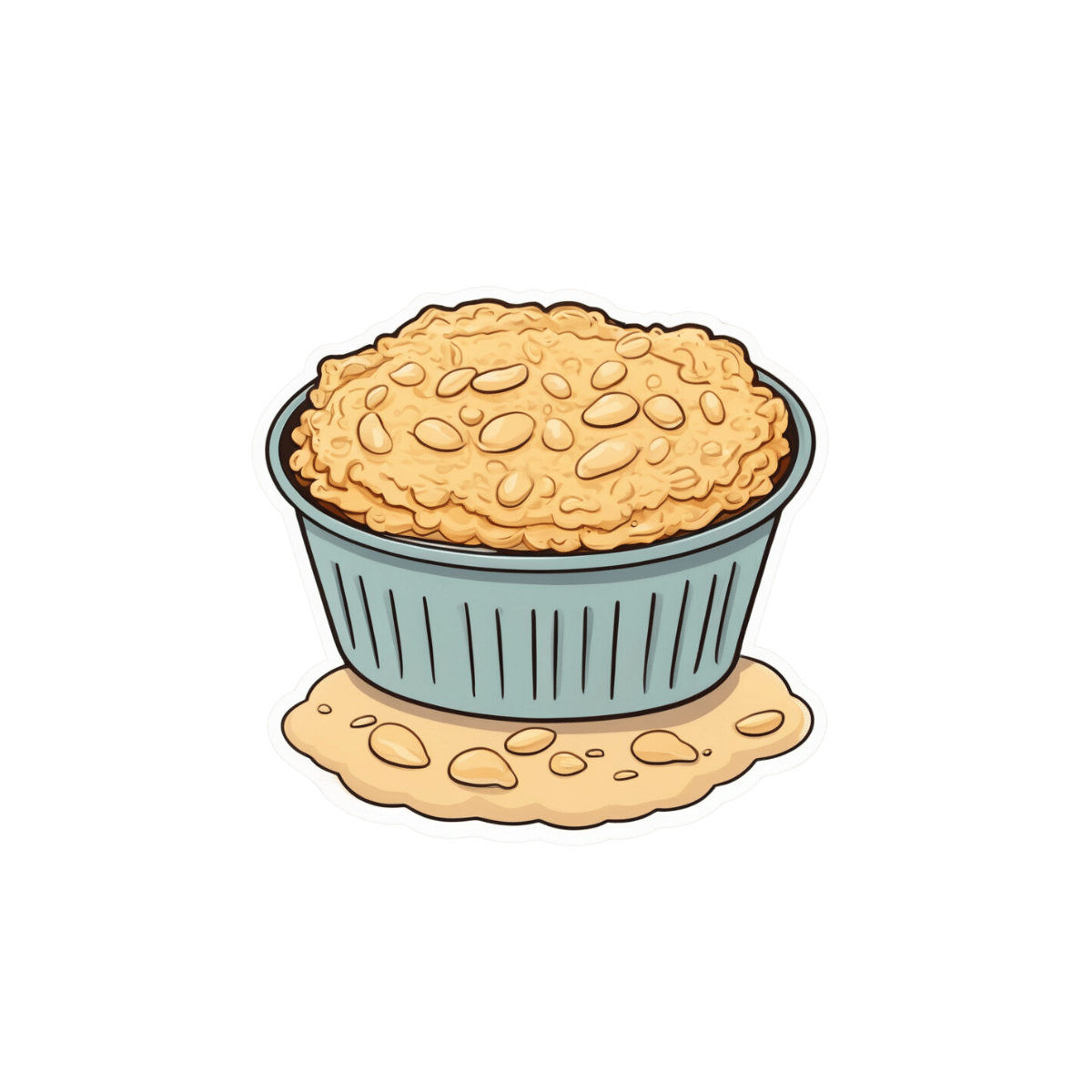
Cannellini Protein Gratin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A healthier twist on a classic, the protein here comes not only from the cannellini beans, but also from (at the risk of alienating French readers) a béchamel sauce that is not made using the traditional method involving flour and butter, but instead, has cashew protein as a major constituent.
You will need
- 3 medium potatoes, chopped (no need to peel them; you can if you want, but many of the nutrients are there and they’re not a problem for the recipe)
- 1 can cannellini beans (also called white kidney beans)
- 1 medium onion, chopped
- 2 stalks celery, sliced
- 1 carrot, chopped
- ½ bulb garlic, minced (or more, if you like)
- 1 jalapeño, chopped
- 2 tbsp tomato paste
- 1 tbsp chia seeds
- 2 tsp black pepper, coarse ground
- Extra virgin olive oil, for frying
For the béchamel sauce:
- ½ cup milk (we recommend a neutral-tasting plant milk, such as unsweetened soy, but go with your preference)
- ⅓ cup cashews, soaked in hot water for at least 5 minutes (longer is fine) and drained
- ¼ cup nutritional yeast
- 1 tsp garlic powder
- 1 tsp dried thyme
Method
(we suggest you read everything at least once before doing anything)
Note: it will be a bonus if you can use a pan that is good both for going on the hob and in the oven, such as a deep cast iron skillet, or a Dutch oven. If you don’t have something like that though, it’s fine, just use a sauté pan or similar, and then transfer to an oven dish for the oven part—we’ll mention this again when we get to it.
1) Preheat the oven to 250℉/175℃.
2) Heat the pan, adding some oil and then the oven; fry it for about 5 minutes, stirring often.
3) Add the potatoes, celery, carrot, garlic, and jalapeño, stirring for another 2 minutes.
4) Add the tomato paste, along with 1 cup water, the chia seeds, and the black pepper, and cook for a further 15 minutes, stirring occasionally as necessary.
5) Add the cannellini beans, and cook for another 15 minutes, stirring occasionally as necessary.
6) Blend all the ingredients for the béchamel sauce, processing it until it is smooth.
7) If you are using an oven-safe pan, pour the béchamel sauce over the bean mixture (don’t stir it; the sauce should remain on top) and transfer it to the oven. Don’t use a lid.
If you’re not using an oven safe pan, first transfer the bean mixture to an oven dish, then pour the béchamel sauce over the bean mixture (don’t stir it; the sauce should remain on top) and put it in the oven. Don’t use a lid.
8) Bake for about 15 minutes, or until turning golden-brown on top.
9) Serve! It can be enjoyed on its own, or with salad and/or rice. See also, our Tasty Versatile Rice Recipe.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- What Matters Most For Your Heart?
- The Many Health Benefits Of Garlic
- Easily Digestible Vegetarian Protein Sources
- Is Dairy Scary?
- Cashew Nuts vs Coconut – Which is Healthier?
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Are GMOs Good Or Bad For Us?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unzipping Our Food’s Genes
In yesterday’s newsletter, we asked you for your (health-related) views on GMOs.
But what does the science say?
First, a note on terms
Technically, we (humans) have been (g)enetically (m)odifying (o)rganisms for thousands of years.
If you eat a banana, you are enjoying the product of many generations of artificial selection, to change its genes to produce a fruit that is soft, sweet, high in nutrients, and digestible without cooking. The original banana plant would be barely recognizable to many people now (and also, barely edible). We’ve done similarly with countless other food products.
So in this article, we’re going to be talking exclusively about modern genetic modification of organisms, using exciting new (ish, new as in “in the last century”) techniques to modify the genes directly, in a copy-paste fashion.
For more details on the different kinds of genetic modification of organisms, and how they’re each done (including the modern kinds), check out this great article from Sciencing, who explain it in more words than we have room for here:
Sciencing | How Are GMOs Made?
(the above also offers tl;dr section summaries, which are great too)
GMOS are outright dangerous (cancer risks, unknown risks, etc): True or False?
False, so far as we know, in any direct* fashion. Obviously “unknown risks” is quite a factor, since those are, well, unknown. But GMOs on the market undergo a lot of safety testing, and have invariably passed happily.
*However! Glyphosate (the herbicide), on the other hand, has a terrible safety profile and is internationally banned in very many countries for this reason.
Why is this important? Because…
- in the US (and two out of ten Canadian provinces), glyphosate is not banned
- In the US (and we may hypothesize, those two Canadian provinces) one of the major uses of genetic modification of foodstuffs is to make it resistant to glyphosate
- Consequently, GMO foodstuffs grown in those places have generally been liberally doused in glyphosate
So… It’s not that the genetic modification itself makes the food dangerous and potentially carcinogenic (it doesn’t), but it is that the genetic modification makes it possible to use a lot more glyphosate without losing crops to glyphosate’s highly destructive properties.
Which results in the end-consumer eating glyphosate. Which is not good. For example:
❝Following the landmark case against Monsanto, which saw them being found liable for a former groundskeeper, 46 year old Dewayne Johnson’s cancer, 32 countries have to date banned the use of Glyphosate, the key ingredient in Monsanto’s Roundup weed killer. The court awarded Johnson R4.2 billion in damages finding Monsanto “acted with malice or oppression”.❞
Source: see below!
You can read more about where glyphosate is and isn’t banned, here:
33 countries ban the use of Glyphosate—the key ingredient in Roundup
For the science of this (and especially the GMO → glyphosate use → cancer pipeline), see:
Use of Genetically Modified Organism (GMO)-Containing Food Products in Children
GMOs are extra healthy because of the modifications (they were designed for that, right?): True or False?
True or False depending on who made them and why! As we’ve seen above, not all companies seem to have the best interests of consumer health in mind.
However, they can be! Here are a couple of great examples:
❝Recently, two genome-edited crops targeted for nutritional improvement, high GABA tomatoes and high oleic acid soybeans, have been released to the market.
Nutritional improvement in cultivated crops has been a major target of conventional genetic modification technologies as well as classical breeding methods❞
Source: Drs. Nagamine & Ezura
Read in full: Genome Editing for Improving Crop Nutrition
(note, they draw a distinction of meaning between genome editing and genetic modification, according to which of two techniques is used, but for the purposes of our article today, this is under the same umbrella)
Want to know more?
If you’d like to read more about this than we have room for here, here’s a great review in the Journal of Food Science & Nutrition:
Should we still worry about the safety of GMO foods? Why and why not? A review
Take care!
Share This Post
-
Switchcraft – by Dr. Elaine Fox
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How do we successfully balance “a mind is like a parachute: it only works if it’s open”, with the importance of also actually having some kind of personal integrity and consistency?
Dr. Fox recommends that we focus on four key attributes:
- Mental agility
- Self-awareness
- Emotional awareness
- Situational awareness
If this sounds a little wishy-washy, it isn’t—she delineates and explains each in detail. And most importantly: how we can build and train each one.
Mental agility, for example, is not about being able to rapidly solve chess problems or “answer these riddles three”. It’s more about:
- Adaptability
- Balancing our life
- Challenging (and if appropriate, changing) our perspective
- Developing our mental competence
This sort of thing is the “meat” of the book. Meanwhile, self-awareness is more a foundational conscious knowledge of one’s own “pole star” values, while emotional awareness is a matter of identifying and understanding and accepting what we feel—anything less is self-sabotage! And situational awareness is perhaps most interesting:
Dr. Fox advocates for “trusting one’s gut feelings”. With a big caveat, though!
If we trust our gut feelings without developing their accuracy, we’re just going to go about being blindly prejudiced and often wrong. So, a whole section of the book is devoted to honing this and improving our ability to judge things as they really are—rather than as we expect.
Bottom line: this book is a great tool for not only challenging our preconceptions about how we think, but giving us the resources to be adaptable and resilient without sacrificing integrity.
Click here to check out Switchcraft on Amazon and level up your thinking!
Share This Post
-
Mythbusting The Big O
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Early To Bed…”
In yesterday’s newsletter, we asked you for your (health-related) views on orgasms.
But what does the science say?
Orgasms are essential to good health: True or False?
False, in the most literal sense. One certainly won’t die without them. Anorgasmia (the inability to orgasm) is a condition that affects many postmenopausal women, some younger women, and some men. And importantly, it isn’t fatal—just generally considered unfortunate:
Anorgasmia Might Explain Why You’re Not Orgasming When You Want To
That article focuses on women; here’s a paper focusing on men:
Orgasms are good for the health, but marginally: True or False?
True! They have a wide array of benefits, depending on various factors (including, of course, one’s own sex). That said, the benefits are so marginal that we don’t have a flock of studies to cite, and are reduced to pop-science sources that verbally cite studies that are, alas, nowhere to be found, for example:
- For women: 9 Orgasm Benefits That Might Surprise You
- For men: 9 Ways Orgasms May Benefit Your Health
Doubtlessly the studies do exist, but are sparse enough that finding them is a nightmare as the keywords for them will bring up a lot of studies about orgasms and health that aren’t answering the above question (usually: health’s affect on orgasms, rather than the other way around).
There is some good science for post-menopausal women, though! Here it is:
Misconceptions About Sexual Health in Older Women
(if you have the time to read this, this also covers many very avoidable things that can disrupt sexual function, in ways that people will errantly chalk up to old age, not knowing that they are missing out needlessly)
Orgasms are good or bad, depending on being male or female: True or False
False, broadly. The health benefits are extant and marginal for almost everyone, as indicated above.
What’s that “almost” about, then?
There are a very few* people (usually men) for whom it doesn’t go well. In such cases, they have a chronic and lifelong problem whereby orgasm is followed by 2–7 days of flu-like and allergic symptoms. Little is known about it, but it appears to be some sort of autoimmune disorder.
Read more: Post-orgasmic illness syndrome: history and current perspectives
*It’s hard to say for sure how few though, as it is surely under-reported and thus under-diagnosed; likely even misdiagnosed if the patient doesn’t realize that orgasms are the trigger for such episodes, and the doctor doesn’t think to ask. Instead, they will be busy trying to eliminate foods from the diet, things like that, while missing this cause.
Orgasms are better avoided for optimal health: True or False?
Aside from the above, False. There is a common myth for men of health benefits of “semen retention”, but it is not based in science, just tradition. You can read a little about it here:
The short version is: do it if you want; don’t if you don’t; the body will compensate either way so it won’t make a meaningful difference to anything for most people, healthwise.
Small counterpoint: while withholding orgasm (and ejaculation) is not harmful to health, what does physiologically need draining sometimes is prostate fluid. But that can also be achieved mechanically through prostate milking, or left to fend for itself (as it will in nocturnal emissions, popularly called wet dreams). However, if you have problems with an enlarged prostate, it may not be a bad idea to take matters into your own hands, so to speak. As ever, do check with your doctor if you have (or think you may have) a condition that might affect this.
One final word…
We’re done with mythbusting for today, but we wanted to share this study that we came across (so to speak) while researching, as it’s very interesting:
On which note: if you haven’t already, consider getting a “magic wand” style vibe; you can thank us later (this writer’s opinion: everyone should have one!).
Top tip: do get the kind that plugs into the wall, not rechargeable. The plug-into-the-wall kind are more powerful, and last much longer (both “in the moment”, and in terms of how long the device itself lasts).
Enjoy!
Share This Post
Related Posts
-
Oral retinoids can harm unborn babies. But many women taking them for acne may not be using contraception
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Oral retinoids are a type of medicine used to treat severe acne. They’re sold under the brand name Roaccutane, among others.
While oral retinoids are very effective, they can have harmful effects if taken during pregnancy. These medicines can cause miscarriages and major congenital abnormalities (harm to unborn babies) including in the brain, heart and face. At least 30% of children exposed to oral retinoids in pregnancy have severe congenital abnormalities.
Neurodevelopmental problems (in learning, reading, social skills, memory and attention) are also common.
Because of these risks, the Australasian College of Dermatologists advises oral retinoids should not be prescribed a month before or during pregnancy under any circumstances. Dermatologists are instructed to make sure a woman isn’t pregnant before starting this treatment, and discuss the risks with women of childbearing age.
But despite this, and warnings on the medicines’ packaging, pregnancies exposed to oral retinoids continue to be reported in Australia and around the world.
In a study published this month, we wanted to find out what proportion of Australian women of reproductive age were taking oral retinoids, and how many of these women were using contraception.
Our results suggest a high proportion of women are not using effective contraception while on these drugs, indicating Australia needs a strategy to reduce the risk oral retinoids pose to unborn babies.
Contraception options
Using birth control to avoid pregnancy during oral retinoid treatment is essential for women who are sexually active. Some contraception methods, however, are more reliable than others.
Long-acting-reversible contraceptives include intrauterine devices (IUDs) inserted into the womb (such as Mirena, Kyleena, or copper devices) and implants under the skin (such as Implanon). These “set and forget” methods are more than 99% effective.
Oral retinoids taken during pregnancy can cause complications in babies. Gorodenkoff/Shutterstock The effectiveness of oral contraceptive pills among “perfect” users (following the directions, with no missed or late pills) is similarly more than 99%. But in typical users, this can fall as low as 91%.
Condoms, when used as the sole method of contraception, have higher failure rates. Their effectiveness can be as low as 82% in typical users.
Oral retinoid use over time
For our study, we analysed medicine dispensing data among women aged 15–44 from Australia’s Pharmaceutical Benefit Scheme (PBS) between 2013 and 2021.
We found the dispensing rate for oral retinoids doubled from one in every 71 women in 2013, to one in every 36 in 2021. The increase occurred across all ages but was most notable in young women.
Most women were not dispensed contraception at the same time they were using the oral retinoids. To be sure we weren’t missing any contraception that was supplied before the oral retinoids, we looked back in the data. For example, for an IUD that lasts five years, we looked back five years before the oral retinoid prescription.
Our analysis showed only one in four women provided oral retinoids were dispensed contraception simultaneously. This was even lower for 15- to 19-year-olds, where only about one in eight women who filled a prescription for oral retinoids were dispensed contraception.
A recent study found 43% of Australian year 10 and 69% of year 12 students are sexually active, so we can’t assume this younger age group largely had no need for contraception.
One limitation of our study is that it may underestimate contraception coverage, because not all contraceptive options are listed on the PBS. Those options not listed include male and female sterilisation, contraceptive rings, condoms, copper IUDs, and certain oral contraceptive pills.
But even if we presume some of the women in our study were using forms of contraception not listed on the PBS, we’re still left with a significant portion without evidence of contraception.
What are the solutions?
Other countries such as the United States and countries in Europe have pregnancy prevention programs for women taking oral retinoids. These programs include contraception requirements, risk acknowledgement forms and regular pregnancy tests. Despite these programs, unintended pregnancies among women using oral retinoids still occur in these countries.
But Australia has no official strategy for preventing pregnancies exposed to oral retinoids. Currently oral retinoids are prescribed by dermatologists, and most contraception is prescribed by GPs. Women therefore need to see two different doctors, which adds costs and burden.
Preventing pregnancy during oral retinoid treatment is essential. Krakenimages.com/Shutterstock Rather than a single fix, there are likely to be multiple solutions to this problem. Some dermatologists may not feel confident discussing sex or contraception with patients, so educating dermatologists about contraception is important. Education for women is equally important.
A clinical pathway is needed for reproductive-aged women to obtain both oral retinoids and effective contraception. Options may include GPs prescribing both medications, or dermatologists only prescribing oral retinoids when there’s a contraception plan already in place.
Some women may initially not be sexually active, but change their sexual behaviour while taking oral retinoids, so constant reminders and education are likely to be required.
Further, contraception access needs to be improved in Australia. Teenagers and young women in particular face barriers to accessing contraception, including costs, stigma and lack of knowledge.
Many doctors and women are doing the right thing. But every woman should have an effective contraception plan in place well before starting oral retinoids. Only if this happens can we reduce unintended pregnancies among women taking these medicines, and thereby reduce the risk of harm to unborn babies.
Dr Laura Gerhardy from NSW Health contributed to this article.
Antonia Shand, Research Fellow, Obstetrician, University of Sydney and Natasha Nassar, Professor of Paediatric and Perinatal Epidemiology and Chair in Translational Childhood Medicine, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Longevity Project – by Dr. Howard Friedman & Dr. Leslie Martin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most books on the topic of longevity focus on such things as diet and exercise, and indeed, those are of course important things. But what of psychological and sociological factors?
Dr. Friedman and Dr. Martin look at a landmark longitudinal study, following a large group of subjects from childhood into old age. Looking at many lifestyle factors and life events, they crunched the numbers to see what things really made the biggest impact on healthy longevity.
A strength of the book is that this study had a huge amount of data—a limitation of the book is that it often avoids giving that concrete data, preferring to say “many”, “a majority”, “a large minority”, “some”, and so forth.
However, the conclusions from the data seem clear, and include many observations such as:
- conscientiousness is a characteristic that not only promotes healthy long life, but also can be acquired as time goes by (some “carefree” children became “conscientious” adults)
- resilience is a characteristic that promotes healthy long life—but tends to only be “unlocked” by adversity
- men tend to live longer if married—women, not so much
- religion and spirituality are not big factors in healthy longevity—but social connections (that may or may not come with such) do make a big difference
Bottom line: if you’d like to know which of your decisions are affecting your healthy longevity (beyond the obvious diet, exercise, etc), this is a great book for collating that information and presenting, in essence, a guideline for a long healthy life.
Click here to check out The Longevity Project and see how it applies to your life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Brain Power – by Michael Gelb & Kelly Howell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s most important when it comes to brain health? Is it the right diet? Supplements? Brain-training? Attitude? Sleep? Physical exercise? Social connections? Something else?
This book covers a lot of bases, including all of the above and more. The authors are not scientists by training and this is not a book of science, so much as a book of aggregated science-based advice from other sources. The authors did consult with many scientists, and their input is shown throughout.
In the category of criticism, nothing here goes very deeply into the science, and there’s also nothing you wouldn’t find we’ve previously written about in a 10almonds article somewhere. But all the same, it’s good to have a wide variety of brain-healthy advices all in one place.
Bottom line: if you’re looking for a one-stop-shop “look after your brain as you age” guide, then this is a good one.
Click here to check out Brain Power, and improve your mind as you age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: