What’s the difference between vegan and vegetarian?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
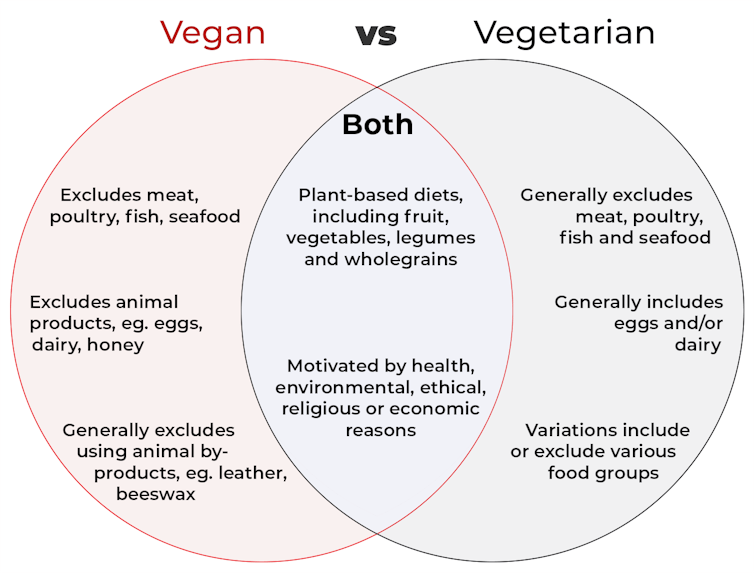
Vegan and vegetarian diets are plant-based diets. Both include plant foods, such as fruits, vegetables, legumes and whole grains.
But there are important differences, and knowing what you can and can’t eat when it comes to a vegan and vegetarian diet can be confusing.
So, what’s the main difference?

What’s a vegan diet?
A vegan diet is an entirely plant-based diet. It doesn’t include any meat and animal products. So, no meat, poultry, fish, seafood, eggs, dairy or honey.
What’s a vegetarian diet?
A vegetarian diet is a plant-based diet that generally excludes meat, poultry, fish and seafood, but can include animal products. So, unlike a vegan diet, a vegetarian diet can include eggs, dairy and honey.
But you may be wondering why you’ve heard of vegetarians who eat fish, vegetarians who don’t eat eggs, vegetarians who don’t eat dairy, and even vegetarians who eat some meat. Well, it’s because there are variations on a vegetarian diet:
- a lacto-ovo vegetarian diet excludes meat, poultry, fish and seafood, but includes eggs, dairy and honey
- an ovo-vegetarian diet excludes meat, poultry, fish, seafood and dairy, but includes eggs and honey
- a lacto-vegetarian diet excludes meat, poultry, fish, seafood and eggs, but includes dairy and honey
- a pescatarian diet excludes meat and poultry, but includes eggs, dairy, honey, fish and seafood
- a flexitarian, or semi-vegetarian diet, includes eggs, dairy and honey and may include small amounts of meat, poultry, fish and seafood.
Are these diets healthy?
A 2023 review looked at the health effects of vegetarian and vegan diets from two types of study.
Observational studies followed people over the years to see how their diets were linked to their health. In these studies, eating a vegetarian diet was associated with a lower risk of developing cardiovascular disease (such as heart disease or a stroke), diabetes, hypertension (high blood pressure), dementia and cancer.
For example, in a study of 44,561 participants, the risk of heart disease was 32% lower in vegetarians than non-vegetarians after an average follow-up of nearly 12 years.
Further evidence came from randomised controlled trials. These instruct study participants to eat a specific diet for a specific period of time and monitor their health throughout. These studies showed eating a vegetarian or vegan diet led to reductions in weight, blood pressure, and levels of unhealthy cholesterol.
For example, one analysis combined data from seven randomised controlled trials. This so-called meta-analysis included data from 311 participants. It showed eating a vegetarian diet was associated with a systolic blood pressure (the first number in your blood pressure reading) an average 5 mmHg lower compared with non-vegetarian diets.
It seems vegetarian diets are more likely to be healthier, across a number of measures.
For example, a 2022 meta-analysis combined the results of several observational studies. It concluded a vegetarian diet, rather than vegan diet, was recommended to prevent heart disease.
There is also evidence vegans are more likely to have bone fractures than vegetarians. This could be partly due to a lower body-mass index and a lower intake of nutrients such as calcium, vitamin D and protein.
But it can be about more than just food
Many vegans, where possible, do not use products that directly or indirectly involve using animals.
So vegans would not wear leather, wool or silk clothing, for example. And they would not use soaps or candles made from beeswax, or use products tested on animals.
The motivation for following a vegan or vegetarian diet can vary from person to person. Common motivations include health, environmental, ethical, religious or economic reasons.
And for many people who follow a vegan or vegetarian diet, this forms a central part of their identity.

So, should I adopt a vegan or vegetarian diet?
If you are thinking about a vegan or vegetarian diet, here are some things to consider:
- eating more plant foods does not automatically mean you are eating a healthier diet. Hot chips, biscuits and soft drinks can all be vegan or vegetarian foods. And many plant-based alternatives, such as plant-based sausages, can be high in added salt
- meeting the nutrient intake targets for vitamin B12, iron, calcium, and iodine requires more careful planning while on a vegan or vegetarian diet. This is because meat, seafood and animal products are good sources of these vitamins and minerals
- eating a plant-based diet doesn’t necessarily mean excluding all meat and animal products. A healthy flexitarian diet prioritises eating more whole plant-foods, such as vegetables and beans, and less processed meat, such as bacon and sausages
- the Australian Dietary Guidelines recommend eating a wide variety of foods from the five food groups (fruit, vegetables, cereals, lean meat and/or their alternatives and reduced-fat dairy products and/or their alternatives). So if you are eating animal products, choose lean, reduced-fat meats and dairy products and limit processed meats.
Katherine Livingstone, NHMRC Emerging Leadership Fellow and Senior Research Fellow at the Institute for Physical Activity and Nutrition, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
HRT: Bioidentical vs Animal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
HRT: A Tale Of Two Approaches
In yesterday’s newsletter, we asked you for your assessment of menopausal hormone replacement therapy (HRT).
- A little over a third said “It can be medically beneficial, but has some minor drawbacks”
- A little under a third said “It helps, but at the cost of increased cancer risk; not worth it”
- Almost as many said “It’s a wondrous cure-all that makes you happier, healthier, and smell nice too”
- Four said “It is a dangerous scam and a sham; “au naturel” is the way to go”
So what does the science say?
Which HRT?
One subscriber who voted for “It’s a wondrous cure-all that makes you healthier, happier, and smell nice too” wrote to add:
❝My answer is based on biodentical hormone replacement therapy. Your survey did not specify.❞
And that’s an important distinction! We did indeed mean bioidentical HRT, because, being completely honest here, this European writer had no idea that Premarin etc were still in such wide circulation in the US.
So to quickly clear up any confusion:
- Bioidentical hormones: these are (as the name suggests) identical on a molecular level to the kind produced by humans.
- Conjugated Equine Estrogens: such as Premarin, come from animals. Indeed, the name “Premarin” comes from “pregnant mare urine”, the substance used to make it.
There are also hormone analogs, such as medroxyprogesterone acetate, which is a progestin and not the same thing as progesterone. Hormone analogs such as the aforementioned MPA are again, a predominantly-American thing—though they did test it first in third-world countries, after testing it on animals and finding it gave them various kinds of cancer (breast, cervical, ovarian, uterine).
A quick jumping-off point if you’re interested in that:
Depot medroxyprogesterone acetate and the risk of breast and gynecologic cancer
this is about its use as a contraceptive (so, much lower doses needed), but it is the same thing sometimes given in the US as part of menopausal HRT. You will note that the date on that research is 1996; DMPA is not exactly cutting-edge and was first widely used in the 1950s.
Similarly, CEEs (like Premarin) have been used since the 1930s, while estradiol (bioidentical estrogen) has been in use since the 1970s.
In short: we recommend being wary of those older kinds and mostly won’t be talking about them here.
Bioidentical hormones are safer: True or False?
True! This is an open-and-shut case:
❝Physiological data and clinical outcomes demonstrate that bioidentical hormones are associated with lower risks, including the risk of breast cancer and cardiovascular disease, and are more efficacious than their synthetic and animal-derived counterparts.
Until evidence is found to the contrary, bioidentical hormones remain the preferred method of HRT. ❞
Further research since that review has further backed up its findings.
Source: Are Bioidentical Hormones Safer or More Efficacious than Other Commonly Used Versions in HRT?
So simply, if you’re going on HRT (estrogen and/or progesterone), you might want to check it’s the bioidentical kind.
HRT can increase the risk of breast cancer: True or False?
Contingently True, but for most people, there is no significant increase in risk.
First: again, we’re talking bioidentical hormones, and in this case, estradiol. Older animal-derived attempts had much higher risks with much lesser efficaciousness.
There have been so many studies on this (alas, none that have been publicised enough to undo the bad PR in the wake of old-fashioned HRT from before the 70s), but here’s a systematic review that highlights some very important things:
❝Estradiol-only therapy carries no risk for breast cancer, while the breast cancer risk varies according to the type of progestogen.
Estradiol therapy combined with medroxyprogesterone, norethisterone and levonorgestrel related to an increased risk of breast cancer, estradiol therapy combined with dydrogesterone and progesterone carries no risk❞
In fewer words:
- Estradiol by itself: no increased risk of breast cancer
- Estradiol with MDPA or other progestogens that aren’t really progesterone: increased risk of breast cancer
- Estradiol with actual progesterone: back to no increased risk of breast cancer
So again, you might want to make sure you are getting actual bioidentical hormones, and not something else!
However! If you are aware that you already have an increased risk of breast cancer (e.g. family history, you’ve had it before, you know you have certain genes for it, etc), then you should certainly discuss that with your doctor, because your personal circumstances may be different:
❝Tailored HRT may be used without strong evidence of a deleterious effect after ovarian cancer, endometrial cancer, most other gynecological cancers, bowel cancer, melanoma, a family history of breast cancer, benign breast disease, in carriers of BRACA mutations, after breast cancer if adjuvant therapy is not being used, past thromboembolism, varicose veins, fibroids and past endometriosis.
Relative contraindications are existing cardiovascular and cerebrovascular disease and breast cancer being treated with adjuvant therapies❞
Source: HRT in difficult circumstances: are there any absolute contraindications?
HRT makes you happier, healthier, and smell nice too: True or False?
Contingently True, assuming you do want its effects, which generally means the restoration of much of the youthful vitality you enjoyed pre-menopause.
The “and smell nice too” was partly rhetorical, but also partly literal: our scent is largely informed by our hormones, and higher estrogen results in a sweeter scent; lower estrogen results in a more bitter scent. Not generally considered an important health matter, but it’s a thing, so hey.
More often, people take menopausal HRT for more energy, stronger bones (reduced osteoporosis risk), healthier heart (reduced CVD risk), improved sexual health, better mood, healthier skin and hair, and general avoidance of menopause symptoms:
Read more: Skin, hair and beyond: the impact of menopause
We’d need another whole main feature to discuss all the benefits properly; today we’re just mythbusting.
HRT does have some drawbacks: True or False?
True, and/but how serious they are (beyond the aforementioned consideration in the case of an already-increased risk of breast cancer) is a matter of opinion.
For example, it is common to get a reprise of monthly cramps and/or mood swings, depending on how one is taking the HRT and other factors (e.g. your own personal physiology and genetic predispositions). For most people, these will even out over time.
It’s also even common to get a reprise of (much slighter than before) monthly bleeding, unless you have for example had a hysterectomy (no uterus = no bleeding). Again, this will usually settle down in a matter of months.
If you experience anything more alarming than that, then indeed check with your doctor.
HRT is a dangerous scam and sham: True or False?
False, simply. As described above, for most people they’re quite safe. Again, talking bioidentical hormones.
The other kind are in the most neutral sense a sham (i.e. they are literally sham hormones), though they’re not without their merits and for many people they may be better than nothing.
As for being a scam, biodentical hormones are widely prescribed in the many countries that have universal healthcare and/or a single-payer healthcare system, where there would be no profit motive (and considerable cost) in doing so.
They’re prescribed because they are effective and thus reduce healthcare spending in other areas (such as treating osteoporosis or CVD after the fact) and improve Health Related Quality of Life, and by extension, health-adjusted life-years, which is one of the top-used metrics for such systems.
See for example:
Our apologies, gentlemen
We wanted to also talk about testosterone therapy for the andropause, but we’ve run out of room today (because of covering the important distinction of bioidentical vs old-fashioned HRT)!
To make it up to you, we’ll do a full main feature on it (it’s an interesting topic) in the near future, so watch this space
Ladies, we’ll also at some point cover the pros and cons of different means of administration, e.g. pills, transdermal gel, injections, patches, pessaries, etc—which often have big differences.
That’ll be in a while though, because we try to vary our topics, so we can’t talk about menopausal HRT all the time, fascinating and important a topic it is.
Meanwhile… take care, all!
Share This Post
-
The Green Roasting Tin – by Rukmini Iyer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be wondering: “do I really need a book to tell me to put some vegetables in a roasting tin and roast them?” and maybe not, but the book offers a lot more than that.
Indeed, the author notes “this book was slightly in danger of becoming the gratin and tart book, because I love both”, but don’t worry, most of the recipes are—as you might expect—very healthy.
As for formatting: the 75 recipes are divided first into vegan or vegetarian, and then into quick/medium/slow, in terms of how long they take.
However, even the “slow” recipes don’t actually take more effort, just, more time in the oven.
One of the greatest strengths of this book is that not only does it offer a wide selection of wholesome mains, but also, if you’re putting on a big spread, these can easily double up as high-class low-effort sides.
Bottom line: if you’d like to eat more vegetables in 2024 but want to make it delicious and with little effort, put this book on your Christmas list!
Click here to check out The Green Roasting Tin, and level-up yours!
Share This Post
-
Fruit & Veg In The Fridge: Pros & Cons
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝What effect does refrigeration have on the nutritional value of fruit and vegetables??❞
It’s difficult to give a single definitive answer, because naturally there are a lot of different fruits and vegetables, and a lot of different climates. The answer may be different for tomatoes in Alaska vs bananas in Arizona!
However, we can still generalize at least somewhat
Refrigeration will generally slow down any degradation process, and in the case of fruit and vegetables, that can mean slowing down their “ripening” too, as applicable.
However…
Refrigeration will also impede helpful bioactivity too, and that includes quite a list of things.
Here’s a good study that’s quite illustrative; we’d summarize the conclusions but the rather long title already does that nicely:
So, this really is a case of “there are pros and cons, but probably more cons on balance”.
In practical terms, a good take-away from this can be twofold:
- don’t keep fruit and veg in the fridge unless the ambient temperature really requires it
- if the ambient temperature does require it, it’s best to get the produce in fresh each day if that’s feasible, to minimize time spent in the fridge
An extra thing not included there: often when it comes to the spoilage of fruit and veg, the problem is that it respires and oxidizes; reducing the temperature does lower the rate of those, but often a far better way is to remove the oxygen. So for example, if you get carried away and chop too many carrot batons for your hummus night, then putting them in a sealed container can go a long way to keeping them fresh.
See also: How Does the Nutritional Value of Fruits and Vegetables Change Over Time?
Enjoy!
Share This Post
Related Posts
-
Sometimes, Perfect Isn’t Practical!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝10 AM breakfast is not realistic for most. What’s wrong with 8 AM and Evening me at 6. Don’t quite understand the differentiation.❞
(for reference, this is about our “Breakfasting For Health?” main feature)
It’s not terrible to do it the way you suggest It’s just not optimal, either, that’s all!
Breakfasting at 08:00 and then dining at 18:00 is ten hours apart, so no fasting benefits between those. Let’s say you take half an hour to eat dinner, then eat nothing again until breakfast, that’s 18:30 to 08:00, so that’s 13½ hours fasting. You’ll recall that fasting benefits start at 12 hours into the fast, so that means you’d only get 1½ hours of fasting benefits.
As for breakfasting at 08:00 regardless of intermittent fasting considerations, the reason for the conclusion of around 10:00 being optimal, is based on when our body is geared up to eat breakfast and get the most out of that, which the body can’t do immediately upon waking. So if you wake and get sunlight at 08:30, get a little moderate exercise, then by 10:00 your digestive system will be perfectly primed to get the most out of breakfast.
However! This is entirely based on you waking and getting sunlight at 08:30.
So, iff you wake and get sunlight at 06:30, then in that case, breakfasting at 08:00 would give the same benefits as described above. What’s important is the 1½ hour priming-time.
Writer’s note: our hope here is always to be informational, not prescriptive. Take what works for you; ignore what doesn’t fit your lifestyle.
I personally practice intermittent fasting for about 21hrs/day. I breakfast (often on nuts and perhaps a little salad) around 16:00, and dine at around 18:00ish, giving myself a little wiggleroom. I’m not religious about it and will slide it if necessary.
As you can see: that makes what is nominally my breakfast practically a pre-dinner snack, and I clearly ignore the “best to eat in the morning” rule because that’s not consistent with my desire to have a family dinner together in the evening while still practicing the level of fasting that I prefer.
Science is science, and that’s what we report here. How we apply it, however, is up to us all as individuals!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Strong Curves – by Bret Contreras & Kellie Davis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The title (and subtitle) is, of course, an appeal to vanity. However, the first-listed author is well-known as “The Glute Guy”, and he takes this very seriously, not just for aesthetic reasons but also for practical reasons.
After all, when it comes to posture and stability, a lot rests on our hips, and hips, well, they rest on our butt and thighs. What’s more, the gluteus maximus is the largest muscle in the human body, so really, is it a good one to neglect? Probably not, and your lower back will definitely thank you for keeping your glutes in good order, too.
That said, while it’s a focal point, it’s not the be-all-and-end-all, and this book does cover the whole body.
The book takes the reader from “absolute beginner” to “could compete professionally”, with clearly-illustrated and well-described exercises. We also get a strong “crash course” in the relevant anatomy and physiology, and even a chapter on nutrition, which is a lot better than a lot of exercise books’ efforts in that regard.
For those who like short courses, this book has several progressive 12-week workout plans that take the reader from a very clear starting point to a very clear goal point.
Another strength of the book is that while a lot of exercises expect (and require) access to a gym, there are also whole sections of “at home / bodyweight” exercises, including 12-week workout plans for such, as described above.
Bottom line: there’s really nothing bad that this reviewer can find to say about this one—highly recommendable to any woman who wants to get strong while keeping a feminine look.
Click here to check out Strong Curves, and rebuild your body, your way!
PS: at first glance, the cover art looks like an AI model; it’s not; that’s the co-author Kellie Davis, who also serves as the model through the book’s many photographic illustrations.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I’ve been given opioids after surgery to take at home. What do I need to know?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Opioids are commonly prescribed when you’re discharged from hospital after surgery to help manage pain at home.
These strong painkillers may have unwanted side effects or harms, such as constipation, drowsiness or the risk of dependence.
However, there are steps you can take to minimise those harms and use opioids more safely as you recover from surgery.
Flystock/Shutterstock Which types of opioids are most common?
The most commonly prescribed opioids after surgery in Australia are oxycodone (brand names include Endone, OxyNorm) and tapentadol (Palexia).
In fact, about half of new oxycodone prescriptions in Australia occur after a recent hospital visit.
Most commonly, people will be given immediate-release opioids for their pain. These are quick-acting and are used to manage short-term pain.
Because they work quickly, their dose can be easily adjusted to manage current pain levels. Your doctor will provide instructions on how to adjust the dosage based on your pain levels.
Then there are slow-release opioids, which are specially formulated to slowly release the dose over about half to a full day. These may have “sustained-release”, “controlled-release” or “extended-release” on the box.
Slow-release formulations are primarily used for chronic or long-term pain. The slow-release form means the medicine does not have to be taken as often. However, it takes longer to have an effect compared with immediate-release, so it is not commonly used after surgery.
Controlling your pain after surgery is important. This allows you get up and start moving sooner, and recover faster. Moving around sooner after surgery prevents muscle wasting and harms associated with immobility, such as bed sores and blood clots.
Everyone’s pain levels and needs for pain medicines are different. Pain levels also decrease as your surgical wound heals, so you may need to take less of your medicine as you recover.
But there are also risks
As mentioned above, side effects of opioids include constipation and feeling drowsy or nauseous. The drowsiness can also make you more likely to fall over.
Opioids prescribed to manage pain at home after surgery are usually prescribed for short-term use.
But up to one in ten Australians still take them up to four months after surgery. One study found people didn’t know how to safely stop taking opioids.
Such long-term opioid use may lead to dependence and overdose. It can also reduce the medicine’s effectiveness. That’s because your body becomes used to the opioid and needs more of it to have the same effect.
Dependency and side effects are also more common with slow-release opioids than immediate-release opioids. This is because people are usually on slow-release opioids for longer.
Then there are concerns about “leftover” opioids. One study found 40% of participants were prescribed more than twice the amount they needed.
This results in unused opioids at home, which can be dangerous to the person and their family. Storing leftover opioids at home increases the risk of taking too much, sharing with others inappropriately, and using without doctor supervision.
Don’t stockpile your leftover opioids in your medicine cupboard. Take them to your pharmacy for safe disposal. Archer Photo/Shutterstock How to mimimise the risks
Before using opioids, speak to your doctor or pharmacist about using over-the-counter pain medicines such as paracetamol or anti-inflammatories such as ibuprofen (for example, Nurofen, Brufen) or diclofenac (for example, Voltaren, Fenac).
These can be quite effective at controlling pain and will lessen your need for opioids. They can often be used instead of opioids, but in some cases a combination of both is needed.
Other techniques to manage pain include physiotherapy, exercise, heat packs or ice packs. Speak to your doctor or pharmacist to discuss which techniques would benefit you the most.
However, if you do need opioids, there are some ways to make sure you use them safely and effectively:
- ask for immediate-release rather than slow-release opioids to lower your risk of side effects
- do not drink alcohol or take sleeping tablets while on opioids. This can increase any drowsiness, and lead to reduced alertness and slower breathing
- as you may be at higher risk of falls, remove trip hazards from your home and make sure you can safely get up off the sofa or bed and to the bathroom or kitchen
- before starting opioids, have a plan in place with your doctor or pharmacist about how and when to stop taking them. Opioids after surgery are ideally taken at the lowest possible dose for the shortest length of time.
A heat pack may help with pain relief, so you end up using fewer painkillers. New Africa/Shutterstock If you’re concerned about side effects
If you are concerned about side effects while taking opioids, speak to your pharmacist or doctor. Side effects include:
- constipation – your pharmacist will be able to give you lifestyle advice and recommend laxatives
- drowsiness – do not drive or operate heavy machinery. If you’re trying to stay awake during the day, but keep falling asleep, your dose may be too high and you should contact your doctor
- weakness and slowed breathing – this may be a sign of a more serious side effect such as respiratory depression which requires medical attention. Contact your doctor immediately.
If you’re having trouble stopping opioids
Talk to your doctor or pharmacist if you’re having trouble stopping opioids. They can give you alternatives to manage the pain and provide advice on gradually lowering your dose.
You may experience withdrawal effects, such as agitation, anxiety and insomnia, but your doctor and pharmacist can help you manage these.
How about leftover opioids?
After you have finished using opioids, take any leftovers to your local pharmacy to dispose of them safely, free of charge.
Do not share opioids with others and keep them away from others in the house who do not need them, as opioids can cause unintended harms if not used under the supervision of a medical professional. This could include accidental ingestion by children.
For more information, speak to your pharmacist or doctor. Choosing Wisely Australia also has free online information about managing pain and opioid medicines.
Katelyn Jauregui, PhD Candidate and Clinical Pharmacist, School of Pharmacy, Faculty of Medicine and Health, University of Sydney; Asad Patanwala, Professor, Sydney School of Pharmacy, University of Sydney; Jonathan Penm, Senior lecturer, School of Pharmacy, University of Sydney, and Shania Liu, Postdoctoral Research Fellow, Faculty of Medicine and Dentistry, University of Alberta
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: