What’s the difference between ‘strep throat’ and a sore throat? We’re developing a vaccine for one of them
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
It’s the time of the year for coughs, colds and sore throats. So you might have heard people talk about having a “strep throat”.
But what is that? Is it just a bad sore throat that goes away by itself in a day or two? Should you be worried?
Here’s what we know about the similarities and differences between strep throat and a sore throat, and why they matter.

How are they similar?
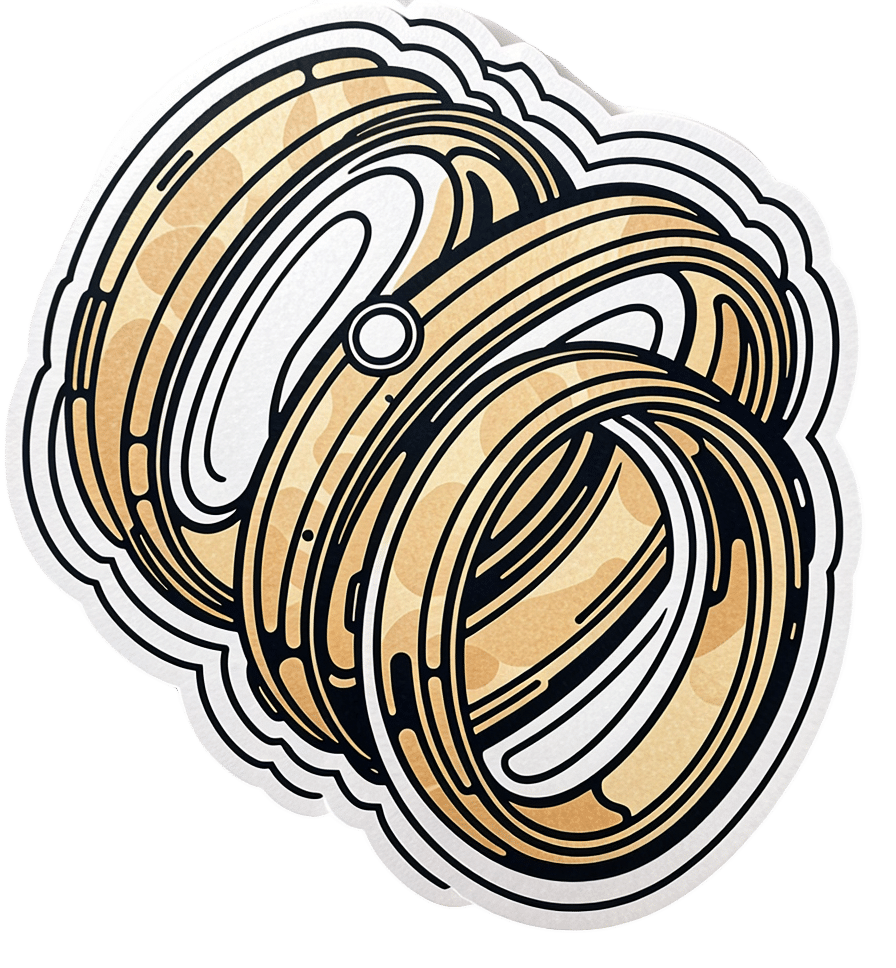
It’s difficult to tell the difference between a sore throat and strep throat as they look and feel similar.
People usually have a fever, a bright red throat and sometimes painful lumps in the neck (swollen lymph nodes). A throat swab can help diagnose strep throat, but the results can take a few days.
Thankfully, both types of sore throat usually get better by themselves.
How are they different?
Most sore throats are caused by viruses such as common cold viruses, the flu (influenza virus), or the virus that causes glandular fever (Epstein-Barr virus).
These viral sore throats can occur at any age. Antibiotics don’t work against viruses so if you have a viral sore throat, you won’t get better faster if you take antibiotics. You might even have some unwanted antibiotic side-effects.
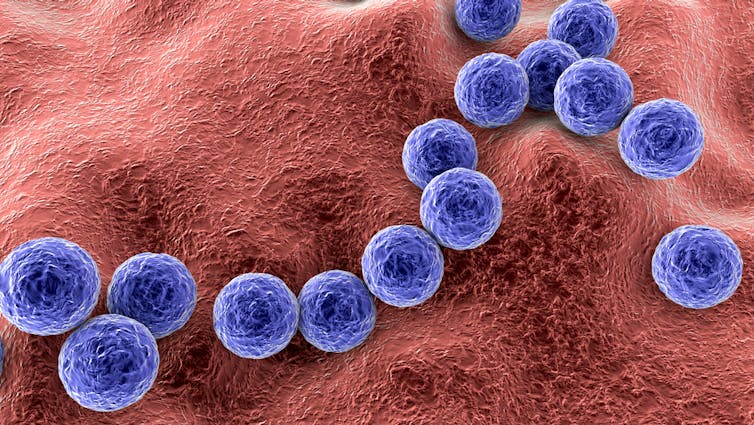
But strep throat is caused by Streptococcus pyogenes bacteria, also known as strep A. Strep throat is most common in school-aged children, but can affect other age groups. In some cases, you may need antibiotics to avoid some rare but serious complications.
In fact, the potential for complications is one key difference between a viral sore throat and strep throat.
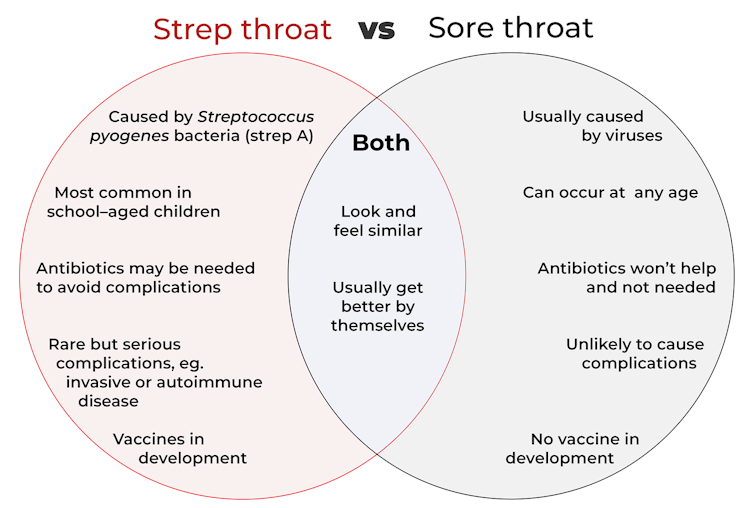
Generally, a viral sore throat is very unlikely to cause complications (one exception is those caused by Epstein-Barr virus which has been associated with illnesses such as chronic fatigue syndrome, multiple sclerosis and certain cancers).
But strep A can cause invasive disease, a rare but serious complication. This is when bacteria living somewhere on the body (usually the skin or throat) get into another part of the body where there shouldn’t be bacteria, such as the bloodstream. This can make people extremely sick.
Invasive strep A infections and deaths have been rising in recent years around the world, especially in young children and older adults. This may be due to a number of factors such as increased social mixing at this stage of the COVID pandemic and an increase in circulating common cold viruses. But overall the reasons behind the increase in invasive strep A infections are not clear.
Another rare but serious side effect of strep A is autoimmune disease. This is when the body’s immune system makes antibodies that react against its own cells.
The most common example is rheumatic heart disease. This is when the body’s immune system damages the heart valves a few weeks or months after a strep throat or skin infection.
Around the world more than 40 million people live with rheumatic heart disease and more than 300,000 die from its complications every year, mostly in developing countries.
However, parts of Australia have some of the highest rates of rheumatic heart disease in the world. More than 5,300 Indigenous Australians live with it.
Why do some people get sicker than others?
We know strep A infections and rheumatic heart disease are more common in low socioeconomic communities where poverty and overcrowding lead to increased strep A transmission and disease.
However, we don’t fully understand why some people only get a mild infection with strep throat while others get very sick with invasive disease.
We also don’t understand why some people get rheumatic heart disease after strep A infections when most others don’t. Our research team is trying to find out.
How about a vaccine for strep A?
There is no strep A vaccine but many groups in Australia, New Zealand and worldwide are working towards one.
For instance, Murdoch Children’s Research Institute and Telethon Kids Institute have formed the Australian Strep A Vaccine Initiative to develop strep A vaccines. There’s also a global consortium working towards the same goal.
Companies such as Vaxcyte and GlaxoSmithKline have also been developing strep A vaccines.
What if I have a sore throat?
Most sore throats will get better by themselves. But if yours doesn’t get better in a few days or you have ongoing fever, see your GP.
Your GP can examine you, consider running some tests and help you decide if you need antibiotics.
Kim Davis, General paediatrician and paediatric infectious diseases specialist, Murdoch Children’s Research Institute; Alma Fulurija, Immunologist and the Australian Strep A Vaccine Initiative project lead, Telethon Kids Institute, and Myra Hardy, Postdoctoral Researcher, Infection, Immunity and Global Health, Murdoch Children’s Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Beating Sleep Apnea
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Healthier, Natural Sleep Without Obstruction!
Obstructive Sleep Apnea, the sleep disorder in which one periodically stops breathing (and thus wakes up) repeatedly through the night, affects about 25% of men and 10% of women:
Prevalence of Obstructive Sleep Apnea Syndrome: A Single-Center Retrospective Study
Why the gender split?
There are clues that suggest it is at least partially hormonal: once women have passed menopause, the gender split becomes equal.
Are there other risk factors?
There are few risk other factors; some we can’t control, and some we can:
- Being older is riskier than being younger
- Being overweight is riskier than not being overweight
- Smoking is (what a shock) riskier than not smoking
- Chronic respiratory diseases increase risk, for example:
- Asthma
- COPD
- Long COVID*—probably. The science is young for this one so far, so we can’t say for sure until more research has been done.
- Some hormonal conditions increase risk, for example:
- Hypothyroidism
- PCOS
*However, patients already undergoing Continuous Positive Airway Pressure (CPAP) treatment for obstructive sleep apnea may have an advantage when fighting a COVID infection:
What can we do about it?
Avoiding the above risk factors, where possible, is great!
If you are already suffering from obstructive sleep apnea, then you probably already know about the possibility of a CPAP device; it’s a mask that one wears to sleep, and it does what its name says (i.e. it applies continuous positive airway pressure), which keeps the airway open.
We haven’t tested these, but other people have, so here are some that the Sleep Foundation found to be worthy of note:
Sleep Foundation | Best CPAP Machines of 2024
What can we do about it that’s not CPAP?
Wearing a mask to sleep is not everyone’s preferred way to do things. There are also a plethora of surgeries available, but we’ll not review those, as those are best discussed with your doctor if necessary.
However, some lifestyle changes can help, including:
- Lose weight, if overweight. In particular, having a collar size under 16” for women or under 17” for men, is sufficient to significantly reduce the risk of obstructive sleep apnea.
- Stop smoking, if you smoke. This one, we hope, is self-explanatory.
- Stop drinking alcohol, or at least reduce intake, if you drink. People who consume alcohol tend to have more frequent, and longer, incidents of obstructive sleep apnea. See also: How To Reduce Or Quit Drinking
- Avoid sedatives and muscle relaxants, if it is safe for you to do so. Obviously, if you need them to treat some other condition you have, talk this through with your doctor. But basically, they can contribute to the “airway collapses on itself” by reducing the muscular tension that keeps your airway the shape it’s supposed to be.
- Sleep on your side, not your back. This is just plain physics, and a matter of wear the obstruction falls.
- Breathe through your nose, not through your mouth. Initially tricky to do while sleeping, but the more you practice it while awake, the more it becomes possible while asleep.
- Consider a nasal decongestant before sleep, if congestion is a problem for you, as that can help too.
For more of the science of these, see:
Cultivating Lifestyle Transformations in Obstructive Sleep Apnea
There are more medical options available not discussed here, too:
American Sleep Apnea Association | Sleep Apnea Treatment Options
Take care!
Share This Post
-
What should I do if I can’t see a psychiatrist?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People presenting at emergency with mental health concerns are experiencing the longest wait times in Australia for admission to a ward, according to a new report from the Australasian College of Emergency Medicine.
But with half of New South Wales’ public psychiatrists set to resign next week after ongoing pay disputes – and amid national shortages in the mental health workforce – Australians who rely on psychiatry support may be wondering where else to go.
If you can’t get in to see a psychiatrist and you need help, there are some other options. However in an emergency, you should call 000.
Why do people see a psychiatrist?
Psychiatrists are doctors who specialise in mental health and can prescribe medication.
People seek or require psychiatry support for many reasons. These may include:
- severe depression, including suicidal thoughts or behaviours
- severe anxiety, panic attacks or phobias
- post-traumatic stress disorder (PTSD)
- eating disorders, such as anorexia or bulimia
- attention deficit hyperactivity disorder (ADHD).
Psychiatrists complement other mental health clinicians by prescribing certain medications and making decisions about hospital admission. But when psychiatry support is not available a range of team members can contribute to a person’s mental health care.
Can my GP help?
Depending on your mental health concerns, your GP may be able to offer alternatives while you await formal psychiatry care.
GPs provide support for a range of mental health concerns, regardless of formal diagnosis. They can help address the causes and impact of issues including mental distress, changes in sleep, thinking, mood or behaviour.
The GP Psychiatry Support Line also provides doctors advice on care, prescription medication and how support can work.
It’s a good idea to book a long consult and consider taking a trusted person. Be explicit about how you’ve been feeling and what previous supports or medication you’ve accessed.
What about psychologists, counsellors or community services?
Your GP should also be aware of supports available locally and online.
For example, Head to Health is a government initiative, including information, a nationwide phone line, and in-person clinics in Victoria. It aims to improve mental health advice, assessment and access to treatment.
Medicare Mental Health Centres provide in-person care and are expanding across Australia.
There are also virtual care services in some areas. This includes advice on individualised assessment including whether to go to hospital.
Some community groups are led by peers rather than clinicians, such as Alternatives to Suicide.
How about if I’m rural or regional?
Accessing support in rural or regional areas is particularly tough.
Beyond helplines and formal supports, other options include local Suicide Prevention Networks and community initiatives such as ifarmwell and Men’s sheds.
Should I go to emergency?
As the new report shows, people who present at hospital emergency departments for mental health should expect long wait times before being admitted to a ward.
But going to a hospital emergency department will be essential for some who are experiencing a physical or mental health crisis.
Managing suicide-related distress
With the mass resignation of NSW psychiatrists looming, and amid shortages and blown-out emergency waiting times, people in suicide-related distress must receive the best available care and support.
Roughly nine Australians die by suicide each day. One in six have had thoughts of suicide at some point in their lives.
Suicidal thoughts can pass. There are evidence-based strategies people can immediately turn to when distressed and in need of ongoing care.
Safety planning is a popular suicide prevention strategy to help you stay safe.
What is a safety plan?
This is a personalised, step-by-step plan to remain safe during the onset or worsening of suicidal urges.
You can develop a safety plan collaboratively with a clinician and/or peer worker, or with loved ones. You can also make one on your own – many people like to use the Beyond Now app.
Safety plans usually include:
- recognising personal warning signs of a crisis (for example, feeling like a burden)
- identifying and using internal coping strategies (such as distracting yourself by listening to favourite music)
- seeking social supports for distraction (for example, visiting your local library)
- letting trusted family or friends know how you’re feeling – ideally, they should know they’re in your safety plan
- knowing contact details of specific mental health services (your GP, mental health supports, local hospital)
- making the environment safer by removing or limiting access to lethal means
- identifying specific and personalised reasons for living.
Our research shows safety planning is linked to reduced suicidal thoughts and behaviour, as well as feelings of depression and hopelessness, among adults.
Evidence from people with lived experience shows safety planning helps people to understand their warning signs and practice coping strategies.
Sharing your safety plan with loved ones may help understand warning signs of a crisis. Dragana Gordic/Shutterstock Are there helplines I can call?
There are people ready to listen, by phone or online chat, Australia-wide. You can try any of the following (most are available 24 hours a day, seven days a week):
Suicide helplines:
- Lifeline 13 11 14
- Suicide Call Back Service 1300 659 467
There is also specialised support:
- for men: MensLine Australia 1300 78 99 78
- children and young people: Kids’ Helpline 1800 55 1800
- Aboriginal and Torres Strait Islander people: 13YARN 13 92 76
- veterans and their families: Open Arms 1800 011 046
- LGBTQIA+ community: QLife 1300 184 527
- new and expecting parents: PANDA 1300 726 306
- people experiencing eating disorders: Butterfly Foundation 1800 33 4673.
Additionally, each state and territory will have its own list of mental health resources.
With uncertain access to services, it’s helpful to remember that there are people who care. You don’t have to go it alone.
Monika Ferguson, Senior Lecturer in Mental Health, University of South Australia and Nicholas Procter, Professor and Chair: Mental Health Nursing, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Why are tall people more likely to get cancer? What we know, don’t know and suspect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People who are taller are at greater risk of developing cancer. The World Cancer Research Fund reports there is strong evidence taller people have a higher chance of of developing cancer of the:
- pancreas
- large bowel
- uterus (endometrium)
- ovary
- prostate
- kidney
- skin (melanoma) and
- breast (pre- and post-menopausal).
But why? Here’s what we know, don’t know and suspect.
Pexels/Andrea Piacquadio Height does increase your cancer risk – but only by a very small amount. Christian Vinces/Shutterstock A well established pattern
The UK Million Women Study found that for 15 of the 17 cancers they investigated, the taller you are the more likely you are to have them.
It found that overall, each ten-centimetre increase in height increased the risk of developing a cancer by about 16%. A similar increase has been found in men.
Let’s put that in perspective. If about 45 in every 10,000 women of average height (about 165 centimetres) develop cancer each year, then about 52 in each 10,000 women who are 175 centimetres tall would get cancer. That’s only an extra seven cancers.
So, it’s actually a pretty small increase in risk.
Another study found 22 of 23 cancers occurred more commonly in taller than in shorter people.
Why?
The relationship between height and cancer risk occurs across ethnicities and income levels, as well as in studies that have looked at genes that predict height.
These results suggest there is a biological reason for the link between cancer and height.
While it is not completely clear why, there are a couple of strong theories.
The first is linked to the fact a taller person will have more cells. For example, a tall person probably has a longer large bowel with more cells and thus more entries in the large bowel cancer lottery than a shorter person.
Scientists think cancer develops through an accumulation of damage to genes that can occur in a cell when it divides to create new cells.
The more times a cell divides, the more likely it is that genetic damage will occur and be passed onto the new cells.
The more damage that accumulates, the more likely it is that a cancer will develop.
A person with more cells in their body will have more cell divisions and thus potentially more chance that a cancer will develop in one of them.
Some research supports the idea having more cells is the reason tall people develop cancer more and may explain to some extent why men are more likely to get cancer than women (because they are, on average, taller than women).
However, it’s not clear height is related to the size of all organs (for example, do taller women have bigger breasts or bigger ovaries?).
One study tried to assess this. It found that while organ mass explained the height-cancer relationship in eight of 15 cancers assessed, there were seven others where organ mass did not explain the relationship with height.
It is worth noting this study was quite limited by the amount of data they had on organ mass.
Is it because tall people have more cells? Halfpoint/Shutterstock Another theory is that there is a common factor that makes people taller as well as increasing their cancer risk.
One possibility is a hormone called insulin-like growth factor 1 (IGF-1). This hormone helps children grow and then continues to have an important role in driving cell growth and cell division in adults.
This is an important function. Our bodies need to produce new cells when old ones are damaged or get old. Think of all the skin cells that come off when you use a good body scrub. Those cells need to be replaced so our skin doesn’t wear out.
However, we can get too much of a good thing. Some studies have found people who have higher IGF-1 levels than average have a higher risk of developing breast or prostate cancer.
But again, this has not been a consistent finding for all cancer types.
It is likely that both explanations (more cells and more IGF-1) play a role.
But more research is needed to really understand why taller people get cancer and whether this information could be used to prevent or even treat cancers.
I’m tall. What should I do?
If you are more LeBron James than Lionel Messi when it comes to height, what can you do?
Firstly, remember height only increases cancer risk by a very small amount.
Secondly, there are many things all of us can do to reduce our cancer risk, and those things have a much, much greater effect on cancer risk than height.
We can take a look at our lifestyle. Try to:
- eat a healthy diet
- exercise regularly
- maintain a healthy weight
- be careful in the sun
- limit alcohol consumption.
And, most importantly, don’t smoke!
If we all did these things we could vastly reduce the amount of cancer.
You can also take part in cancer screening programs that help pick up cancers of the breast, cervix and bowel early so they can be treated successfully.
Finally, take heart! Research also tells us that being taller might just reduce your chance of having a heart attack or stroke.
Susan Jordan, Associate Professor of Epidemiology, The University of Queensland and Karen Tuesley, Postdoctoral Research Fellow, School of Public Health, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
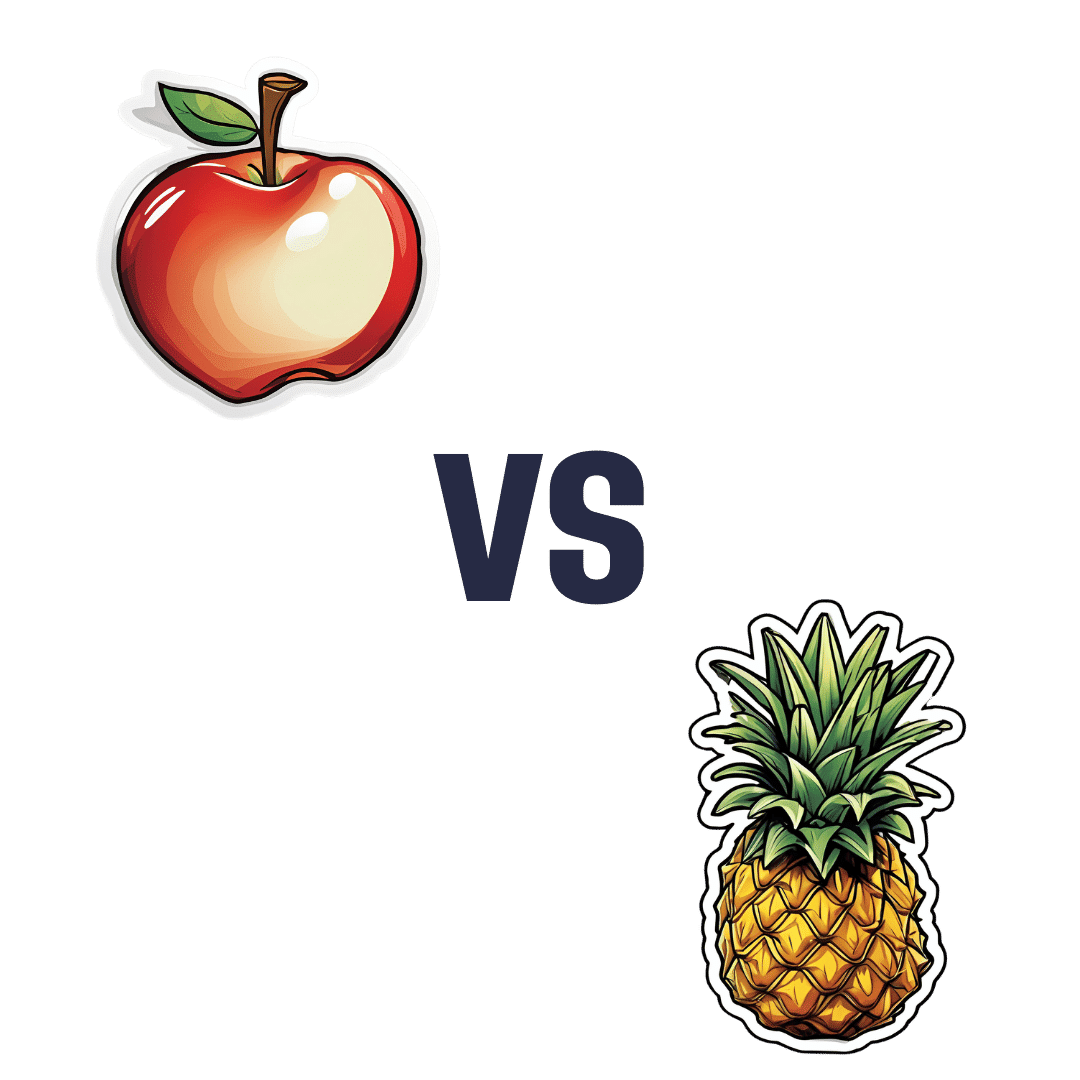
Apple vs Pineapple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apple to pineapple, we picked the pineapple.
Why?
An apple a day may keep the doctor away, but pineapples are heavier and armored and spiky and generally much more intimidating.
More seriously, apples are great but we say pineapples have the better nutritional and phytochemical properties overall:
In terms of macros, actually apples win this first round, albeit marginally; the two fruits are equal on carbs, while apple has a little more fiber and pineapple has a (very) little more protein. This makes the fiber content the deciding factor, so apples do win this one, even if by just 1g/100g difference.
When it comes to vitamins, however, apples have more of vitamins E and K, while pineapple has more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, and choline. The margins of difference are equally generous on both sides, so this is a clear and overwhelming win for pineapple (including 10x more vitamin C than apples, which are themselves considered a good source of vitamin C)
In the category of minerals, apples have slightly more phosphorus, and pineapple has a lot more calcium, copper, iron, magnesium, manganese, potassium, selenium, and zinc. Another easy win for pineapple.
Pineapples are not only also higher in polyphenols, but also contain bromelain, a powerful anti-inflammatory group of enzymes that are unique to pineapple—you can read about it in the link below!
Meanwhile, pineapple wins the day in our head-to-head here, but as ever when it comes to a plurality of healthy things, do enjoy either or both! Diversity is good.
Want to learn more?
You might like to read:
Bromelain vs Inflammation & Much More
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Life After Death? (Your Life; A Loved One’s Death)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Show Must Go On
We’ve previously written about the topics of death and dying. It’s not cheery, but it is important to tackle.
Sooner is better than later, in the case of:
Preparations For Managing Your Own Mortality
And for those who are left behind, of course it is hardest of all:
What Grief Does To Your Body (And How To Manage It)
But what about what comes next? For those who are left behind, that is.
Life goes on
In cases when the death is that of a close loved one, the early days after death can seem like a surreal blur. How can the world go ticking on as normal when [loved one] is dead?
But incontrovertibly, it does, so we can only ask again: how?
And, we get to choose that, to a degree. The above-linked article about grief gives a “101” rundown, but it’s (by necessity, for space) a scant preparation for one of the biggest challenges in life that most of us will ever face.
For many people, processing grief involves a kind of “saying goodbye”. For others, it doesn’t, as in the following cases of grieving the loss of one’s child—something no parent should ever have to face, but it happens:
Dr. Ken Druck | The Love That Never Dies
(with warning, the above article is a little heavy)
In short: for those who choose not to “say goodbye” in the case of the death of a loved one, it’s more often not a case of cold neglect, but rather the opposite—a holding on. Not in the “denial” sense of holding on, but rather in the sense of “I am not letting go of this feeling of love, no matter how much it might hurt to hold onto; it’s all I have”.
What about widows, and love after death?
Note: we’ll use the feminine “widow” here as a) it’s the most common and b) most scientific literature focuses on widows, but there is no reason why most of the same things won’t also apply to widowers.
We say “most”, as society does tend to treat widows and widowers differently, having different expectations about a respectful mourning period, one’s comportment during same, and so on.
As an aside: most scientific literature also assumes heterosexuality, which is again statistically reasonable, and for the mostpart the main difference is any extra challenges presented by non-recognition of marriages, and/or homophobic in-laws. But otherwise, grief is grief, and as the saying goes, love is love.
One last specificity before we get into the meat of this: we are generally assuming marriages to be monogamous here. Polyamorous arrangements will likely sidestep most of these issues completely, but again, they’re not the norm.
Firstly, there’s a big difference between remarrying (or similar) after being widowed, and remarrying (or similar) after a divorce, and that largely lies in the difference of how they begin. A divorce is (however stressful it may often be) more often seen as a transition into a new period of freedom, whereas bereavement is almost always felt as a terrible loss.
The science, by the way, shows the stats for this; people are less likely to remarry, and slower to remarry if they do, in instances of bereavement rather than divorce, for example:
Timing of Remarriage Among Divorced and Widowed Parents
Love after death: the options
For widows, then, there seem to be multiple options:
- Hold on to the feelings for one’s deceased partner; never remarry
- Grieve, move on, find new love, relegating the old to history
- Try to balance the two (this is tricky but can be done*)
*Why is balancing the two tricky, and how can it be done?
It’s tricky because ultimately there are three people’s wishes at hand:
- The deceased (“they would want me to be happy” vs “I feel I would be betraying them”—which two feelings can also absolutely come together, by the way)
- Yourself (whether you actually want to get a new partner, or just remain single—this is your 100% your choice either way, and your decision should be made consciously)
- The new love (how comfortable are they with your continued feelings for your late love, really?)
And obviously only two of the above can be polled for opinions, and the latter one might say what they think we want to hear, only to secretly and/or later resent it.
One piece of solid advice for the happily married: talk with your partner now about how you each would feel about the other potentially remarrying in the event of your death. Do they have your pre-emptive blessing to do whatever, do you ask a respectable mourning period first (how long?), would the thought just plain make you jealous? Be honest, and bid your partner be honest too.
One piece of solid advice for everyone: make sure you, and your partner(s), as applicable, have a good emotional safety net, if you can. Close friends or family members that you genuinely completely trust to be there through thick and thin, to hold your/their hand through the emotional wreck that will likely follow.
Because, while depression and social loneliness are expected and looked out for, it’s emotional loneliness that actually hits the hardest, for most people:
Longitudinal Examination of Emotional Functioning in Older Adults After Spousal Bereavement
…which means that having even just one close friend or family member with whom one can be at one’s absolute worst, express emotions without censure, not have to put on the socially expected appearance of emotional stability… Having that one person (ideally more, but having at least one is critical) can make a huge difference.
But what if a person has nobody?
That’s definitely a hard place to be, but here’s a good starting point:
How To Beat Loneliness & Isolation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mosquitoes can spread the flesh-eating Buruli ulcer. Here’s how you can protect yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Each year, more and more Victorians become sick with a flesh-eating bacteria known as Buruli ulcer. Last year, 363 people presented with the infection, the highest number since 2004.
But it has been unclear exactly how it spreads, until now. New research shows mosquitoes are infected from biting possums that carry the bacteria. Mozzies spread it to humans through their bite.
What is Buruli ulcer?
Buruli ulcer, also known as Bairnsdale ulcer, is a skin infection caused by the bacterium Mycobacterium ulcerans.
It starts off like a small mosquito bite and over many months, slowly develops into an ulcer, with extensive destruction of the underlying tissue.
While often painless initially, the infection can become very serious. If left untreated, the ulcer can continue to enlarge. This is where it gets its “flesh-eating” name.
Thankfully, it’s treatable. A six to eight week course of specific antibiotics is an effective treatment, sometimes supported with surgery to remove the infected tissue.
Where can you catch it?
The World Health Organization considers Buruli ulcer a neglected tropical skin disease. Cases have been reported across 33 countries, primarily in west and central Africa.
However, since the early 2000s, Buruli ulcer has also been increasingly recorded in coastal Victoria, including suburbs around Melbourne and Geelong.
Scientists have long known Australian native possums were partly responsible for its spread, and suspected mosquitoes also played a role in the increase in cases. New research confirms this.
Our efforts to ‘beat Buruli’
Confirming the role of insects in outbreaks of an infectious disease is achieved by building up corroborating, independent evidence.
In this new research, published in Nature Microbiology, the team (including co-authors Tim Stinear, Stacey Lynch and Peter Mee) conducted extensive surveys across a 350 km² area of Victoria.
We collected mosquitoes and analysed the specimens to determine whether they were carrying the pathogen, and links to infected possums and people. It was like contact tracing for mosquitoes.
Aedes notoscriptus was the mosquito identified as carrying the bacteria that caused Buruli ulcer.
Cameron Webb (NSW Health Pathology)Molecular testing of the mosquito specimens showed that of the two most abundant mosquito species, only Aedes notoscriptus (a widespread species commonly known as the Australian backyard mosquito) was positive for Mycobacterium ulcerans.
We then used genomic tests to show the bacteria found on these mosquitoes matched the bacteria in possum poo and humans with Buruli ulcer.
We further analysed mosquito specimens that contained blood to show Aedes notoscriptus was feeding on both possums and humans.
To then link everything together, geospatial analysis revealed the areas where human Buruli ulcer cases occur overlap with areas where both mosquitoes and possums that harbour Mycobacterium ulcerans are active.
Stop its spread by stopping mozzies breeding
The mosquito in this study primarily responsible for the bacteria’s spread is Aedes notoscriptus, a mosquito that lays its eggs around water in containers in backyard habitats.
Controlling “backyard” mosquitoes is a critical part of reducing the risk of many global mosquito-borne disease, especially dengue and now Buruli ulcer.
You can reduce places where water collects after rainfall, such as potted plant saucers, blocked gutters and drains, unscreened rainwater tanks, and a wide range of plastic buckets and other containers. These should all be either emptied at least weekly or, better yet, thrown away or placed under cover.
Mosquitoes can lay eggs in a wide range of water-filled items in the backyard.
Cameron Webb (NSW Health Pathology)There is a role for insecticides too. While residual insecticides applied to surfaces around the house and garden will reduce mosquito populations, they can also impact other, beneficial, insects. Judicious use of such sprays is recommended. But there are ecological safe insecticides that can be applied to water-filled containers (such as ornamental ponds, fountains, stormwater pits and so on).
Recent research also indicates new mosquito-control approaches that use mosquitoes themselves to spread insecticides may soon be available.
How to protect yourself from bites
The first line of defence will remain personal protection measures against mosquito bites.
Covering up with loose fitted long sleeved shirts, long pants, and covered shoes will provide physical protection from mosquitoes.
Applying topical insect repellent to all exposed areas of skin has been proven to provide safe and effective protection from mosquito bites. Repellents should include diethytolumide (DEET), picaridin or oil of lemon eucalyptus.
While the rise in Buruli ulcer is a significant health concern, so too are many other mosquito-borne diseases. The steps to avoid mosquito bites and exposure to Mycobacteriam ulcerans will also protect against viruses such as Ross River, Barmah Forest, Japanese encephalitis, and Murray Valley encephalitis.
Cameron Webb, Clinical Associate Professor and Principal Hospital Scientist, University of Sydney; Peter Mee, Adjunct Associate Lecturer, School of Applied Systems Biology, La Trobe University; Stacey Lynch, Team Leader- Mammalian infection disease research, CSIRO, and Tim Stinear, Professor of Microbiology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: